Anthem Claim Dispute Form With 2 Points In King
Description
Form popularity
FAQ
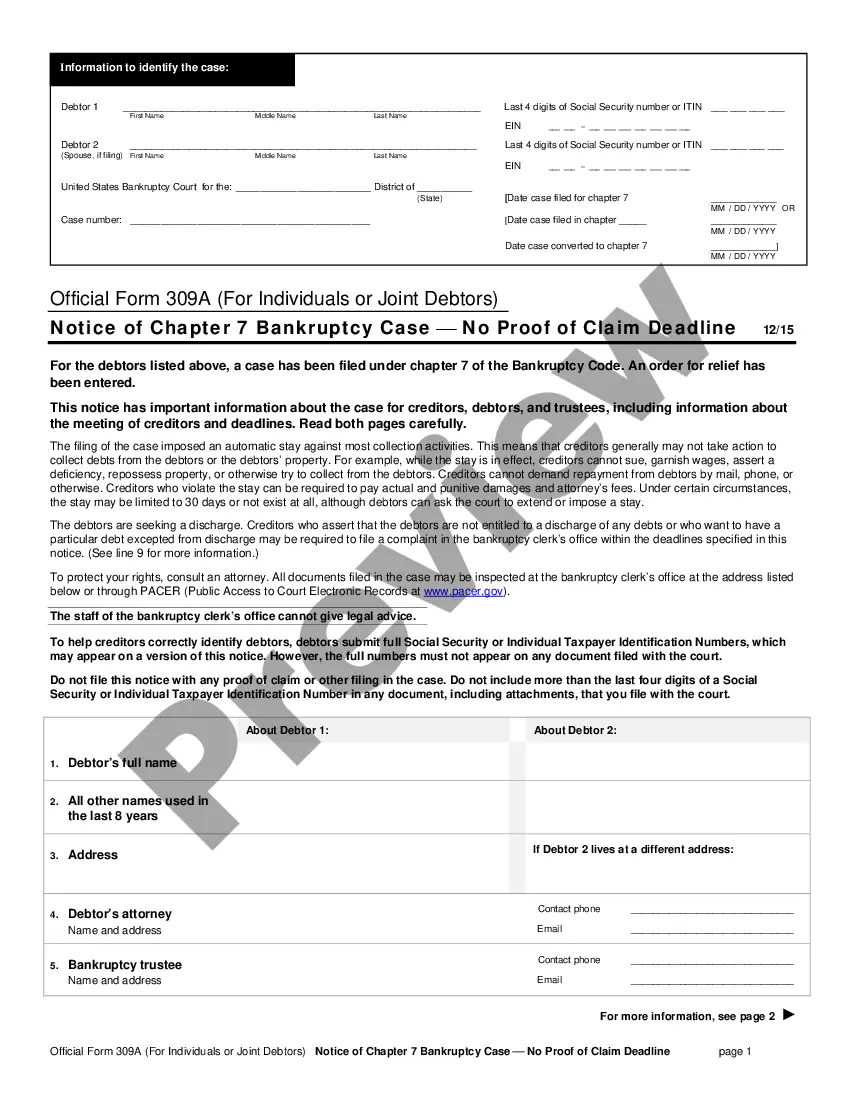
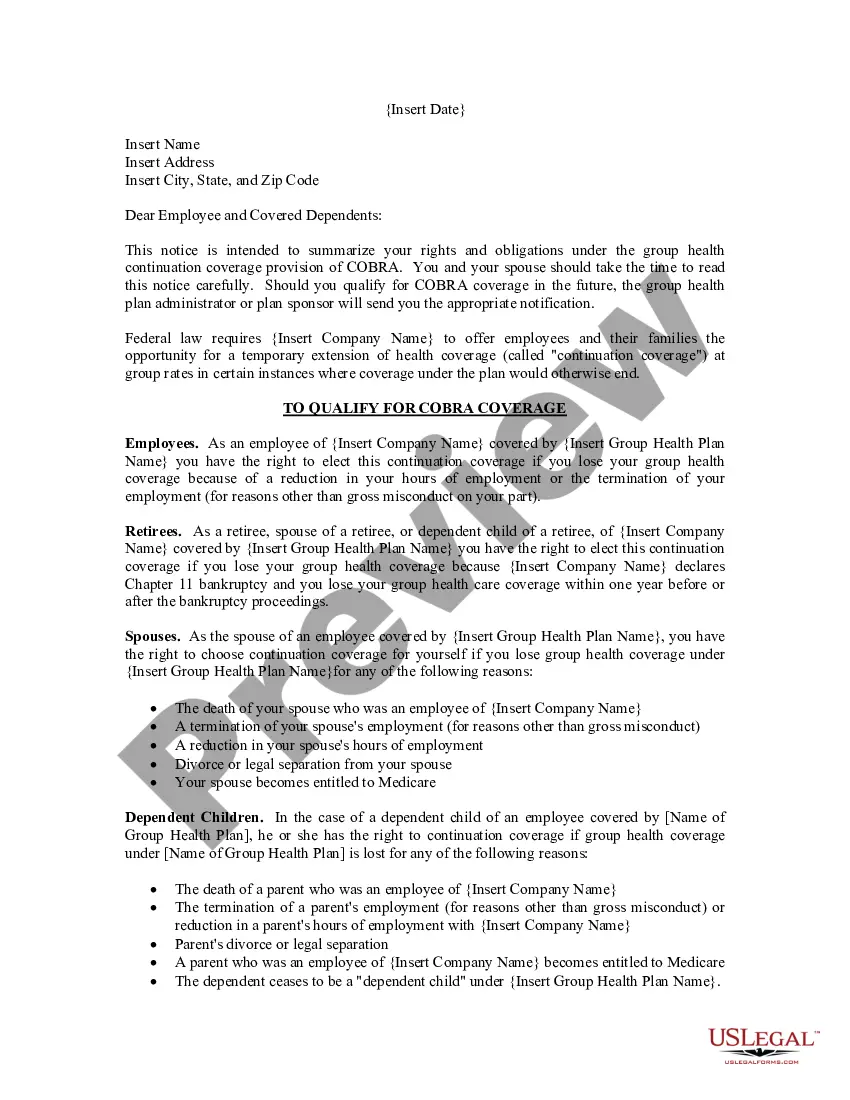
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
You need to file your appeal within 60 calendar days from the date on the coverage determination/organization determination notice (denial letter) you received.
If you think we have made a mistake in denying your medical service, or if you don't agree with our decision, you can ask for an appeal. You must do this within 60 calendar days from the date on the Notice of Action sent to you. We will resolve your concerns within 30 days of receiving your complaint.
Simply put, you can appeal if you think there is a logical and acceptable reason why the claim was false. It would probably be denied if there was no way to submit the claim within the time limit However, if you have a valid reason, this denial could get overturned, and your claim might be accepted.
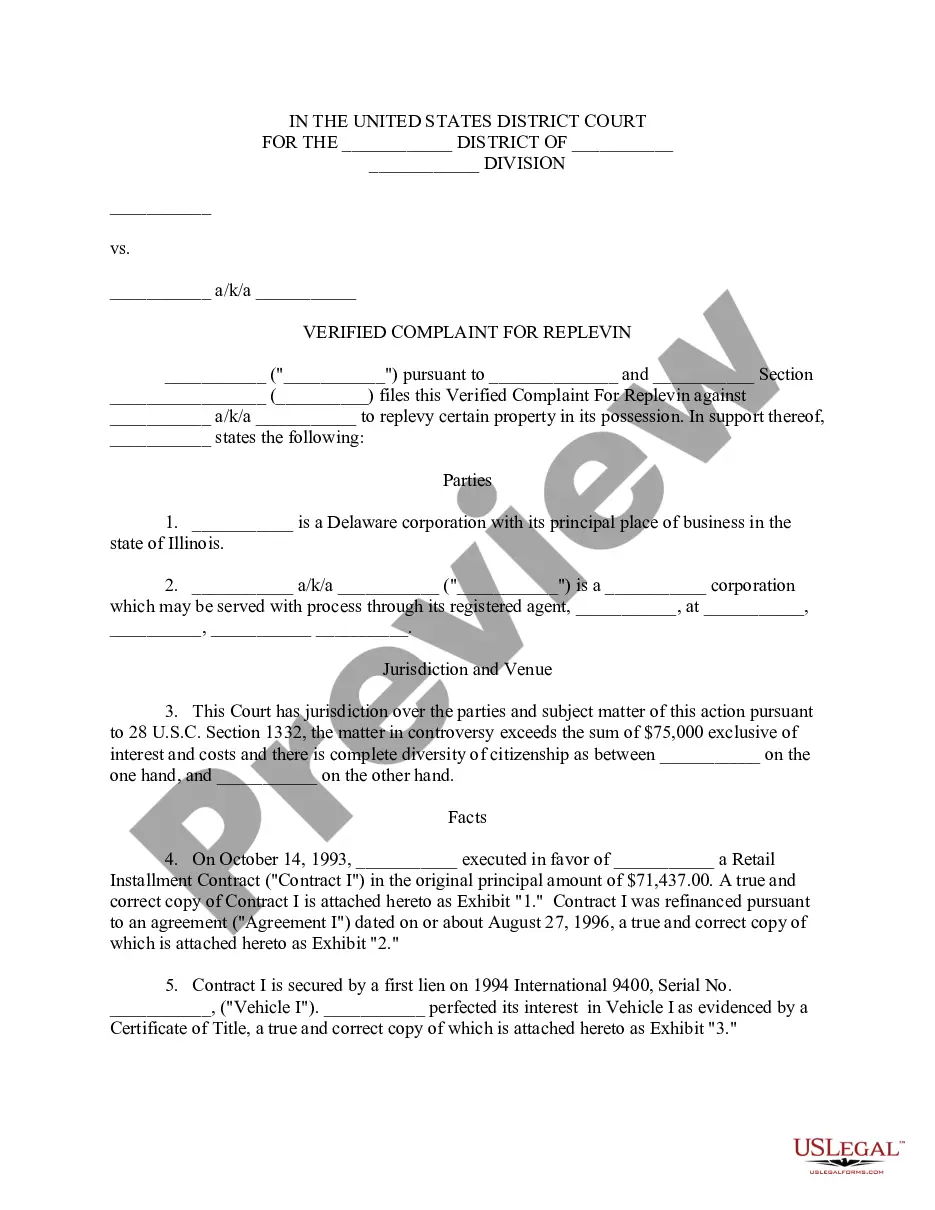
How to Find Timely Filing Limits With Insurance Insurance CompanyTimely Filing Limit (From the date of service) Anthem BCBS Ohio, Kentucky, Indiana, Wisconsin 90 Days Wellmark BCBS Iowa and South Dakota 180 Days BCBS Alabama 2 Years BCBS Arkansas 180 Days28 more rows
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
Original (or initial) Medi-Cal claims must be received by the California MMIS FI within six months following the month in which services were rendered. This requirement is referred to as the six-month billing limit.
Anthem follows the standard of: • 180 days for participating providers and facilities. 210 days for nonparticipating providers and facilities. Timely filing is determined by subtracting the date of service from the date we receive the claim and comparing the number of days to the applicable federal or state mandate.
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.