Here Denied Claim For Medical Necessity In Fulton
Description
Form popularity
FAQ
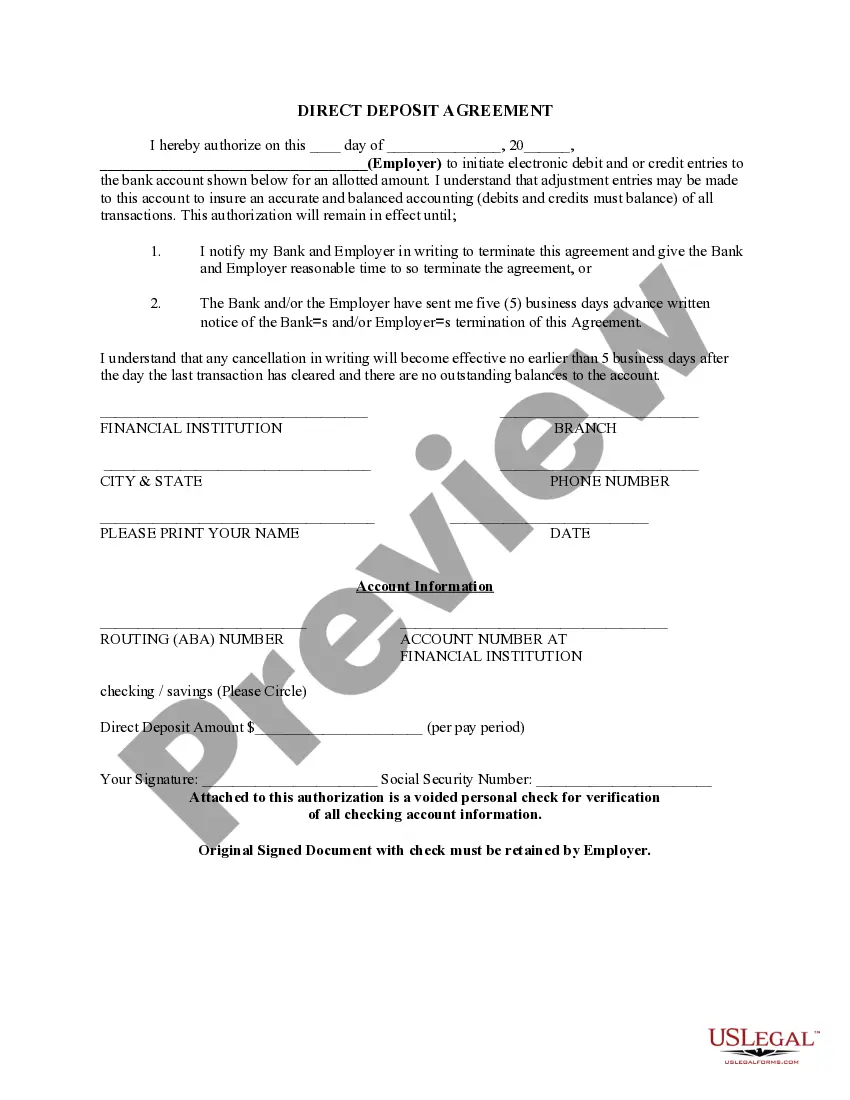
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
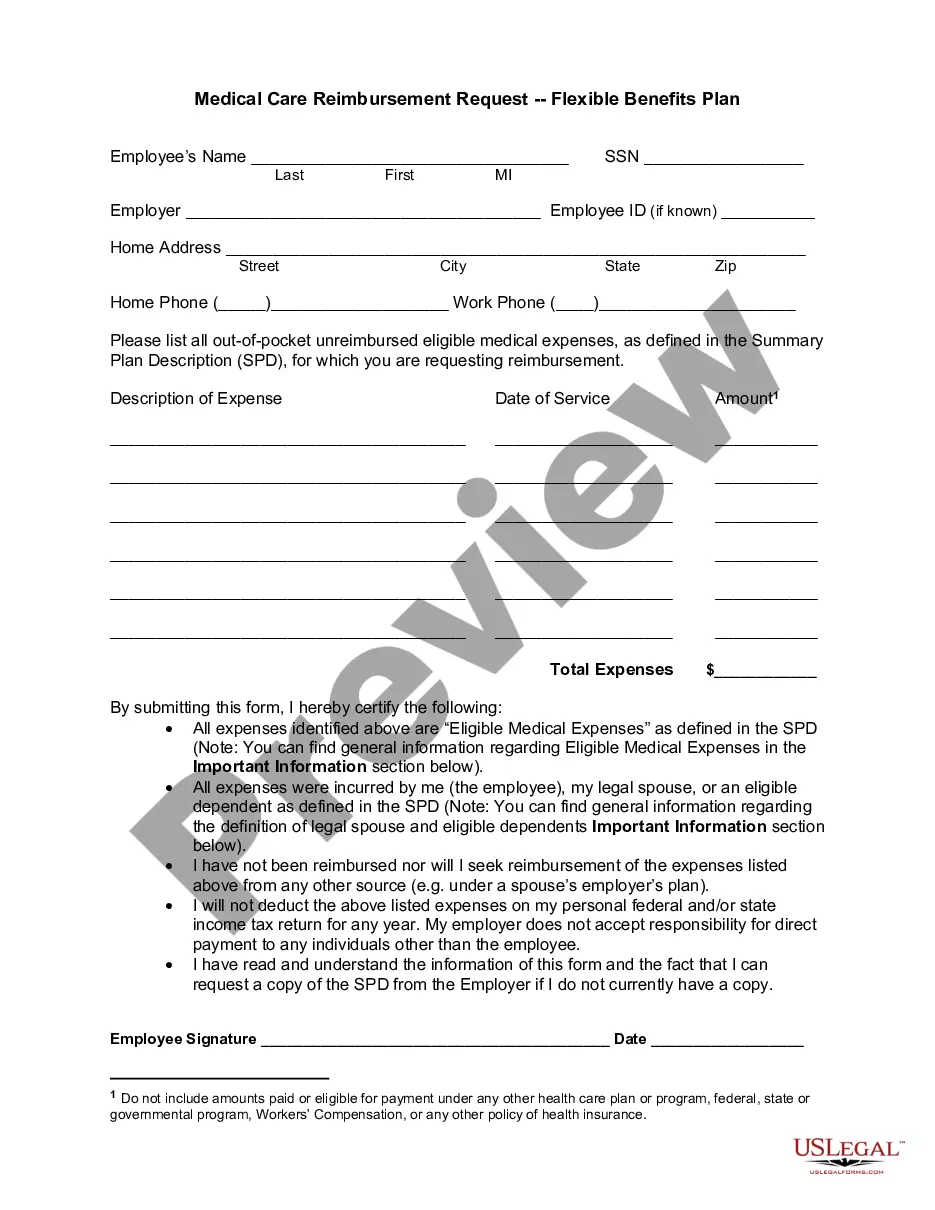
Denial code 151 is used when the payer determines that the information provided does not justify the number or frequency of services billed. In other words, the payer believes that the documentation or evidence submitted does not support the need for the amount or frequency of services claimed for reimbursement.
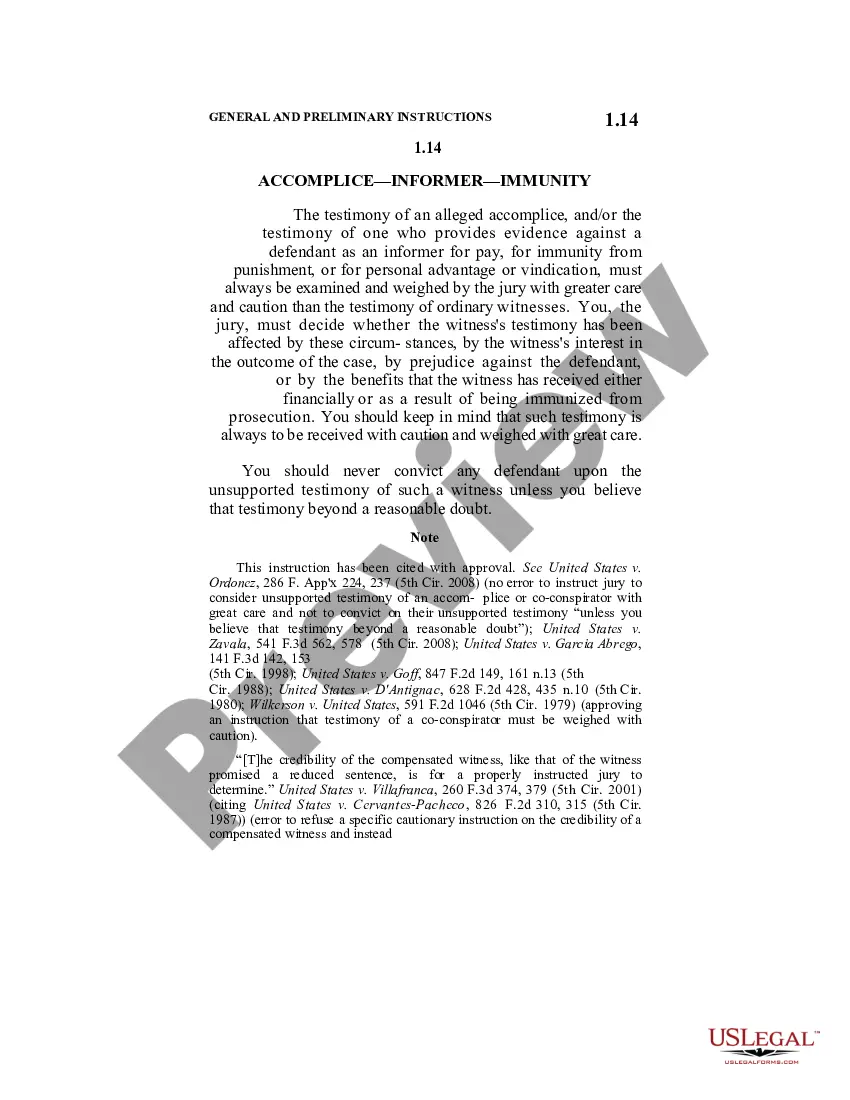
Medical Necessity Denials: Appeals Review the definition of “Medical Necessity” in your provider contract. Review the patient's medical records, including surgical reports. Call the health plan to discuss the denial with the designated reviewer.
Be persistent Your appeal should include an explanation of your reconsideration request, along with any necessary supporting documentation, such as a copy of the claim in question and copies of earlier communication to the company about the matter.
Denial code 256 is when a healthcare provider's service is not covered by a managed care contract, resulting in non-payment.
Denial code 167 means the diagnosis is not covered. Check the 835 Healthcare Policy Identification Segment for more information.
This denial code indicates that the necessary supporting documentation or information was not included with the claim, leading to its denial.
Denial code 50 is used when the payer determines that the services provided are not considered a 'medical necessity'. This means that the payer does not believe that the services are essential for the patient's diagnosis or treatment.
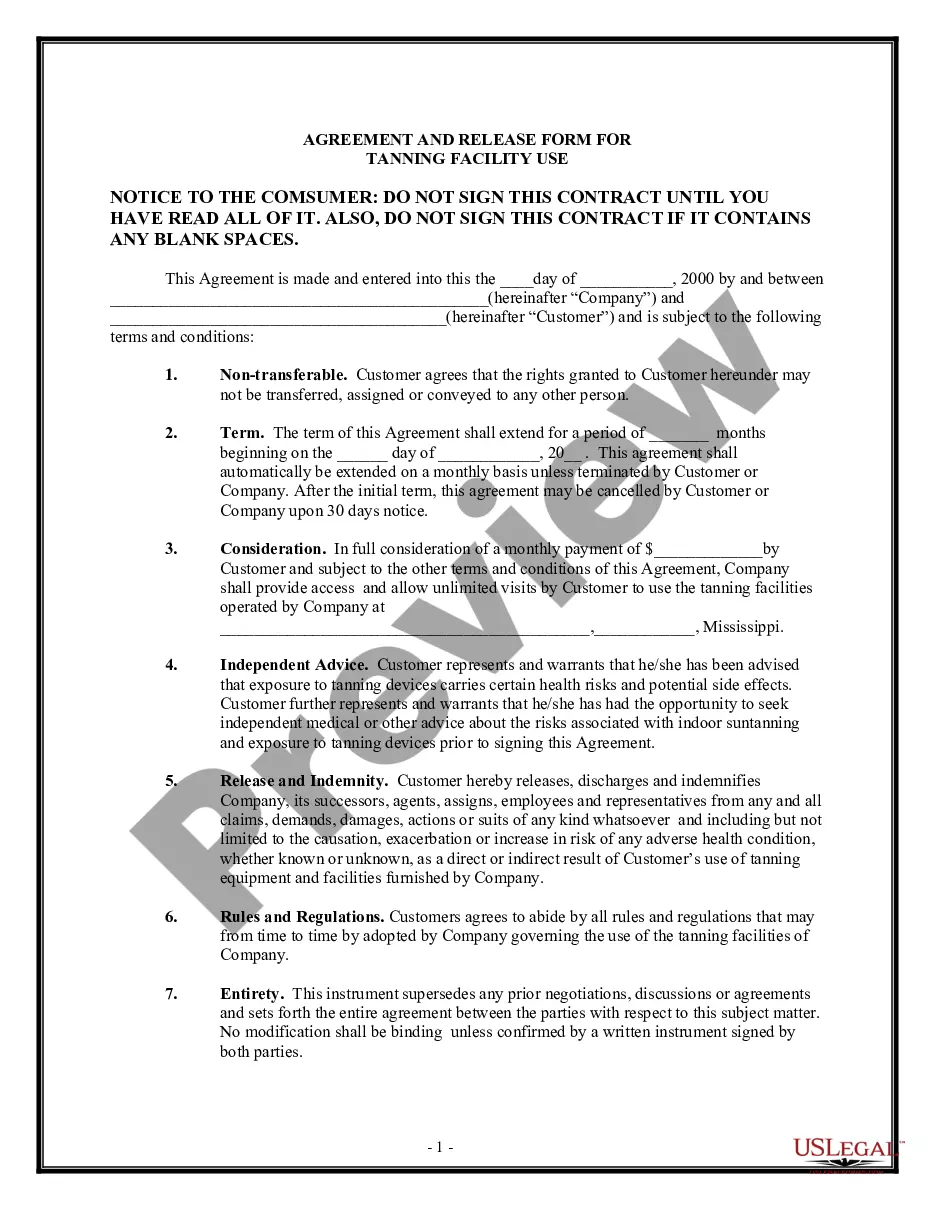
Plans only cover health care they determine is medically necessary. Examples of services or treatments a plan may define as not medically necessary include cosmetic procedures, treatments that haven't been proven effective, and treatments more expensive than others that are also effective.