Anthem Claim Dispute Form With Decimals In Fulton
Description
Form popularity
FAQ
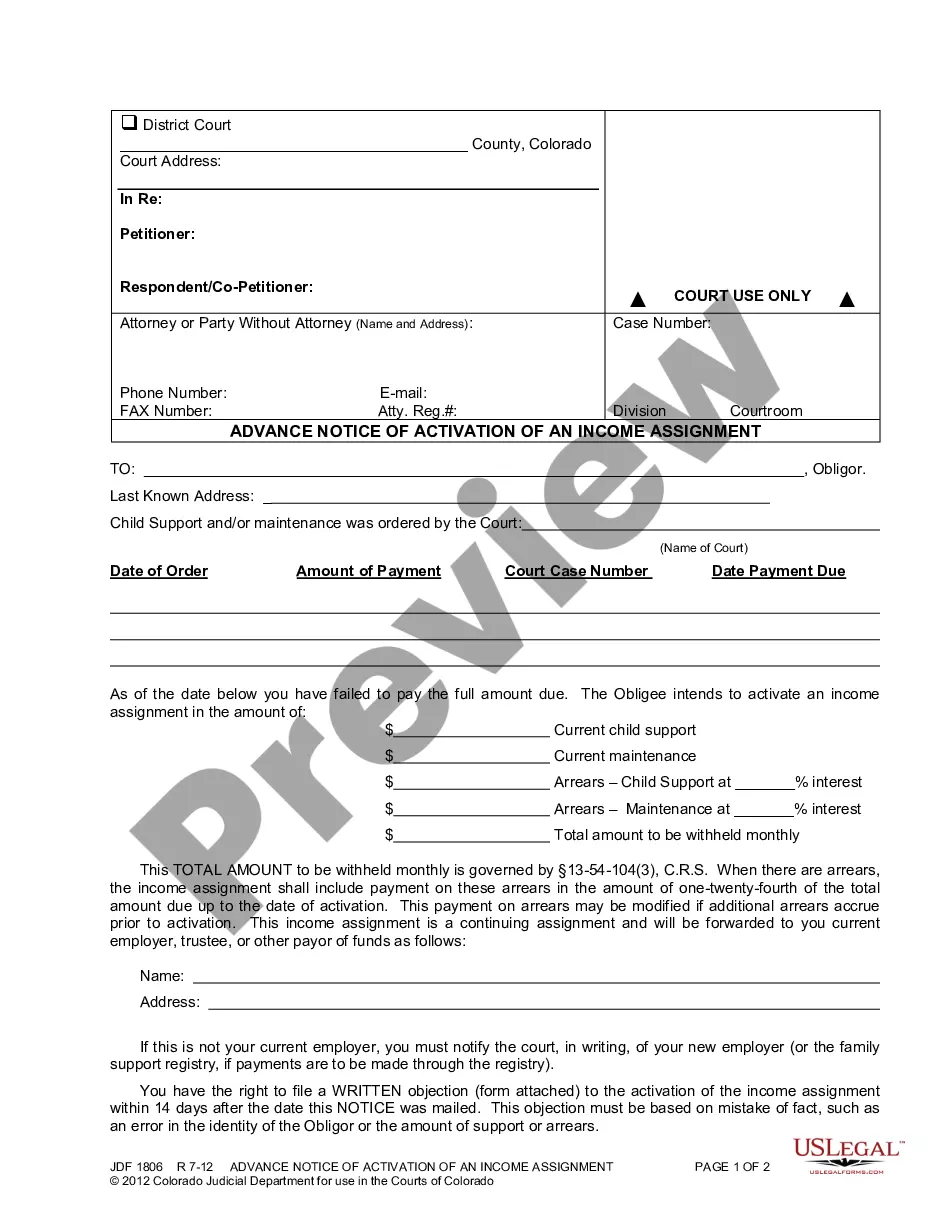
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
You can also fax to 855-516-1083. Please be sure to mark "EXPEDITED" on the form before faxing.
One redetermination form can be submitted for multiple claims only for denials by the Unified Program Integrity Contractor or Medical Review probe reviews. Fax request to 1-888-541-3829.
File the appeal within ten (10) days from the date your "Determination of Eligibility" was sent by one of these methods: Mail the appeal to 10 North Senate Avenue, Indianapolis, IN 46204; Fax the appeal to (317) 233-6888; Deliver the appeal in person to the Department at 10 N.
Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
Please fax to 1-855-516-1083. You may ask us to rush your appeal if your health needs it. We'll let you know we got your appeal within 24 hours from the time we received it.
After you fill out the form, Mail/Fax/deliver your request for a hearing within 33 days of the date of the notice you are appealing. Mail: FSSA Document Center PO Box 1810 Marion, Indiana 46952 Fax: 1-800-403-0864 Visit your local DFR/Medicaid Office.
Customer Care Centers Call 888-831-2246 Option 4 and ask to speak with Dr.
How to Find Timely Filing Limits With Insurance Insurance CompanyTimely Filing Limit (From the date of service) Anthem California 90 Days BCBS Illinois 180 Days Beacon Health 90 Days Blue Cross of California 180 Days28 more rows
You may submit a grievance to Blue Shield by calling (800) 393-6130, going online at blueshieldca, or by mailing your written grievance to Blue Shield of California, Appeals and Grievances Dept, P.O. Box 5588, El Dorado Hills, CA 95762.