Anthem Claim Dispute Form For Reimbursement In Cuyahoga
Description
Form popularity
FAQ
Anthem and Blue Cross Blue Shield are related, but they are not the same company. While they are both top health insurance providers in the USA, the big difference is that Blue Cross Blue Shield is the umbrella that is made up of several independent companies, and one of these smaller companies is Anthem.
If you need help, call us at 844-912-0938 (TTY 711).
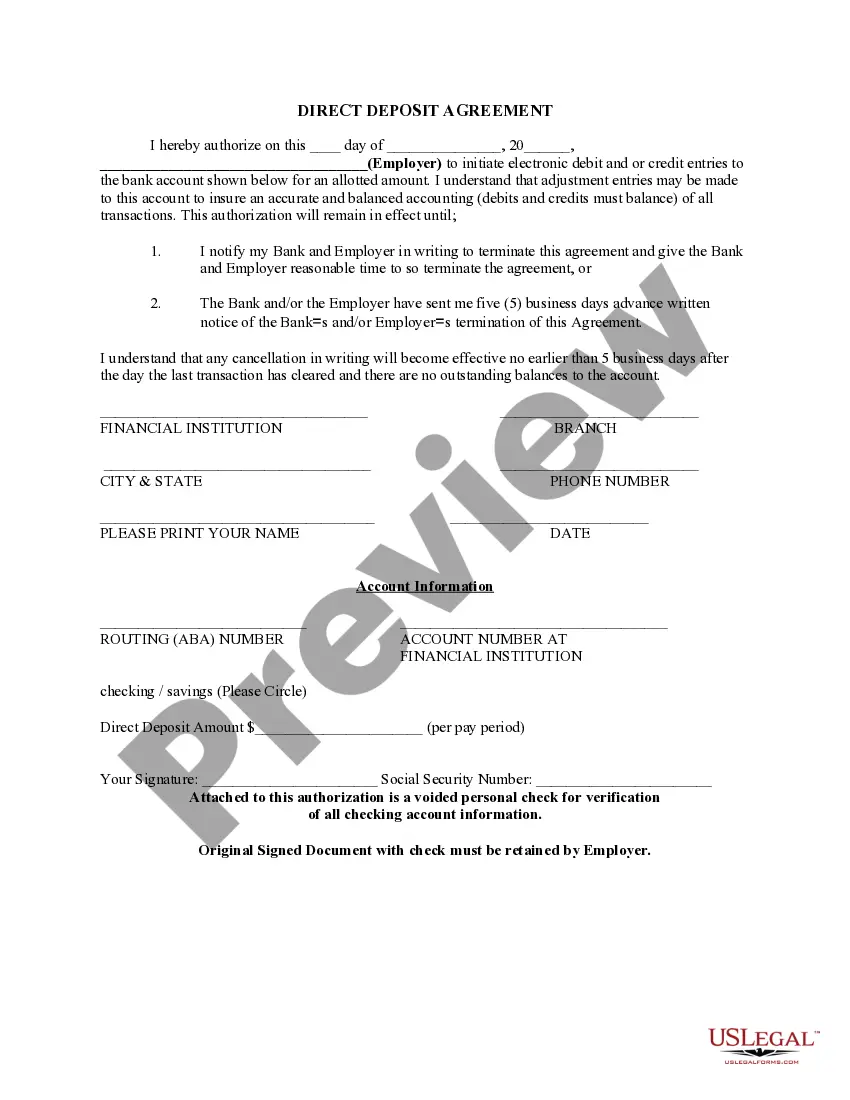
Participating providers, all claims including secondary claims, should be submitted within 90 calendar days from the date of service. Non- participating providers, all claims should be submitted within 90 calendar days from the date of service.
Effective for dates of service on or after July 1, 2020, provider claims must be submitted within 365 calendar days from the date of service or discharge. Providers also have 365 calendar days from the date of service or discharge to submit a corrected claim.
Anthem will consider reimbursement for the initial claim, when received and accepted within timely filing requirements, in compliance with federal, and/or state mandates. Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
How long do I have to submit an appeal? Consideration will not be given to appeals received greater than 180 days from the claim adjudication/denial date.
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.
Shopping Assistance Individual & Family Plans (under age 65): 1-844-290-7584. Medicare Supplement and Medicare Advantage Plans: 4/1 – 9/30: Mon-Fri, 8 a.m. to 8 p.m. Medicare Part D Plans: 4/1 – 9/30: Mon-Fri, 8 a.m. to 8 p.m. Employer Plan: Contact your broker or consultant to learn more about Anthem plans.
BLUE CROSS & BLUE SHIELD OF OHIO is a not-for-profit mutual insurance company and an Independent Licensee of the Blue Cross and Blue Shield Assn. The state's oldest and largest health insurer, by 1995 it served more than 1.6 million Ohioans.