Anthem Claim Dispute Form With 2 Points In Collin
Description
Form popularity
FAQ
Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
Set the billing frequency to either Replacement of Prior Claim or Void/Cancel of Prior Claim in the Claim Information section (for professional and facility claims). You will use Replacement of Prior Claim if the claim has been processed and Void/Cancel of Prior Claim if the claim is still in processing.
Is Anthem the same as Blue Cross Blue Shield? Anthem is part of the Blue Cross Blue Shield group. Blue Cross Blue Shield is made up of independent companies. Anthem is one of these companies.
Log into Availity Essentials. Select Claims & Payments from the navigation menu, then choose Claim Status. Search and locate the claim using the Member or Claim Number options. On the Claim Status results page, select Dispute Claim (if offered and applicable)
Claims dispute From the Availity homepage, select Claims & Payments from the top navigation. Select Claim Status Inquiry from the drop-down menu. Submit an inquiry and review the Claims Status Detail page. If the claim is denied or final, there will be an option to dispute the claim.
To use the Appeals application, the Availity administrator must assign the Claim Status role for the user. The Disputes and Appeals functionality will support Appeals, Reconsiderations and Rework requests for providers. The Disputes and Appeals functionality is accessible from the Claim Status transaction.
If you think we have made a mistake in denying your medical service, or if you don't agree with our decision, you can ask for an appeal. You must do this within 60 calendar days from the date on the Notice of Action sent to you. We will resolve your concerns within 30 days of receiving your complaint.
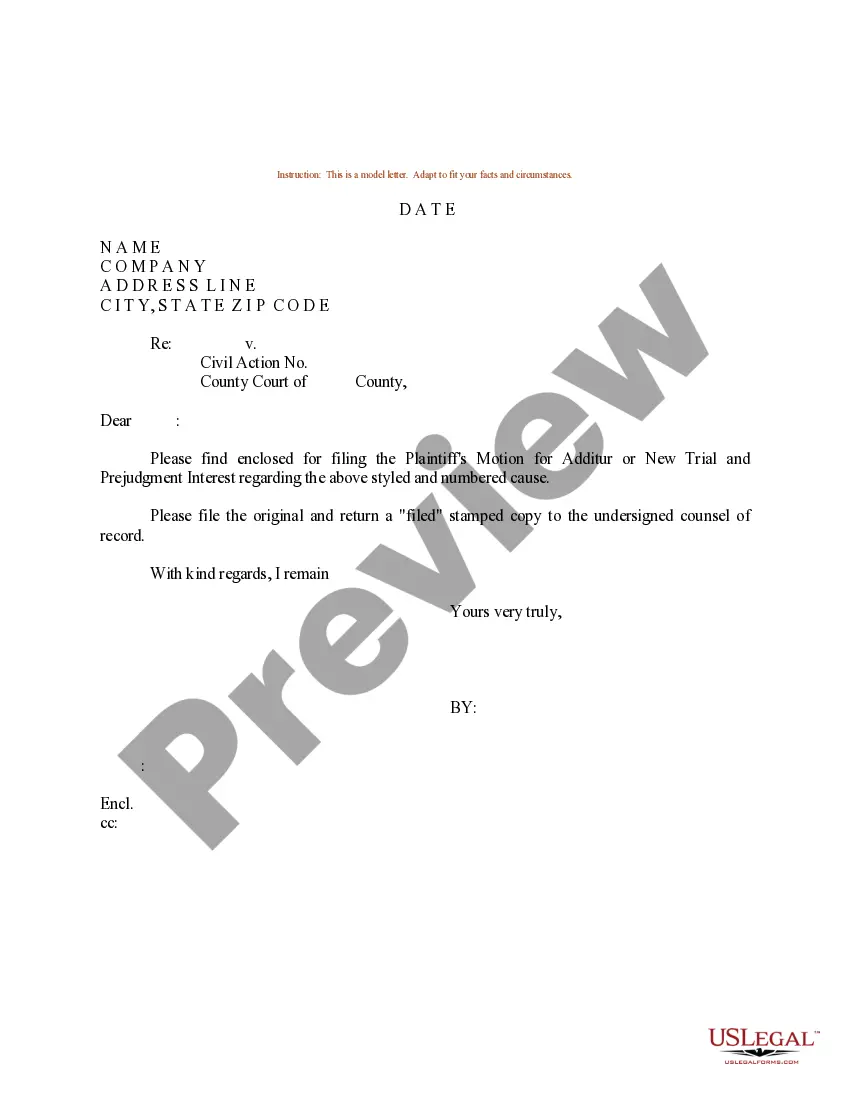
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
Claim forms are available by logging into the member website at blueshieldca or by contacting the benefit administrator. Please submit your claim form and medical records within one year of the service date.