Letter For Overpayment In Queens
Description
Form popularity
FAQ
Payments Log in to myEDD. Select Benefit Overpayment Services. Select Make a Payment. Select payment method type (such as ACH Debit). Complete the required fields, then select Submit.
If you have not received the back payments after 3 weeks, you can let us know by calling us at 888-209-6851. If you cannot reach us by phone you can send a message through the secure messaging system in your online account.
To be considered for a waiver, you must complete and return the Personal Financial Statement (DE 1446). We will review your information to determine if repaying the overpayment would cause you extraordinary hardship. To learn how we determine if you qualify for a waiver, visit Benefit Overpayment FAQs.
You have the right to appeal an overpayment determination. You must submit your appeal in writing within 30 days of the mailing date on the Notice of Overpayment (DE 1444). You can still submit an appeal after the 30-day deadline, but you must provide the reasons why you missed the appeal deadline.
To reopen your claim, simply start claiming weekly benefits again. You may receive a form in the mail about the period of time for which you did not claim benefits. This is called “Break in Claim” form.
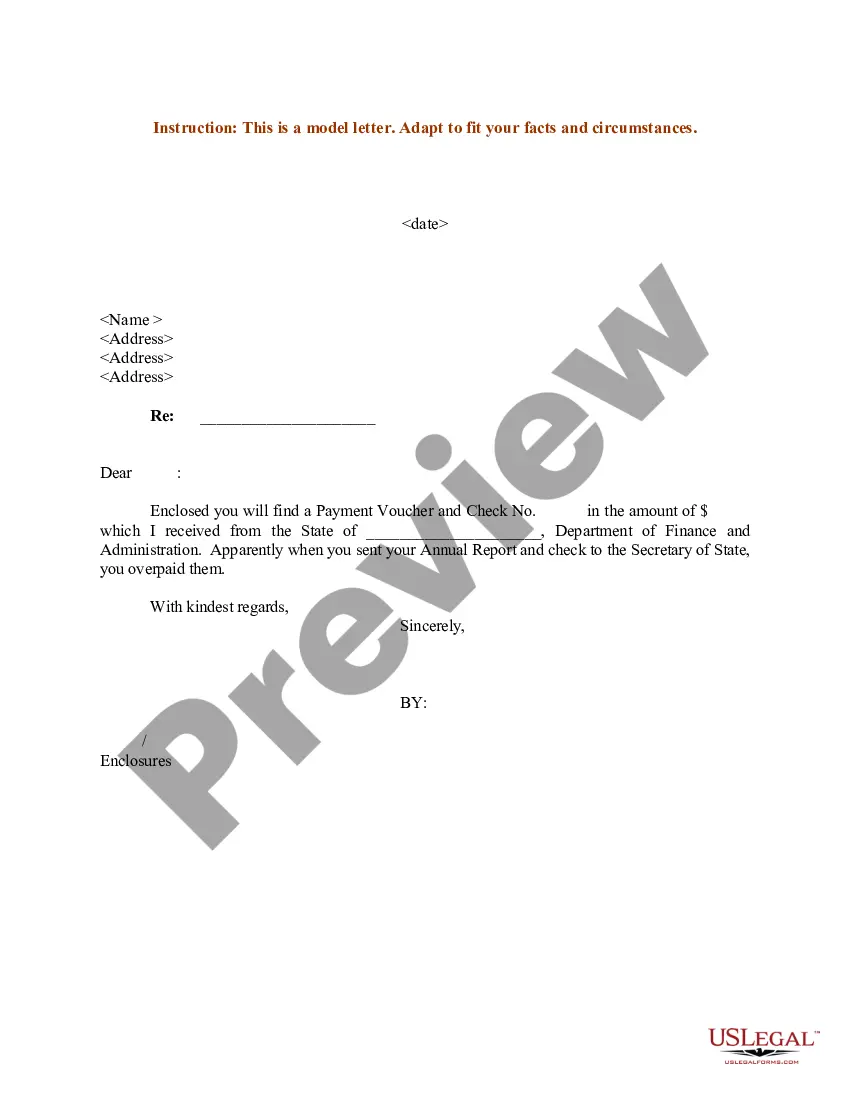
An overpayment letter is a formal request to repay a debt owed to the Medicare Trust Fund. Payment is due upon receipt of the notice. Send the payment with a copy of the overpayment letter received or request an immediate offset.
Remember, every time you certify for weekly benefits, you must provide accurate information about any: • work you perform, • work you refused, and • change in your availability for work. WHAT HAPPENS IF I RETURN TO WORK AND THEN I AM DIAGNOSED WITH COVID-19?
You were overpaid in error because <REASON>. Please contact me at <AGENCY PAYROLL OFFICER TELEPHONE NUMBER> to discuss your method of repayment by <FOUR CALENDAR DAYS FROM ABOVE DATE>. Failure to respond timely will result in the immediate recovery of the overpayment.