Severance Agreement Form With Cobra In New York
Description
Form popularity
FAQ
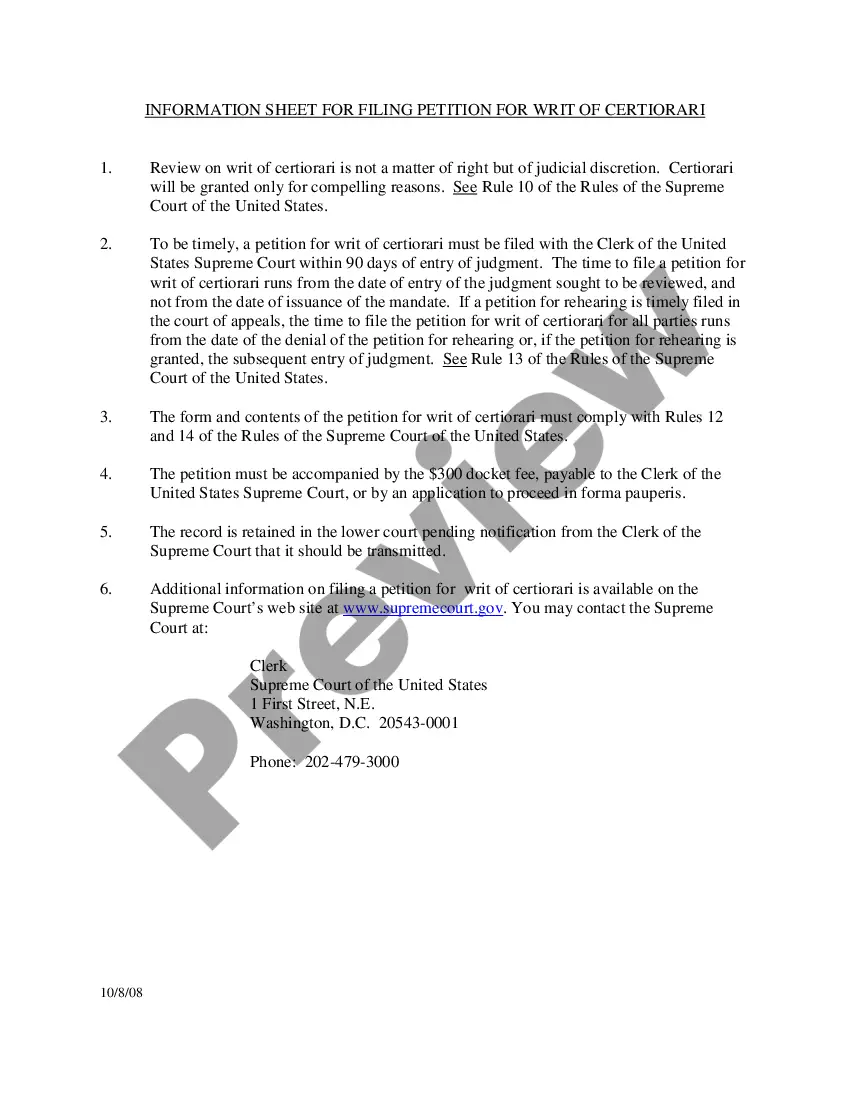
Understanding the 60-Day Loophole It's not so much of a loophole, but two 60-day windows of time to remember. You have a 60-day window following the end of your employer-sponsored plan to select COBRA coverage or choose a new plan in the individual ACA marketplace.
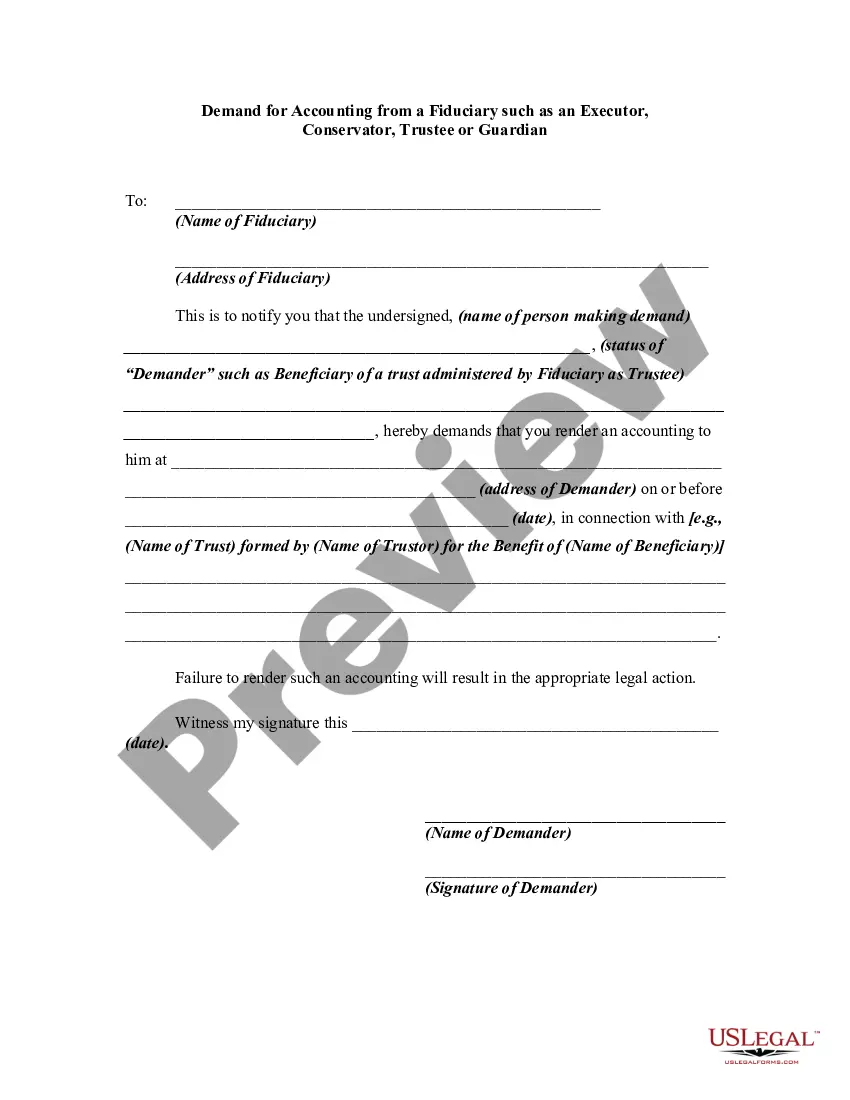
Required content and form The notice must explain the reason coverage has terminated, provide the date of termination and describe any rights the qualified beneficiary may have to elect alternative group or individual coverage, such as a conversion right (29 C.F.R. 2590.606-4(d)).
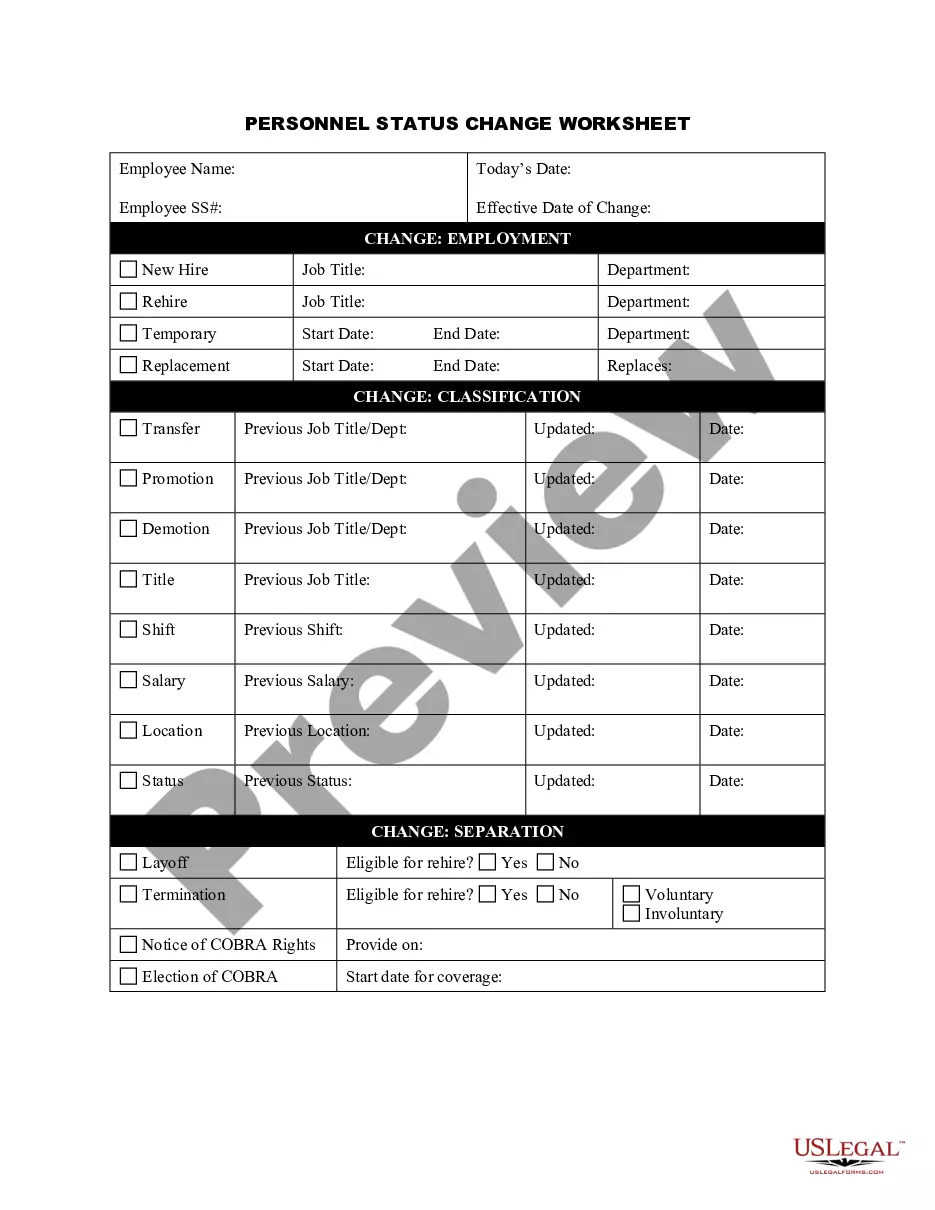
COBRA applies to most private sector businesses with 20 or more employees. It requires an employer's group health insurance plan to continue after qualifying life events. These include: Termination or a reduction of a covered employee's hours.
Qualified beneficiaries are eligible to continue health coverage under Federal COBRA for 18 months. Those who are eligible may continue coverage under New York State's continuation coverage for an additional 18 months, totaling 36 months of coverage when combining Federal COBRA benefits and NYS continuation benefits.
COBRA health insurance provides for the continuation of group health coverage when you quit, retire or are fired from a job that offered a qualifying plan. It can also be applied if your hours are reduced so that you no longer meet your employer's criteria for plan eligibility. The only exception is dismissal for gross.
When it's time to stop or cancel your coverage, you would need to make a request from the plan administrator to receive a letter of notice of COBRA termination. Typically, the COBRA Administrator is in the HR department or is a third-party administrator.
How to ask for a severance package Review your company's documents. You can typically find details of the company's policy regarding severance packages in a couple of places. Make note of your accomplishments. Stay professional. Negotiate severance during your job offer. Agree to an exit interview.