Corporate Refusal Form Dental In Wayne
Description
Form popularity
FAQ
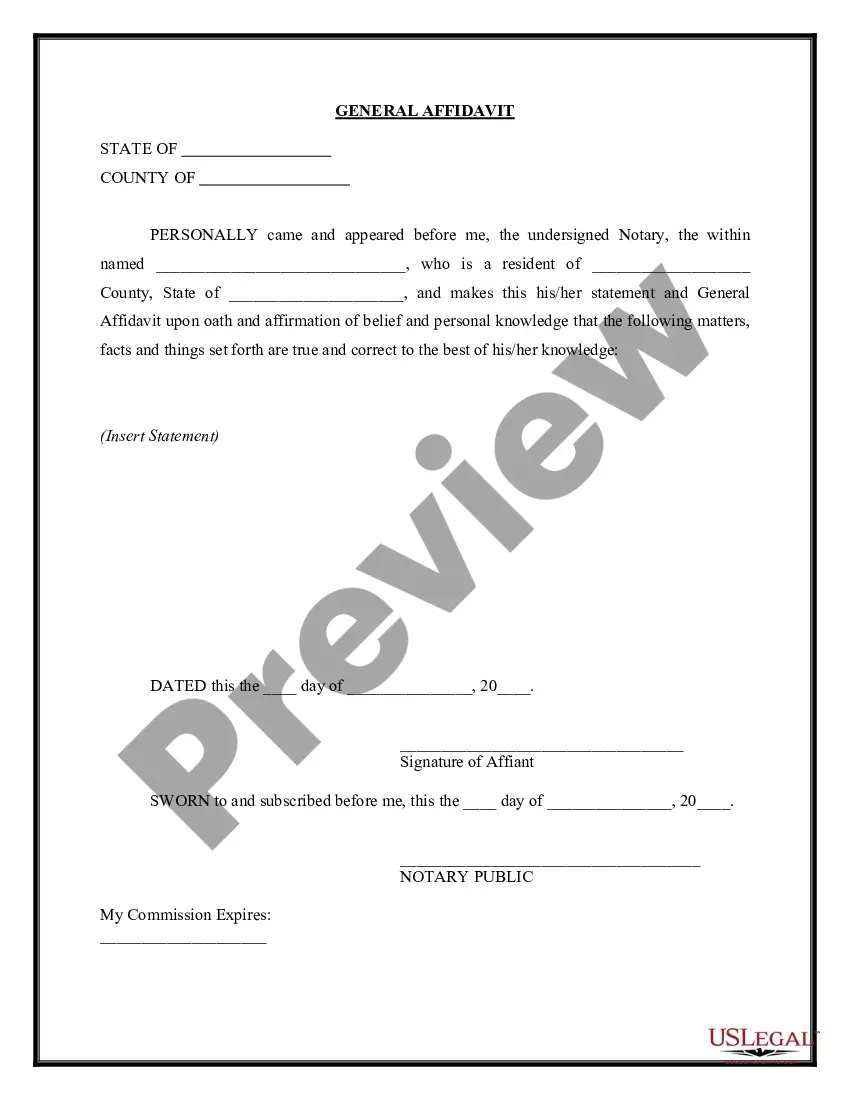
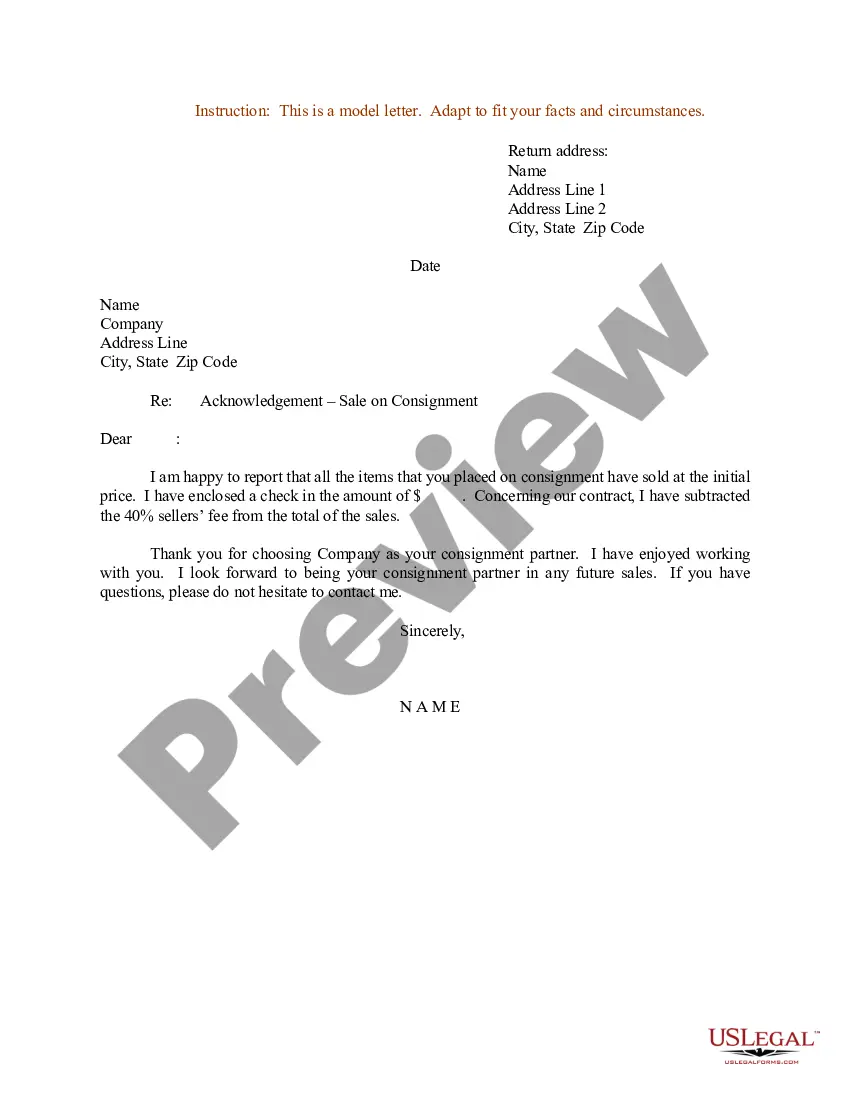
Your documentation needs to tell a clear story. First, document the results of the mental status assessment, including patient statements and behaviors. Then, document the information you provided to your patient and his response, in his own words. Note any additional written information you gave him.
As with the informed consent process, informed refusal should be documented in the medical record and include the following: describe the intervention offered; identify the reasons the intervention was offered; identify the potential benefits and risks of the intervention;
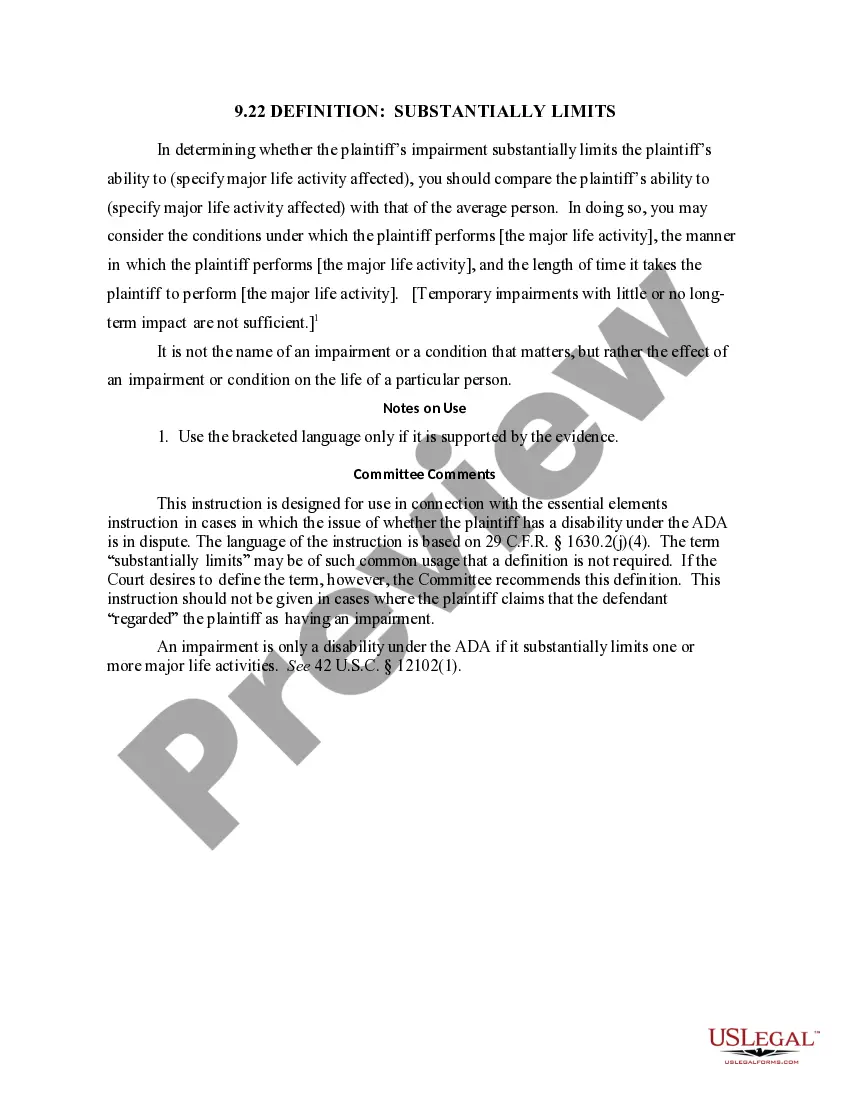
Dentists can refuse to treat you under certain conditions, but it's still their ethical duty to treat you. Whether it's behavior, medical risks, or payment issues, knowing why a dentist might refuse dental treatment can help you prevent them.
Document Nonadherent or Noncompliant Behavior Document with specificity any nonadherent, noncompliant, or disruptive behavior, such as canceled or no-show appointments, failure to follow instructions, and inappropriate conduct toward staff or other visitors to the practice.
Documentation should include the following: The patient's capacity to understand the information being provided or discussed. Treatment was offered and refused. The reasons a patient refuses a treatment.
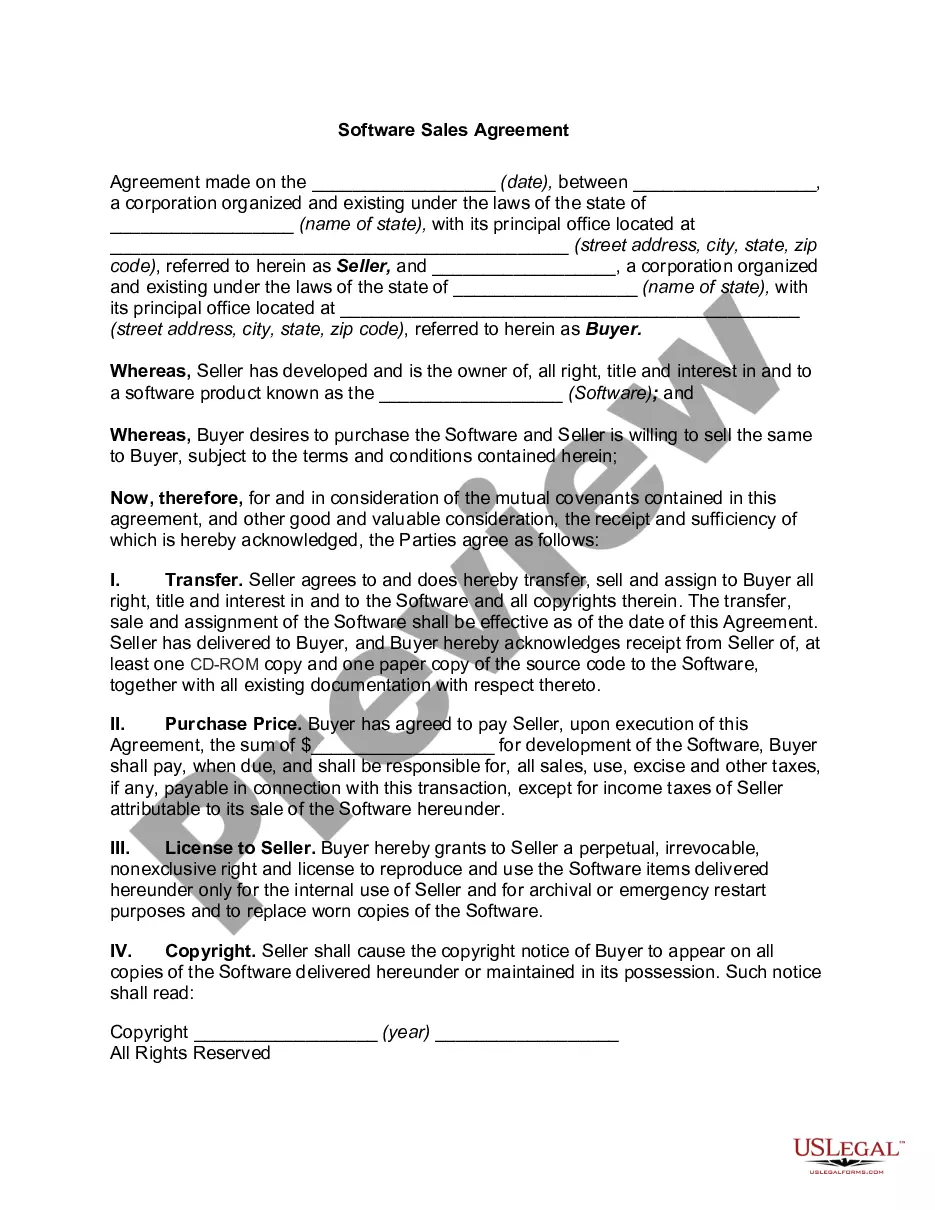
Every patient has the right to accept or refuse recommended treatment from their dentist, known as informed consent or refusal.
If a patient refuses treatment, you must decide whether or not to keep them in your practice. There is no right or wrong decision and each decision carries its own risks.
Your documentation in the medical record must include that you and the primary care provider informed him about: the problem needing treatment or diagnosis. the proposed treatment, medication, or diagnostic test. the anticipated benefits, risks, complications, adverse reactions, and consequences of the proposed treatment.
The consent form should describe if/when identifiable data will be destroyed and how such data will be protected and how it will be used or shared. Language - Consent forms should be written in the 2nd person (i.e., "you are") and in a language that is clear, concise, and understandable to the subject population.
Dental clearance is communication between a healthcare provider and a patient's dentist to validate that planned medical/surgical treatment is safe for the patient and to review the potential need for dental treatment before the medical/surgical treatment.