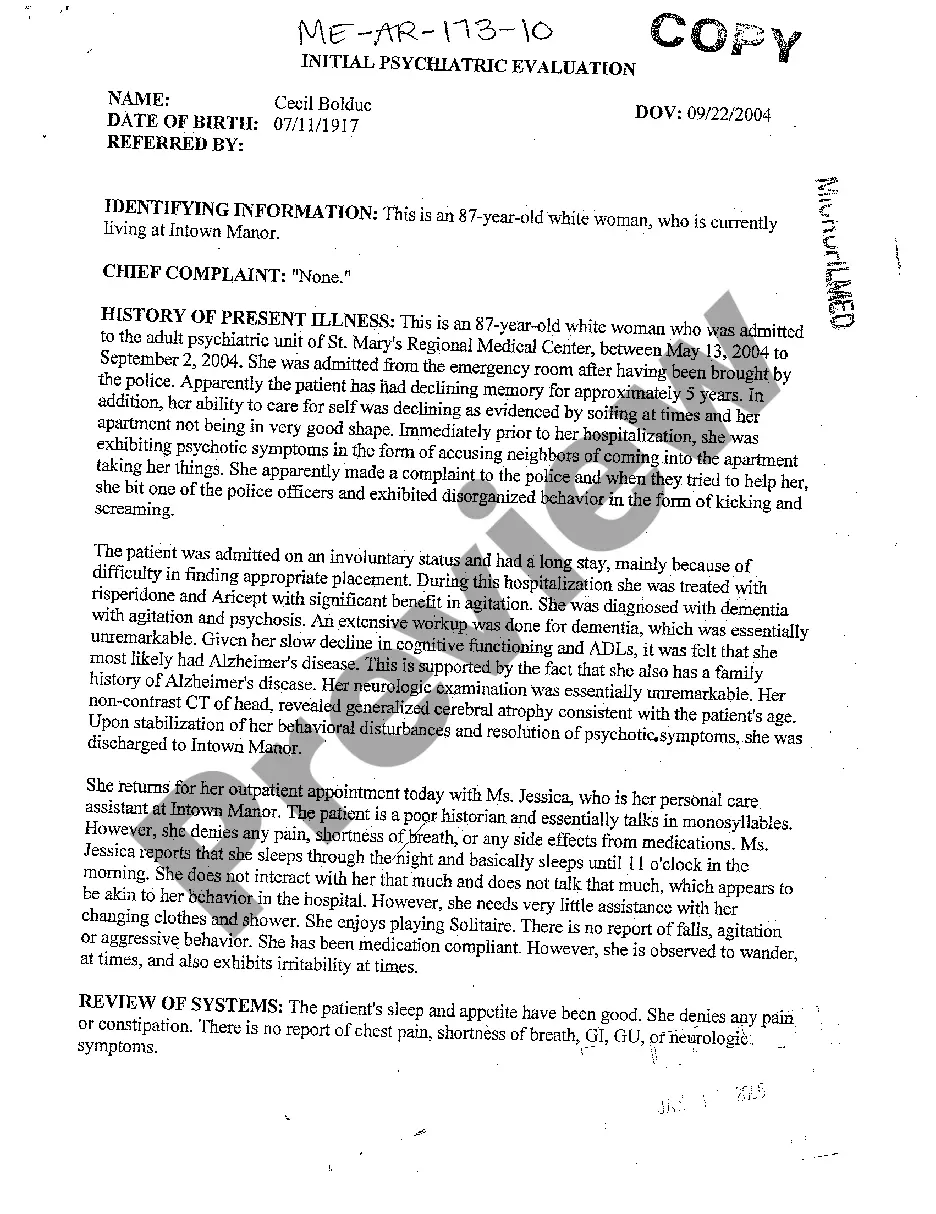
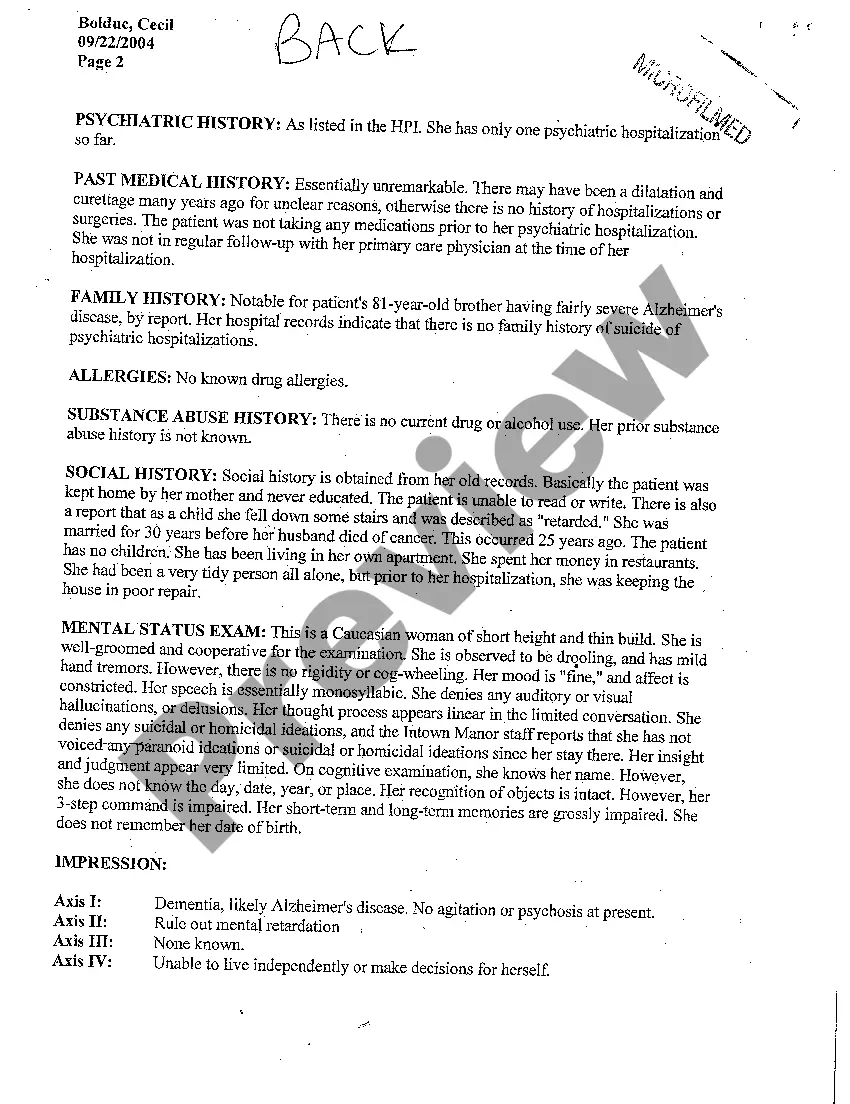
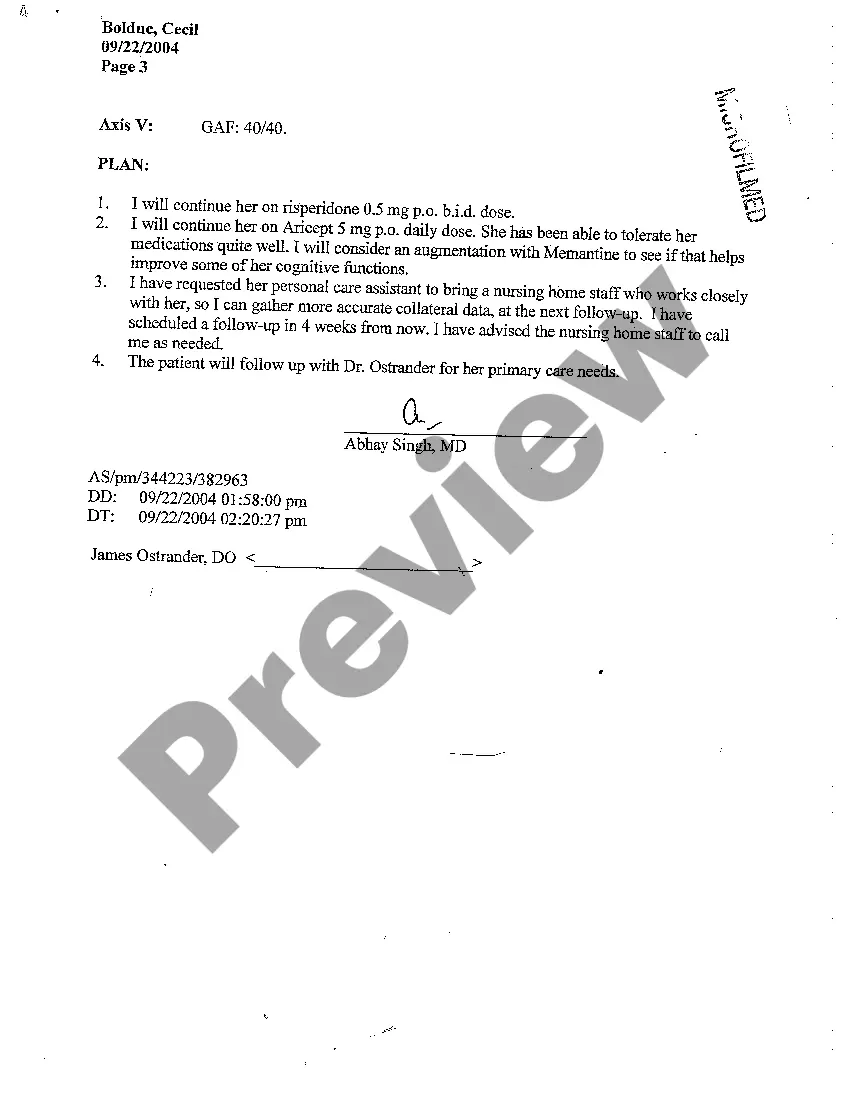
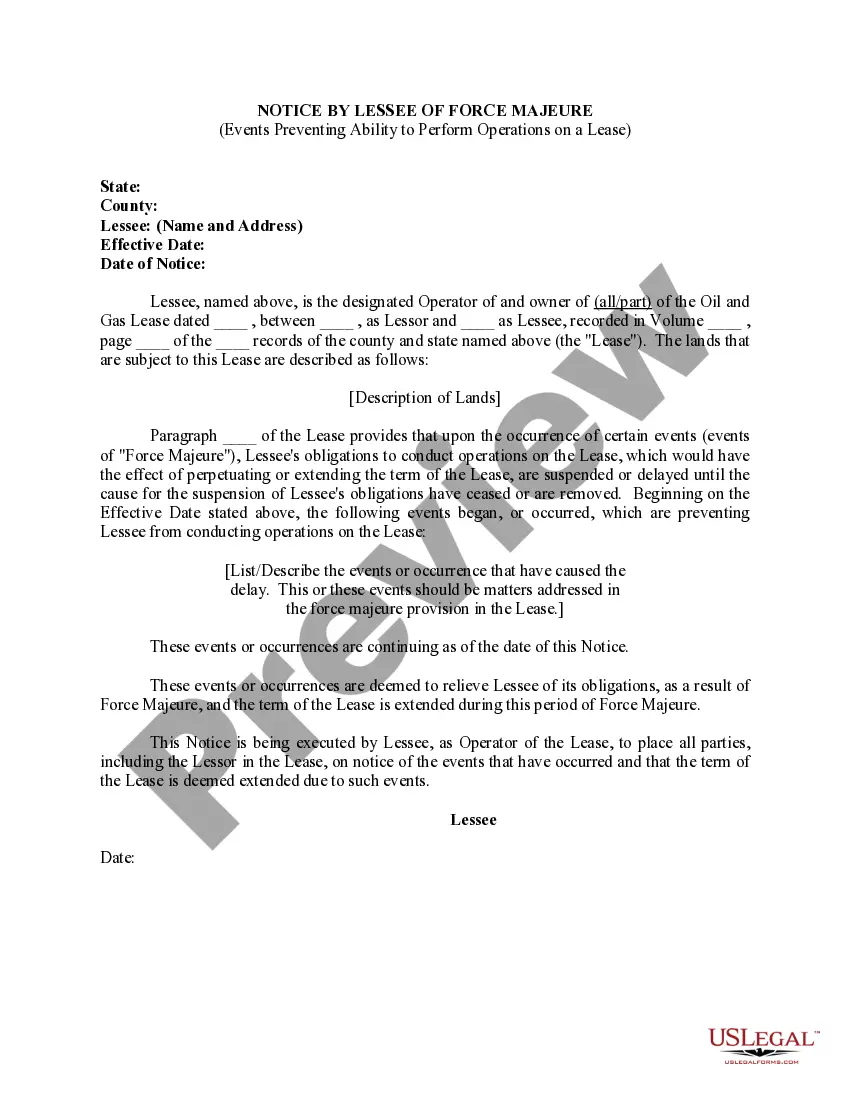
Template For Initial Psychiatric Evaluation
Description
How to fill out Maine Initial Psychiatric Evaluation?
Finding a go-to place to access the most recent and relevant legal samples is half the struggle of working with bureaucracy. Finding the right legal files calls for precision and attention to detail, which is the reason it is very important to take samples of Template For Initial Psychiatric Evaluation only from reliable sources, like US Legal Forms. An improper template will waste your time and hold off the situation you are in. With US Legal Forms, you have little to be concerned about. You may access and check all the information regarding the document’s use and relevance for the situation and in your state or county.
Take the following steps to complete your Template For Initial Psychiatric Evaluation:
- Utilize the catalog navigation or search field to find your template.
- Open the form’s information to check if it fits the requirements of your state and area.
- Open the form preview, if there is one, to ensure the template is definitely the one you are searching for.
- Resume the search and look for the correct template if the Template For Initial Psychiatric Evaluation does not match your needs.
- If you are positive regarding the form’s relevance, download it.
- When you are an authorized customer, click Log in to authenticate and gain access to your picked templates in My Forms.
- If you do not have an account yet, click Buy now to get the form.
- Pick the pricing plan that fits your needs.
- Go on to the registration to complete your purchase.
- Finalize your purchase by picking a transaction method (credit card or PayPal).
- Pick the file format for downloading Template For Initial Psychiatric Evaluation.
- Once you have the form on your gadget, you may modify it using the editor or print it and finish it manually.
Remove the inconvenience that accompanies your legal documentation. Discover the comprehensive US Legal Forms collection where you can find legal samples, examine their relevance to your situation, and download them on the spot.
Form popularity
FAQ
Your intake appointment can take one to two hours. You'll fill out paperwork and assessments to help determine a diagnosis. After that, you'll have a conversation with the psychiatrist and an NP or PA may observe. The doctor will get to know you and come to understand why you are seeking treatment.
Components of a clinical encounter which should be documented include: Chief Complaint or Reason for Encounter. Referral Source. History of Present Illness. Current Treatments including medications and ongoing therapies. Mental Status Examination. Diagnoses. Treatment Plan including.
The mental health test assesses your emotional wellbeing via a series of questions and also includes a physical examination. As a priority your doctor will determine if you are at risk of hurting yourself or others. For children, the mental health assessment will be tailored to the child's age and stage of development.
Elicit specific information, including a history of the presenting problems, pertinent medical information, family background, social history, and specific symptom and behavioral patterns. Formally test mental status (see that Chapter). Ask if the patient has any questions or unmentioned concerns.
To conduct a successful initial assessment with your patient, you should document their: Presenting problems. Mental health status and history. Previous treatments. Current providers. Relevant demographic information. Medications. Substance use information. Physical or mental health conditions.