Pa Real Form For United Healthcare
Description
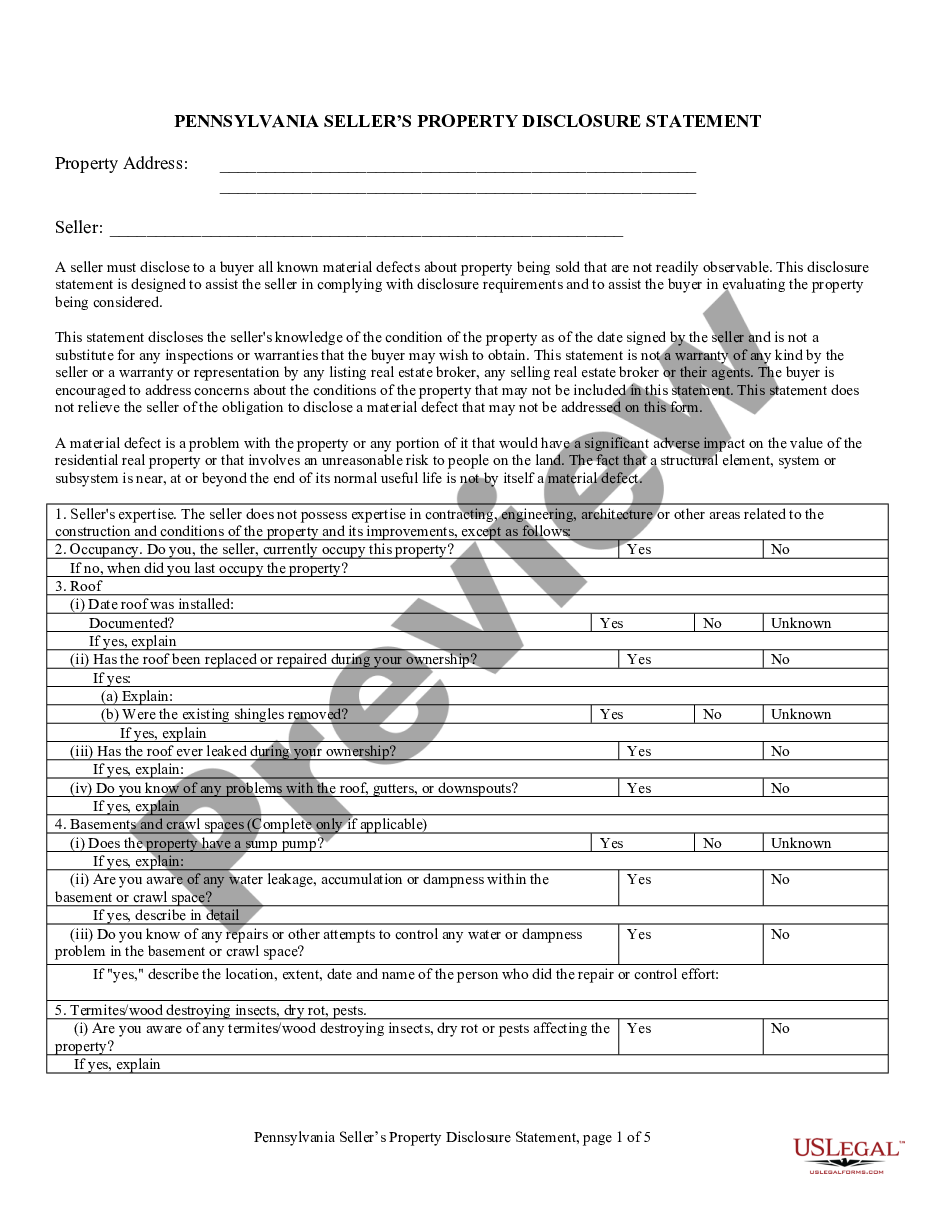
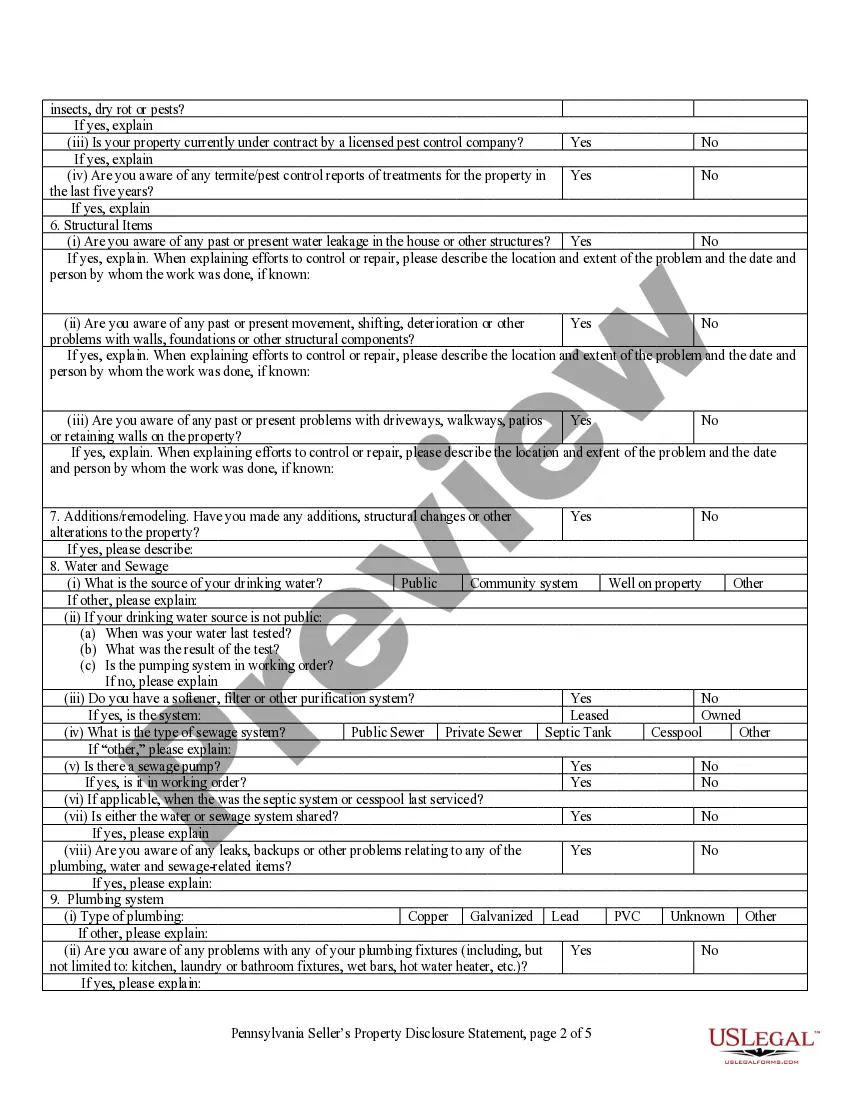
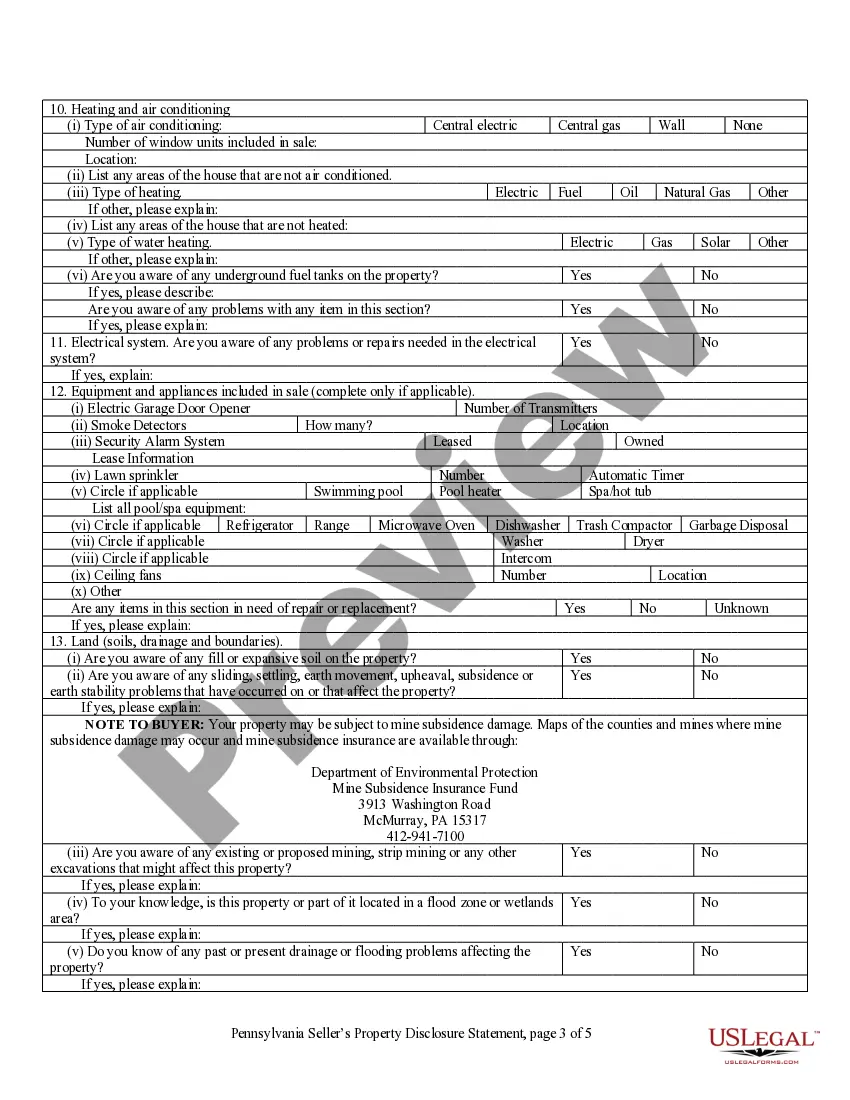
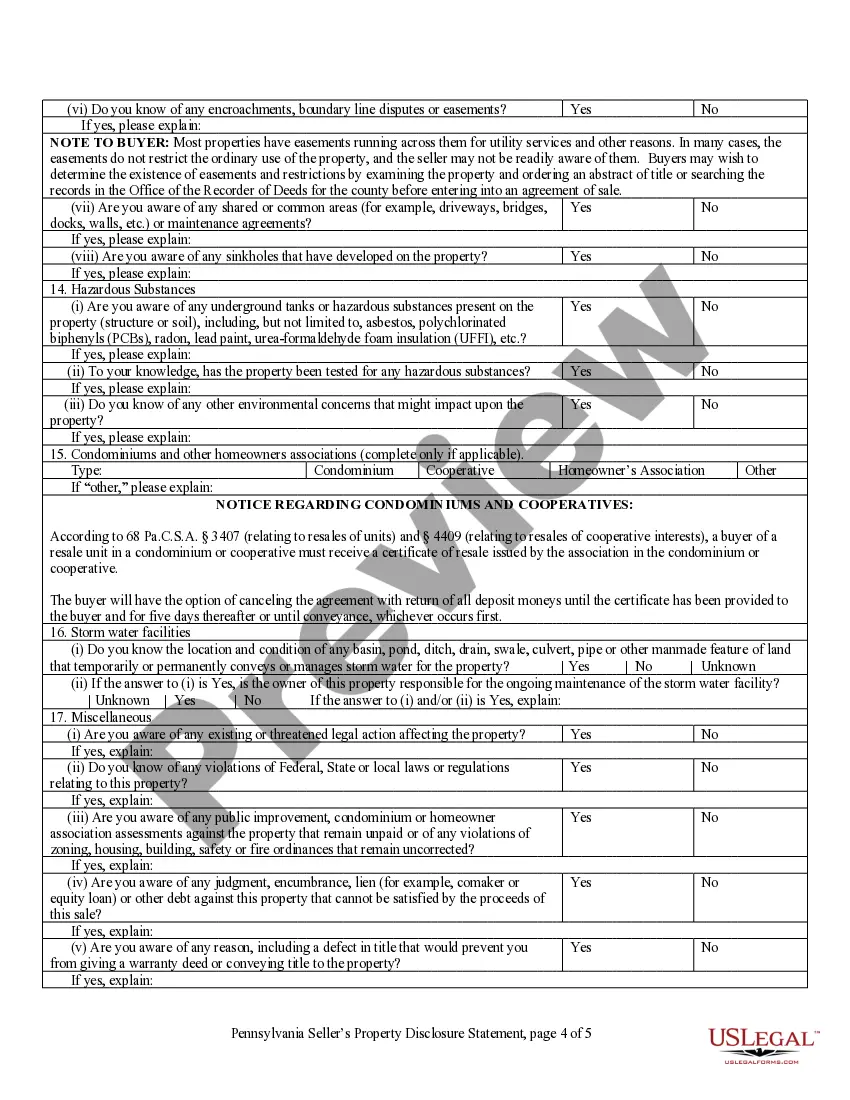
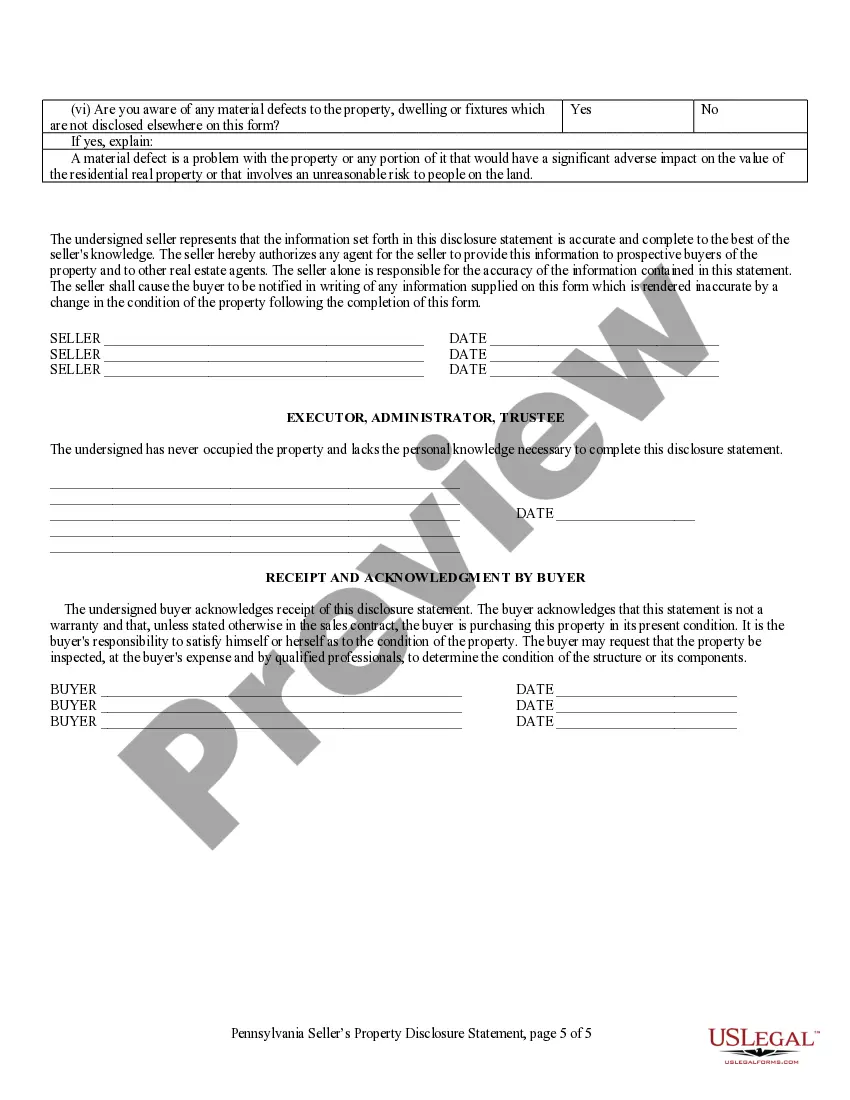
How to fill out Pennsylvania Residential Real Estate Sales Disclosure Statement?
Drafting legal documents from scratch can sometimes be daunting. Certain scenarios might involve hours of research and hundreds of dollars invested. If you’re looking for a a more straightforward and more cost-effective way of preparing Pa Real Form For United Healthcare or any other paperwork without jumping through hoops, US Legal Forms is always at your fingertips.
Our online catalog of over 85,000 up-to-date legal documents addresses almost every aspect of your financial, legal, and personal affairs. With just a few clicks, you can instantly access state- and county-compliant forms carefully prepared for you by our legal professionals.
Use our website whenever you need a trusted and reliable services through which you can quickly find and download the Pa Real Form For United Healthcare. If you’re not new to our services and have previously set up an account with us, simply log in to your account, select the template and download it away or re-download it anytime later in the My Forms tab.
Don’t have an account? No worries. It takes minutes to set it up and explore the catalog. But before jumping directly to downloading Pa Real Form For United Healthcare, follow these tips:
- Check the document preview and descriptions to make sure you have found the form you are looking for.
- Check if form you select conforms with the regulations and laws of your state and county.
- Choose the right subscription option to purchase the Pa Real Form For United Healthcare.
- Download the file. Then complete, sign, and print it out.
US Legal Forms has a spotless reputation and over 25 years of expertise. Join us today and turn form completion into something easy and streamlined!
Form popularity
FAQ
What is a Prior Authorization? A prior authorization (PA), sometimes referred to as a ?pre-authorization,? is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
Prior authorization (prior auth, or PA) is a management process used by insurance companies to determine if a prescribed product or service will be covered. This means if the product or service will be paid for in full or in part.
The healthcare provider is usually responsible for initiating prior authorization by submitting a request form to a patient's insurance provider. As mentioned in the ?How does prior authorization work?? section above, this will then often prompt a time-consuming back and forth between the provider and payer.
Prior authorization works like this: Step 1: If your doctor didn't contact your insurance company when prescribing a medication, your pharmacy will contact them. ... Step 2: The physician (or their staff) will contact the insurance company. ... Step 3: Your insurance provider may want you to fill out and sign some forms.
Starting September 1, 2022, UnitedHealthcare will no longer be a Medical Assistance plan option in the Southwest and Lehigh/Capital areas of Pennsylvania. United Healthcare will continue to be an available plan if you live in Southeastern Pennsylvania (Bucks, Chester, Delaware, Montgomery, or Philadelphia counties).