Hillsborough Florida Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
Preparing documents for business or personal needs is always a significant obligation.
When drafting a contract, a public service application, or a power of attorney, it's essential to take into account all federal and state regulations of the specific region.
However, small counties and even municipalities also possess legislative rules that you need to consider.
Check that the template adheres to legal standards and click Buy Now.
- All these factors make it stressful and time-consuming to produce a Hillsborough Notice from Employer to Employee Regarding Early Termination of Continuation Coverage without expert help.
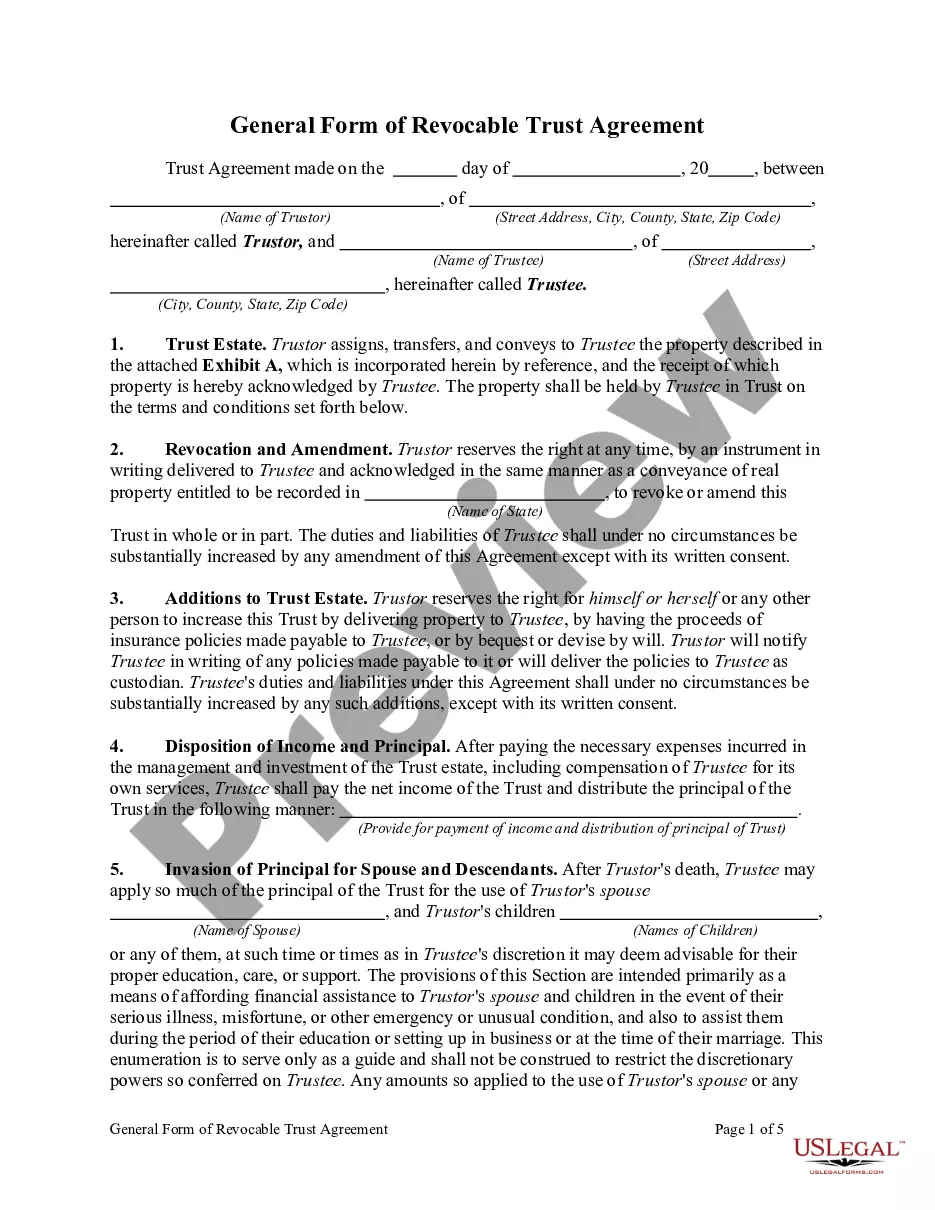
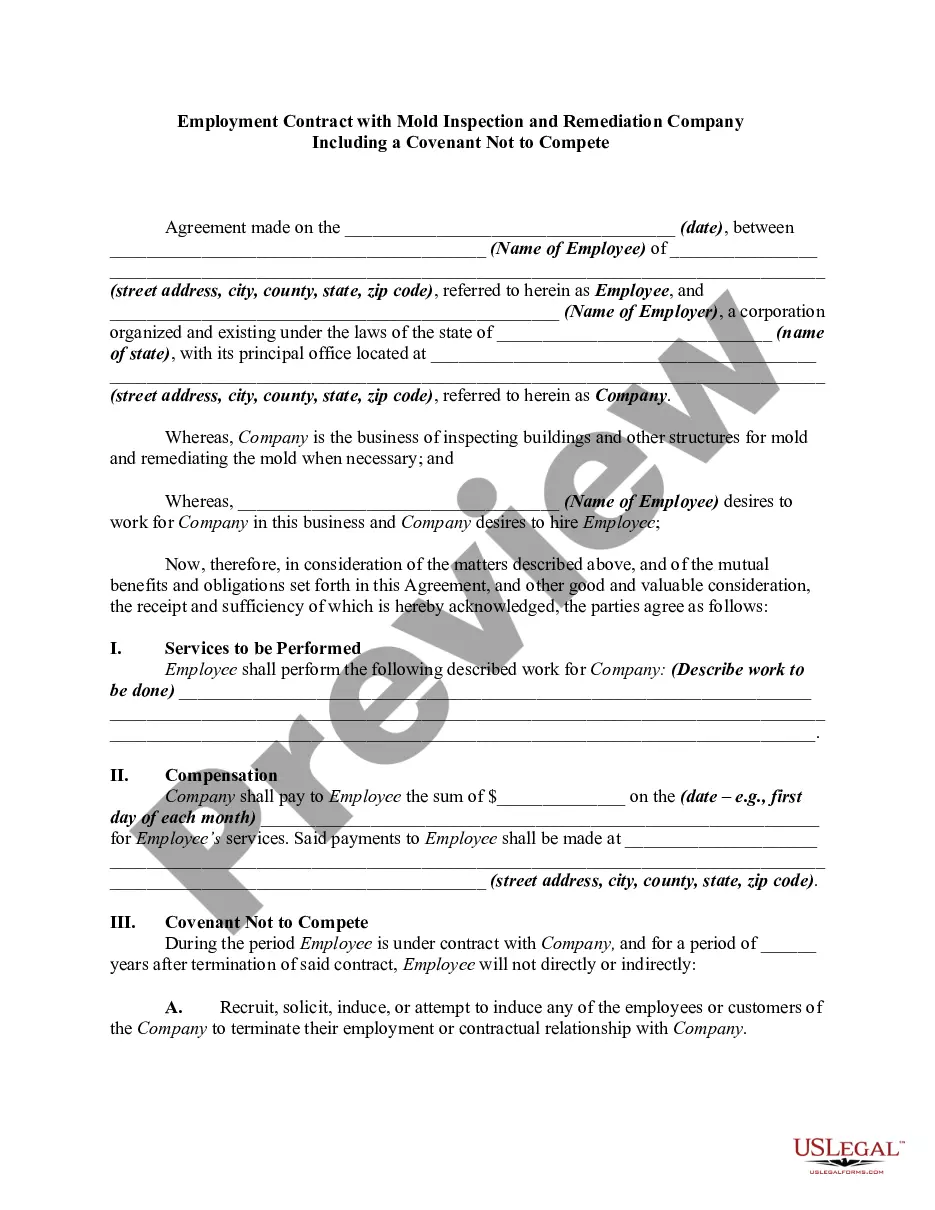
- You can potentially save on legal fees by drafting your documentation and creating a legally valid Hillsborough Notice from Employer to Employee Regarding Early Termination of Continuation Coverage yourself, utilizing the US Legal Forms online library.
- This is the most extensive online collection of state-specific legal templates that are professionally verified, ensuring their validity when selecting a sample for your county.
- Previously subscribed users only need to Log In to their accounts to retrieve the necessary form.
- If you don't have a subscription yet, follow the step-by-step guide below to obtain the Hillsborough Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
- Review the page you've accessed and confirm whether it contains the document you need.
- To do this, utilize the form description and preview if these options are available.
Form popularity
FAQ
Yes, employers with fewer employees may be affected by mini COBRA laws specific to Florida, which provide rights to health insurance continuation. This type of coverage allows employees to maintain health insurance despite job changes. If you have received a Hillsborough Florida Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, it is essential to understand how these laws apply to your situation.
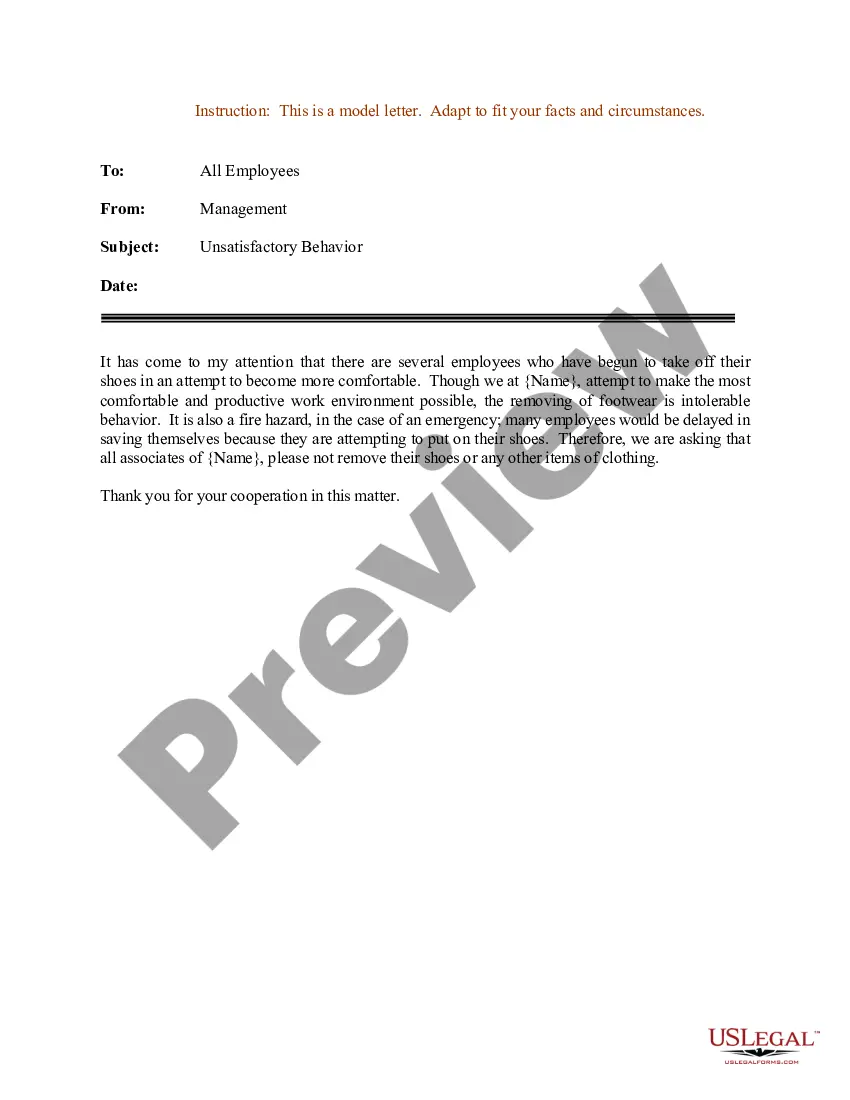
The COBRA termination letter format must include the reason why the coverageis being terminated, the rights of the beneficiaries, and the specific date the coverage will end. The letter is customized to fit theD particular plan offered by the company as well as particulars related to the employee.
State continuation coverage refers to state laws that enable employees to extend their employer-sponsored group health insurance even if they are not eligible for an extension through COBRA. While COBRA law applies throughout the U.S., it is only applicable to employers with 20 or more employees.
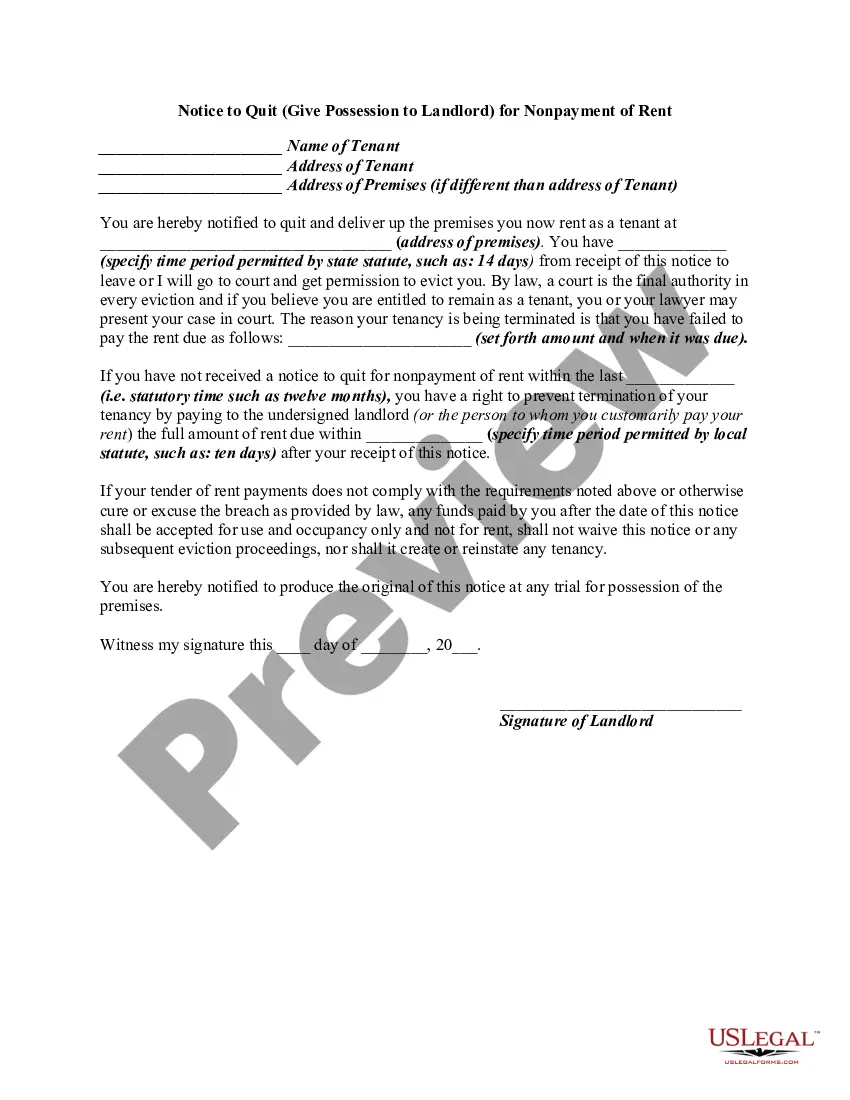
COBRA requires continuation coverage to be offered to covered employees, their spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain specific events.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
A covered employee's spouse who would lose coverage due to a divorce may elect continuation coverage under the plan for a maximum of 36 months. A qualified beneficiary must notify the plan administrator of a qualifying event within 60 days after divorce or legal separation.