Bronx New York Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
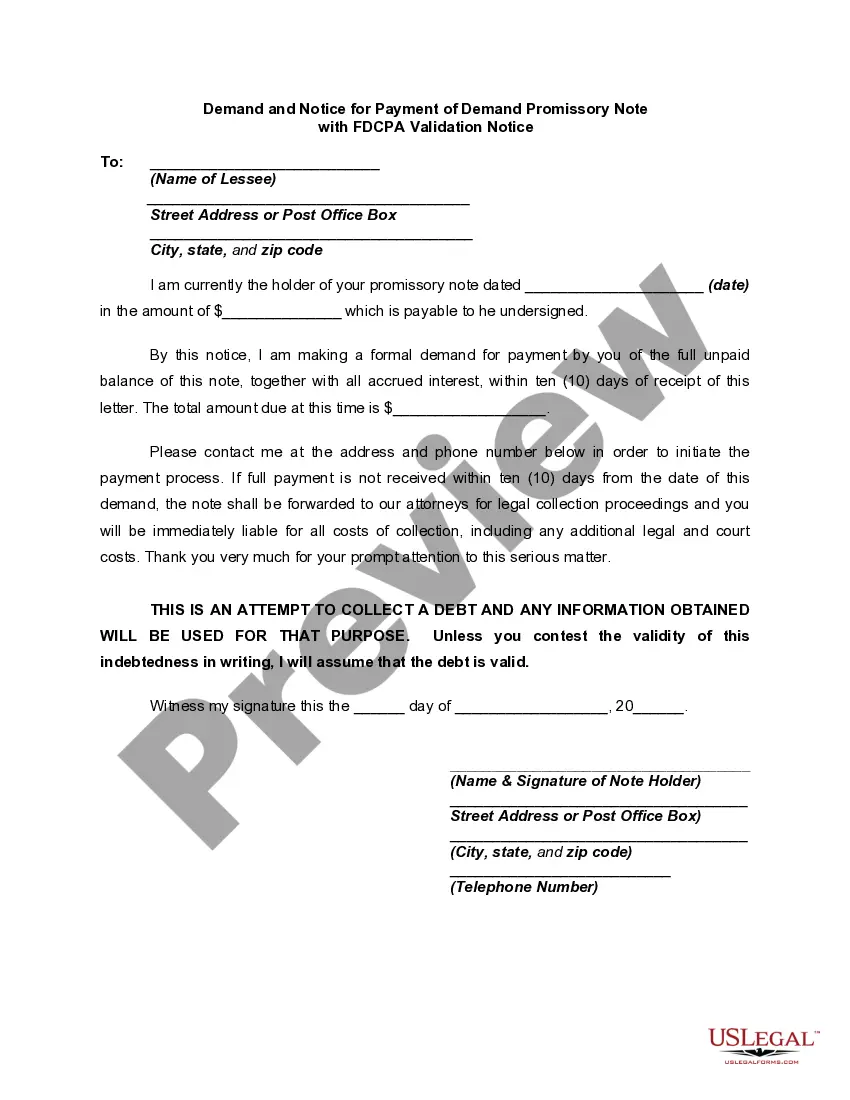
Are you seeking to swiftly generate a legally-binding Bronx Qualifying Event Notice Information for Employer to Plan Administrator or perhaps any other document to manage your personal or business affairs? You can choose one of the two alternatives: engage a professional to compose a valid document for you or create it completely by yourself. The good news is, there's another choice - US Legal Forms. It will assist you in obtaining well-written legal documentation without incurring excessive fees for legal services.
US Legal Forms offers a comprehensive catalog of over 85,000 state-specific document templates, including Bronx Qualifying Event Notice Information for Employer to Plan Administrator and form packages. We provide documents for a variety of scenarios: from divorce papers to real estate document templates. We've been in operation for more than 25 years and have established a solid reputation among our clients. Here's how you can join them and acquire the necessary document without unnecessary complications.
If you have already registered an account, you can effortlessly Log In to it, find the Bronx Qualifying Event Notice Information for Employer to Plan Administrator template, and download it. To re-download the form, simply navigate to the My documents tab.
It's hassle-free to purchase and download legal forms if you utilize our services. Additionally, the paperwork we offer is updated by legal professionals, which provides you with greater assurance when handling legal matters. Try US Legal Forms now and experience it for yourself!
- First, carefully confirm if the Bronx Qualifying Event Notice Information for Employer to Plan Administrator is customized to your state's or county's regulations.
- If the document includes a description, ensure to check what it's appropriate for.
- Start the search anew if the document isn’t what you were seeking by using the search box in the header.
- Choose the plan that best fits your requirements and continue to payment.
- Select the file format you prefer to receive your document in and download it.
- Print it out, fill it in, and sign on the designated line.
Form popularity
FAQ
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
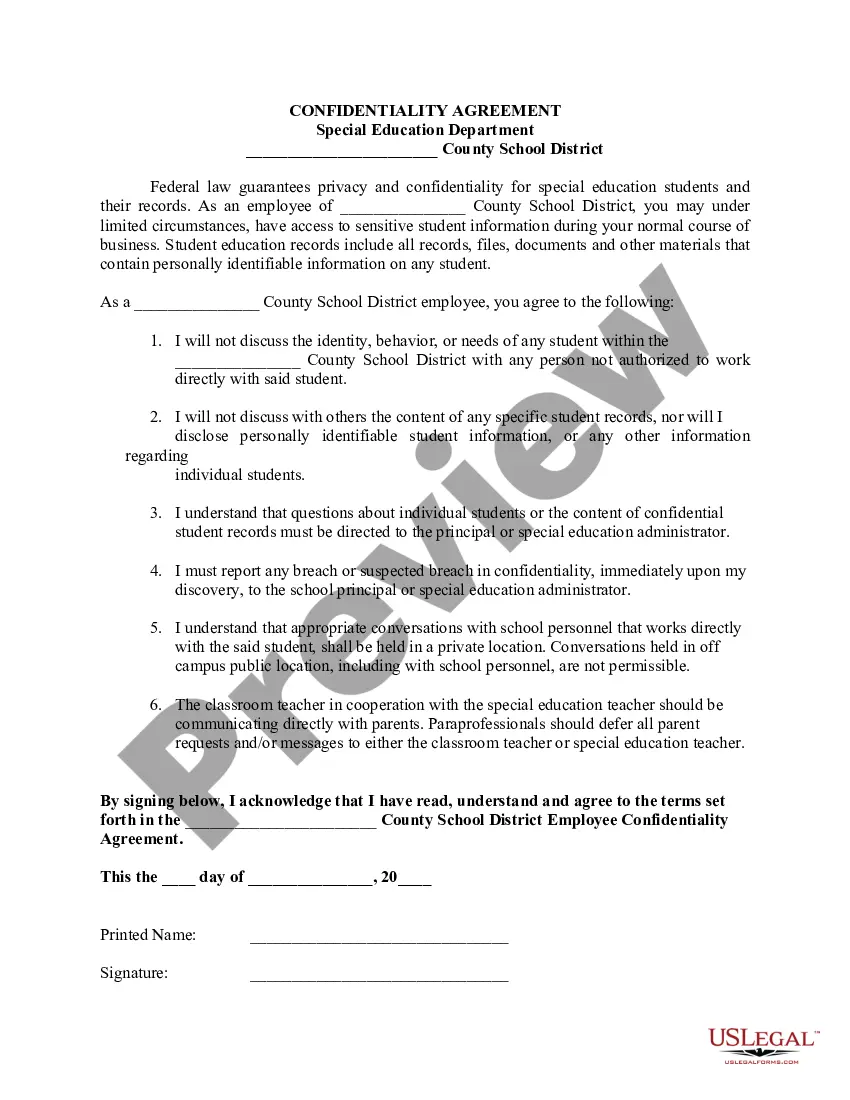
Cal-COBRA administration requires four basic compliance components: Notifying all eligible group health care participants of their Cal-COBRA rights. Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Voluntary or involuntary termination of the covered employee's employment for any reason other than gross misconduct. Reduction in the hours worked by the covered employee below plan eligibility requirements. Covered employee becoming entitled to Medicare. Divorce or legal separation of the covered employee.
Which of the following is considered a qualifying event under cobra? Divorce. Other qualifying events include the voluntary termination of employment; an employee's change from full time to part time; or the death of the employee.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section. Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.
In general, the COBRA qualifying event must be a termination of employment or a reduction of the covered employee's employment hours. Second, the covered employee must be determined under title II or title XVI of the Social Security Act to be disabled.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.