Maricopa Arizona Notice of Qualifying Event from Employer to Plan Administrator
Category:
State:
Multi-State
County:
Maricopa
Control #:
US-AHI-005
Format:
Word;
Rich Text
Instant download
Description
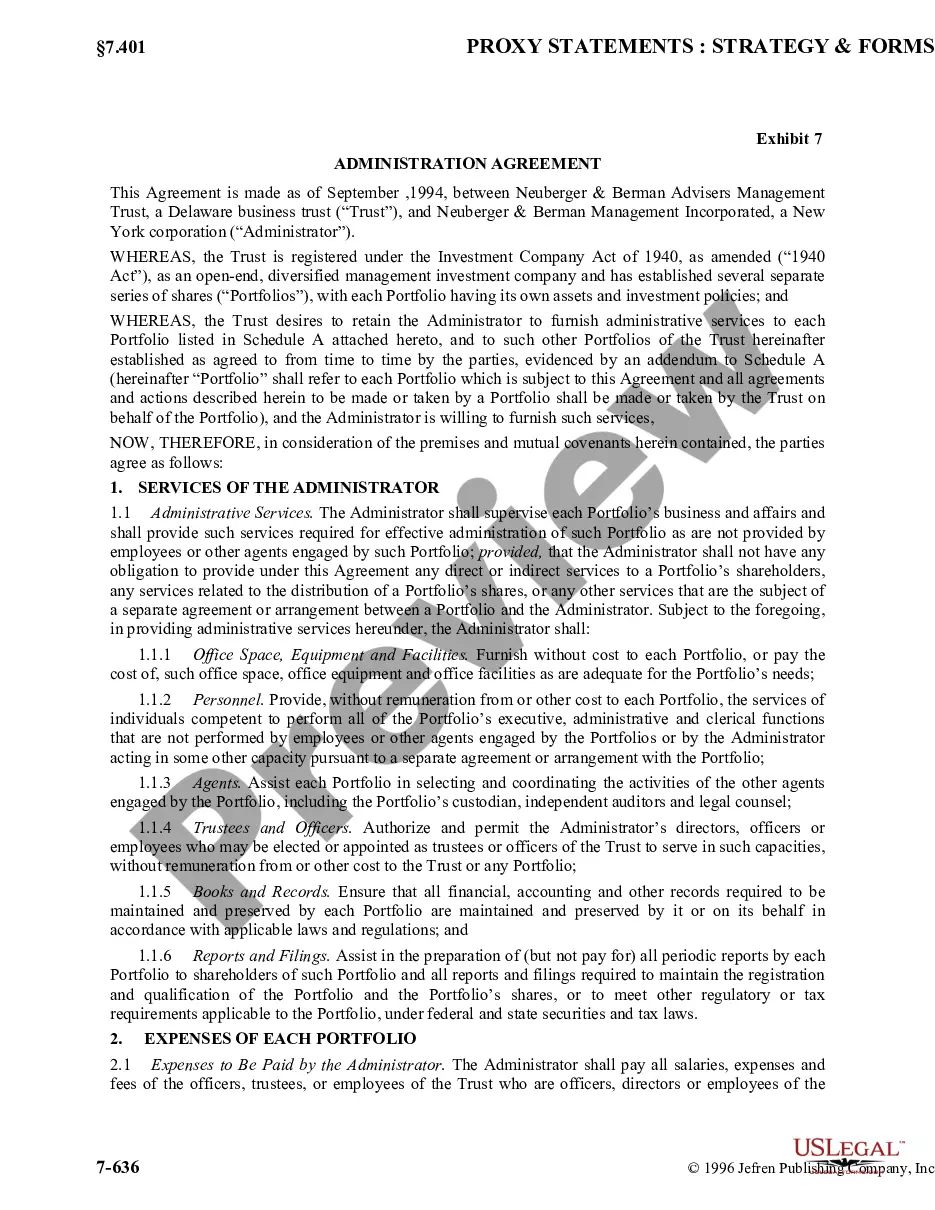
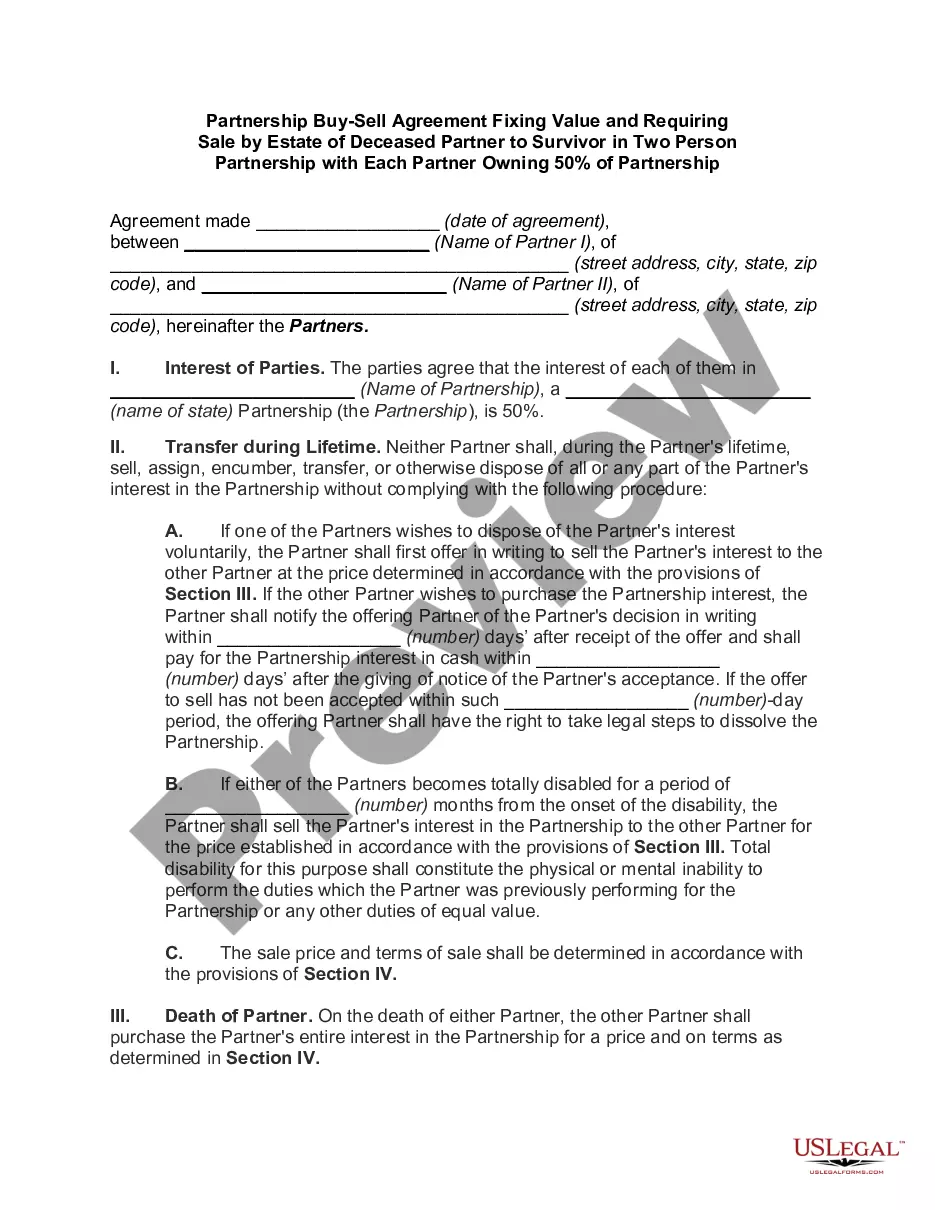
This AHI memo serveS as notice to the employer regarding (Name of Employee, Account Number) and the qualified beneficiaries under (his/her) account.
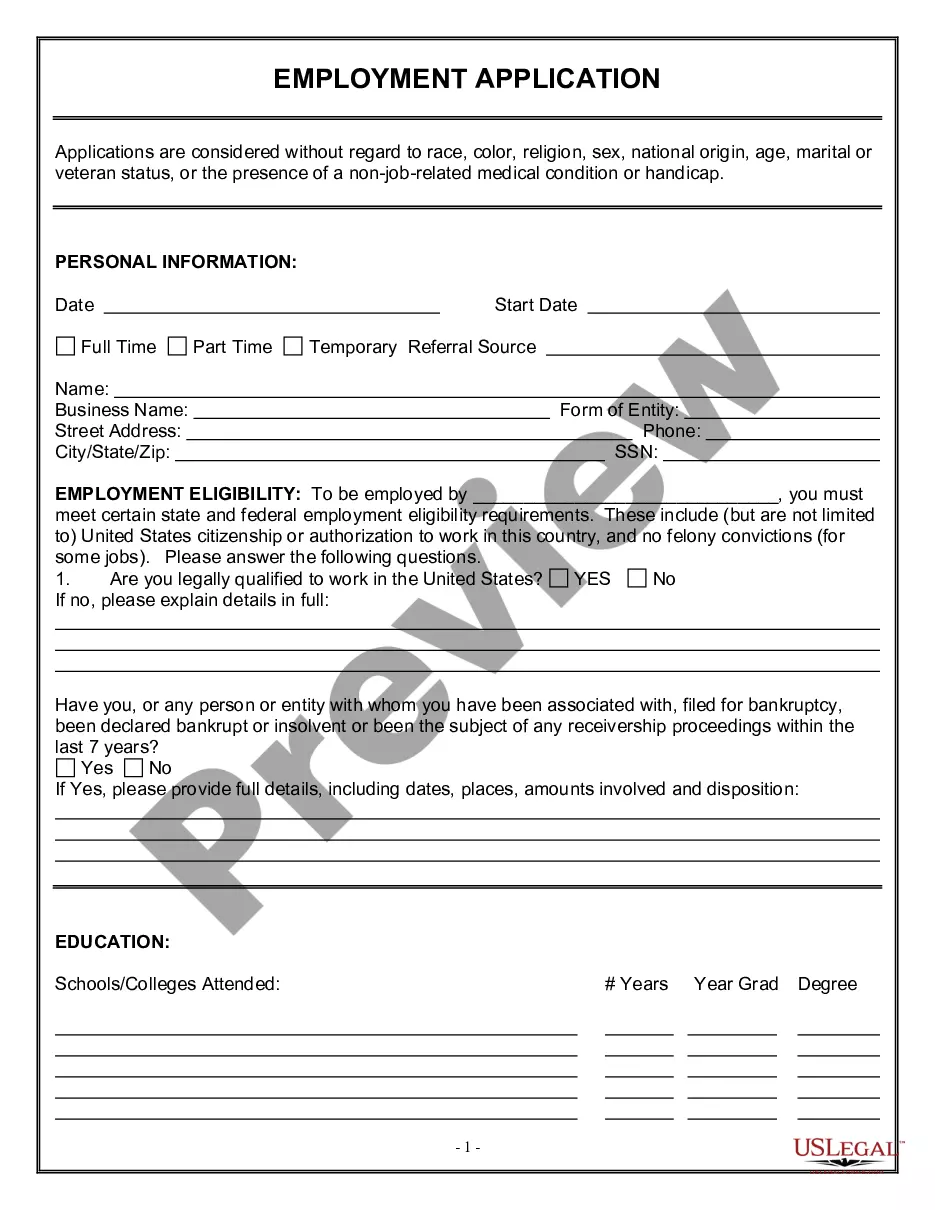
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
Preparing documents for business or personal purposes is consistently a significant obligation.
When formulating a contract, a public service application, or a power of attorney, it's crucial to take into account all federal and state laws pertaining to the particular region.
Nevertheless, minor counties and even towns also have legislative procedures that you must consider.
The remarkable aspect of the US Legal Forms library is that all the documents you've ever bought are never lost - you can retrieve them in your profile within the My documents tab at any time. Enroll in the platform and swiftly obtain verified legal forms for any situation with just a few clicks!
- All these factors make it stressful and lengthy to generate a Maricopa Notice of Qualifying Event from Employer to Plan Administrator without professional assistance.
- It's simple to avoid incurring costs on attorneys generating your documents and create a legally valid Maricopa Notice of Qualifying Event from Employer to Plan Administrator by yourself, utilizing the US Legal Forms online library.
- It is the largest digital collection of state-specific legal documents that have been professionally scrutinized, ensuring their authenticity when selecting a template for your county.
- Previously subscribed users only need to Log In to their accounts to retrieve the required form.
- If you do not yet have a subscription, follow the step-by-step instructions below to acquire the Maricopa Notice of Qualifying Event from Employer to Plan Administrator.
- Browse through the page you've accessed and confirm if it contains the document you require.
- To accomplish this, utilize the form description and preview if these features are offered.