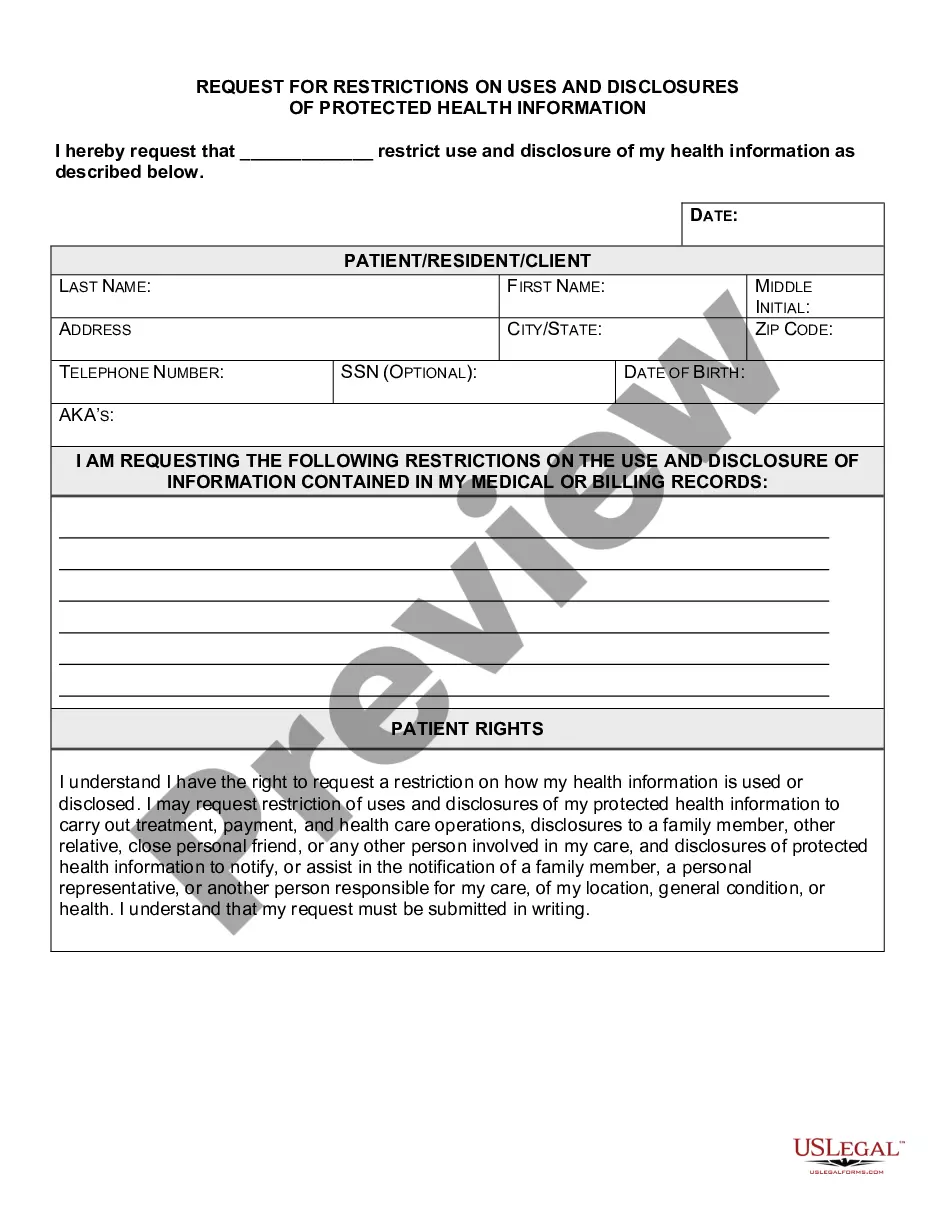
Virginia Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
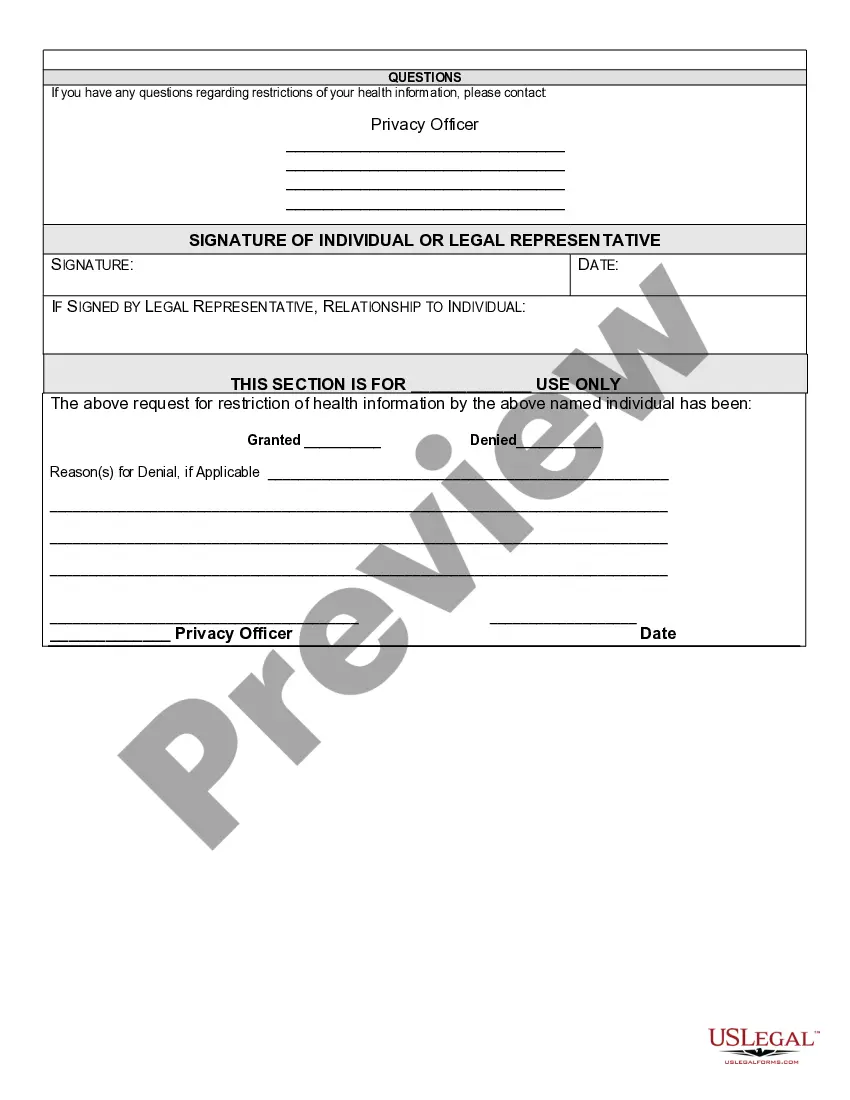
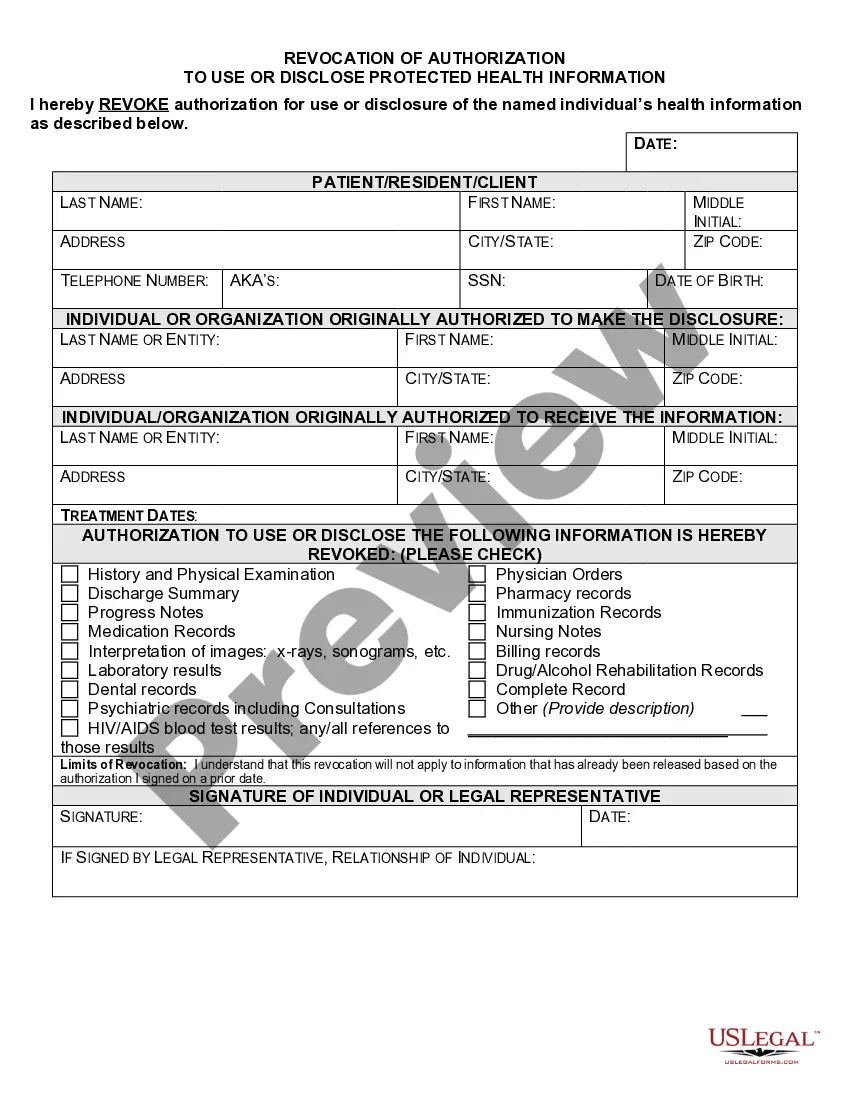
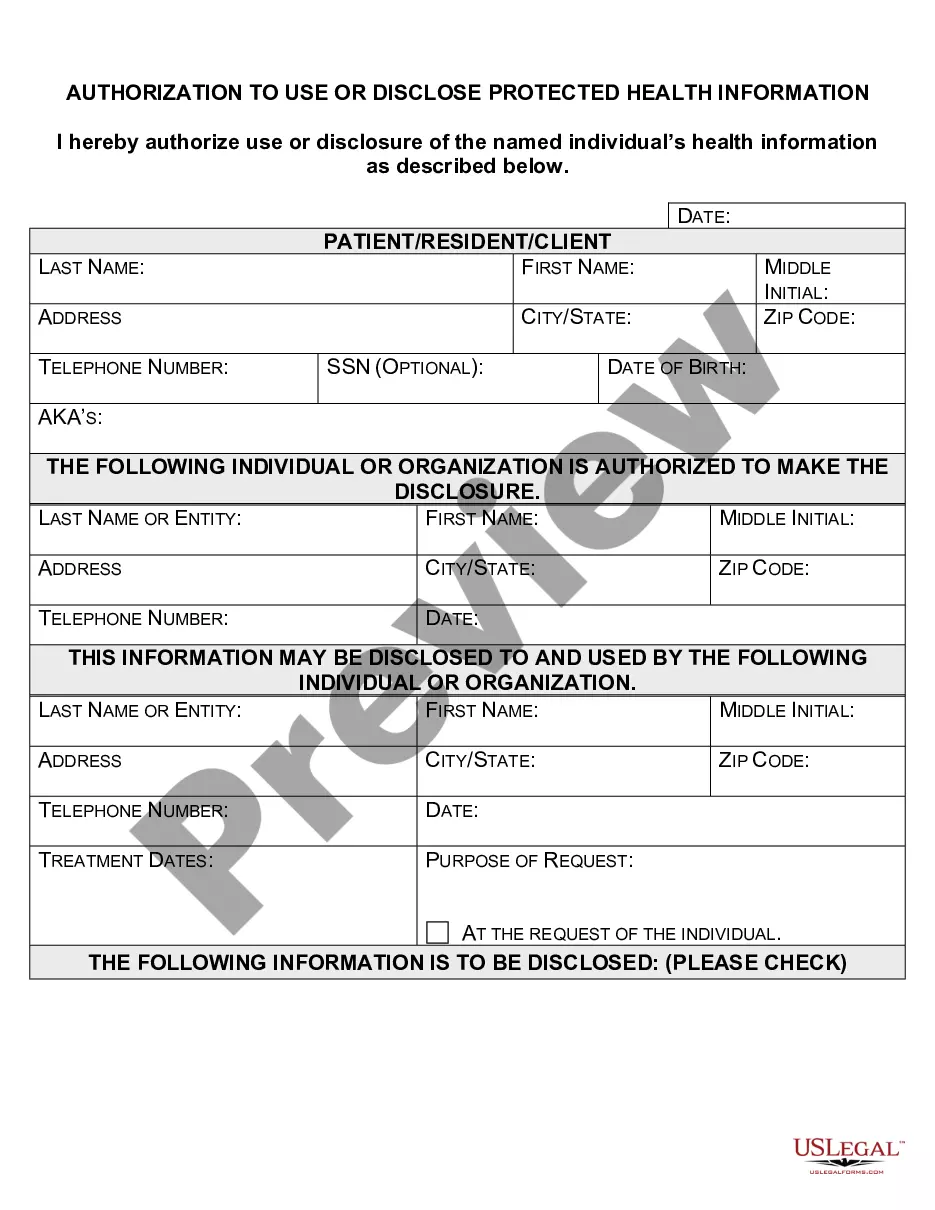
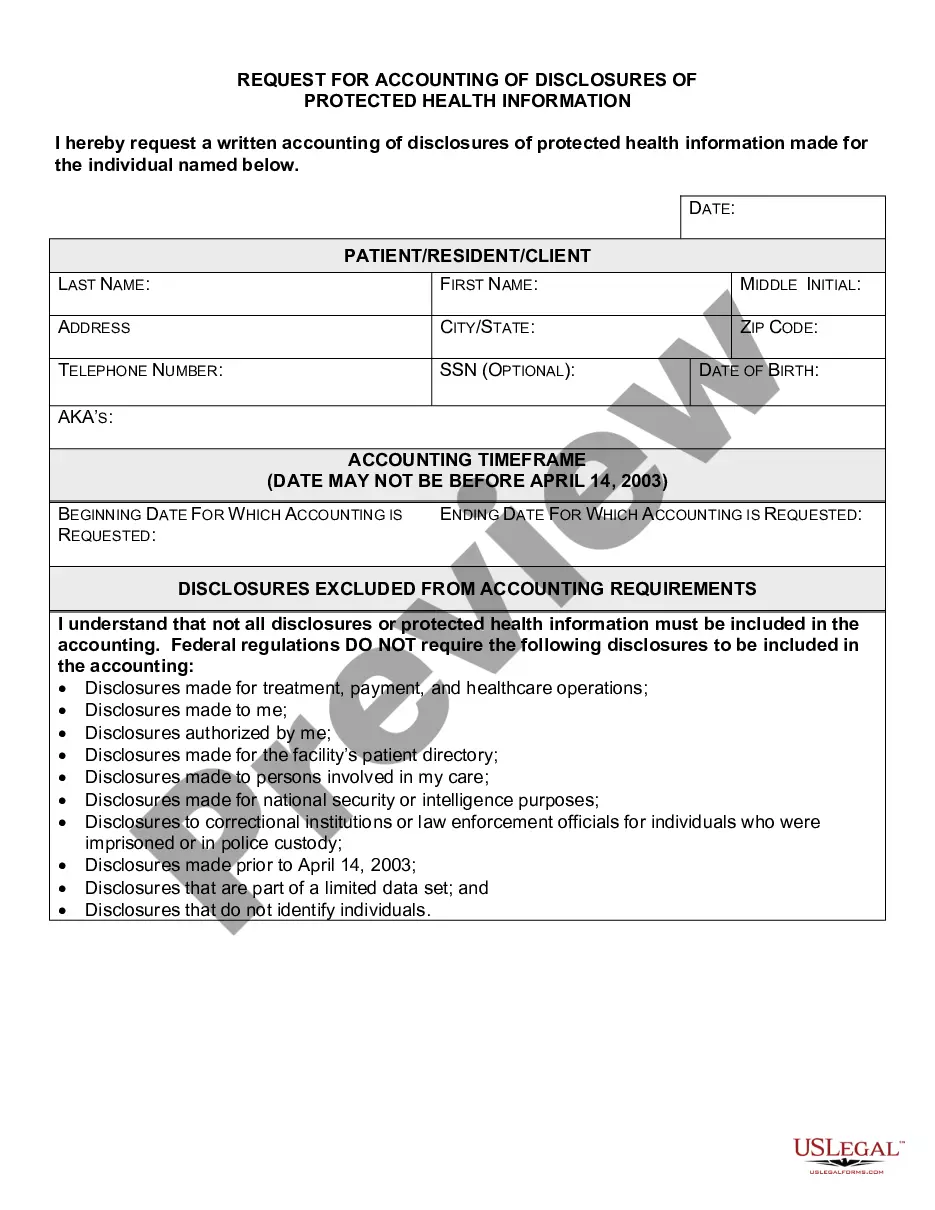
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
You might spend time online looking for the legal document template that fits the state and federal criteria you require.
US Legal Forms offers a vast array of legal templates that can be reviewed by professionals.
You can acquire or create the Virginia Request for Restrictions on Uses and Disclosures of Protected Health Information through your account.
If available, use the Review button to examine the document template as well.
- If you have a US Legal Forms account, you may Log In and press the Acquire button.
- Afterward, you can complete, modify, create, or sign the Virginia Request for Restrictions on Uses and Disclosures of Protected Health Information.
- Each legal document template you purchase is yours indefinitely.
- To obtain another version of the purchased form, navigate to the My documents tab and click on the corresponding button.
- If this is your first time using the US Legal Forms site, follow the simple instructions below.
- First, ensure you have selected the correct document template for your desired region/city.
- Review the form description to confirm you have chosen the correct document.
Form popularity
FAQ
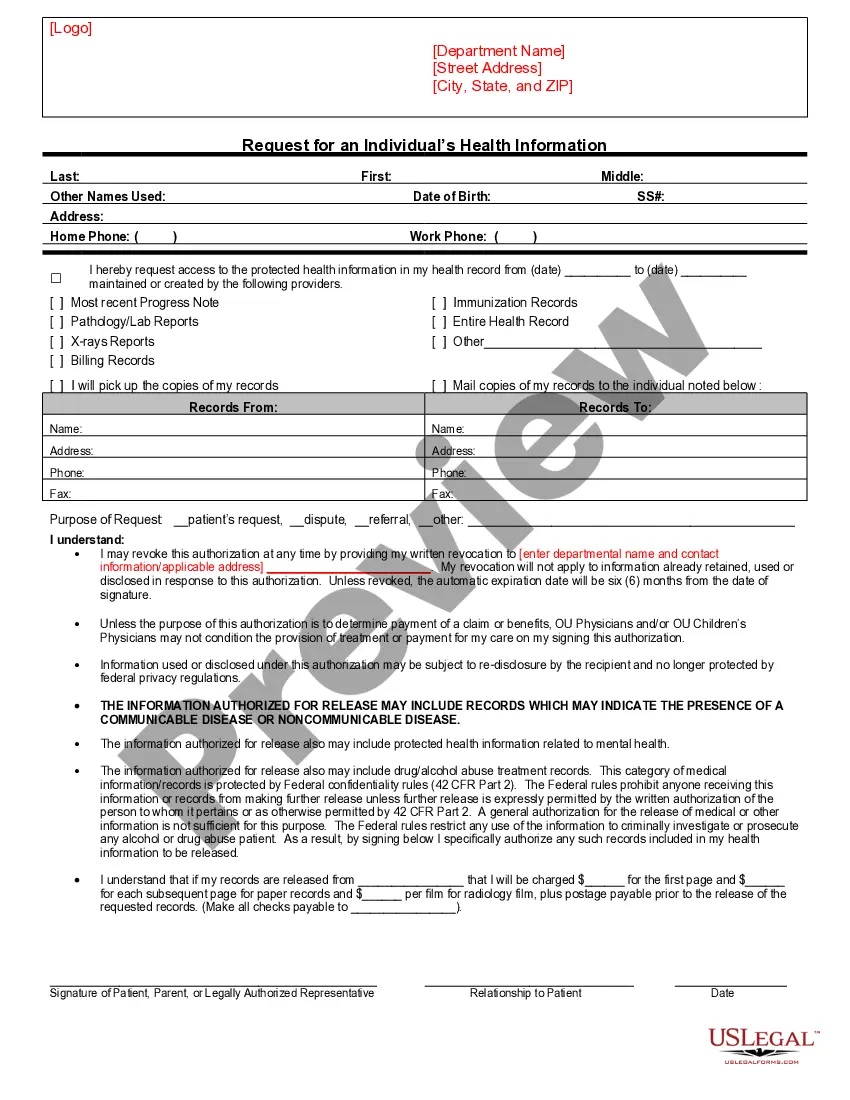
Unauthorized access, use, and disclosure refer to instances when protected health information is accessed or shared without proper consent or legal authority. This may involve employees mishandling data or external breaches by hackers. Understanding how these events occur can help you implement measures to prevent them. Engaging with the Virginia Request for Restrictions on Uses and Disclosures of Protected Health Information allows individuals to manage their health data proactively.
Yes, a covered entity can refuse to restrict PHI disclosure to health plans even if the individual pays in full out of pocket. The Virginia Request for Restrictions on Uses and Disclosures of Protected Health Information allows individuals to make such requests, but healthcare providers have discretion. It’s beneficial to understand your rights in this context. Using resources from USLegalForms can help clarify situations regarding payment and disclosure restrictions.
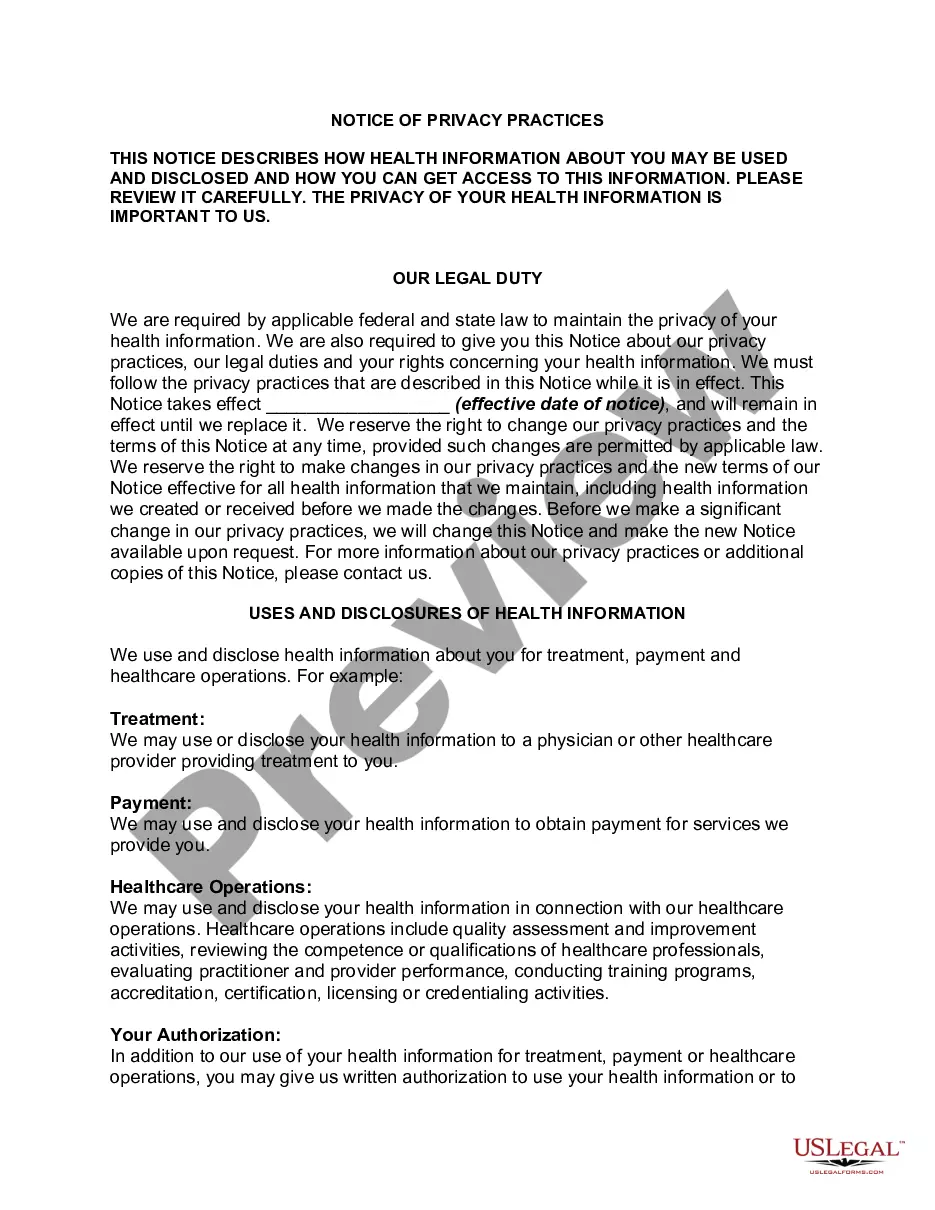
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.
Health Information Privacy Protection Act of 2013 - Prohibits the enrollment of any individual in a qualified health plan offered in a state through an American Health Benefit Exchange under the Patient Protection and Affordable Care Act until the state certifies to the Secretary of Health and Human Services (HHS), and
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
HIPAA was enacted to provide a strict confidentiality law and limit disclosure of information that could reveal a patient's identity.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that required the creation of national standards to protect sensitive patient health information from being disclosed without the patient's consent or knowledge.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that required the creation of national standards to protect sensitive patient health information from being disclosed without the patient's consent or knowledge.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the