COBRA Continuation Coverage Election Notice
Description
What Is COBRA Continuation Coverage?
COBRA Continuation Coverage is a federal mandate that allows employees and their families to continue their health insurance when they experience a qualifying event, such as job loss or reduced hours. This important provision ensures that those adversely affected do not lose their health benefits immediately.
Qualified beneficiaries may include:
- The employee who was covered under the group health plan.
- The employee's spouse.
- Dependent children.
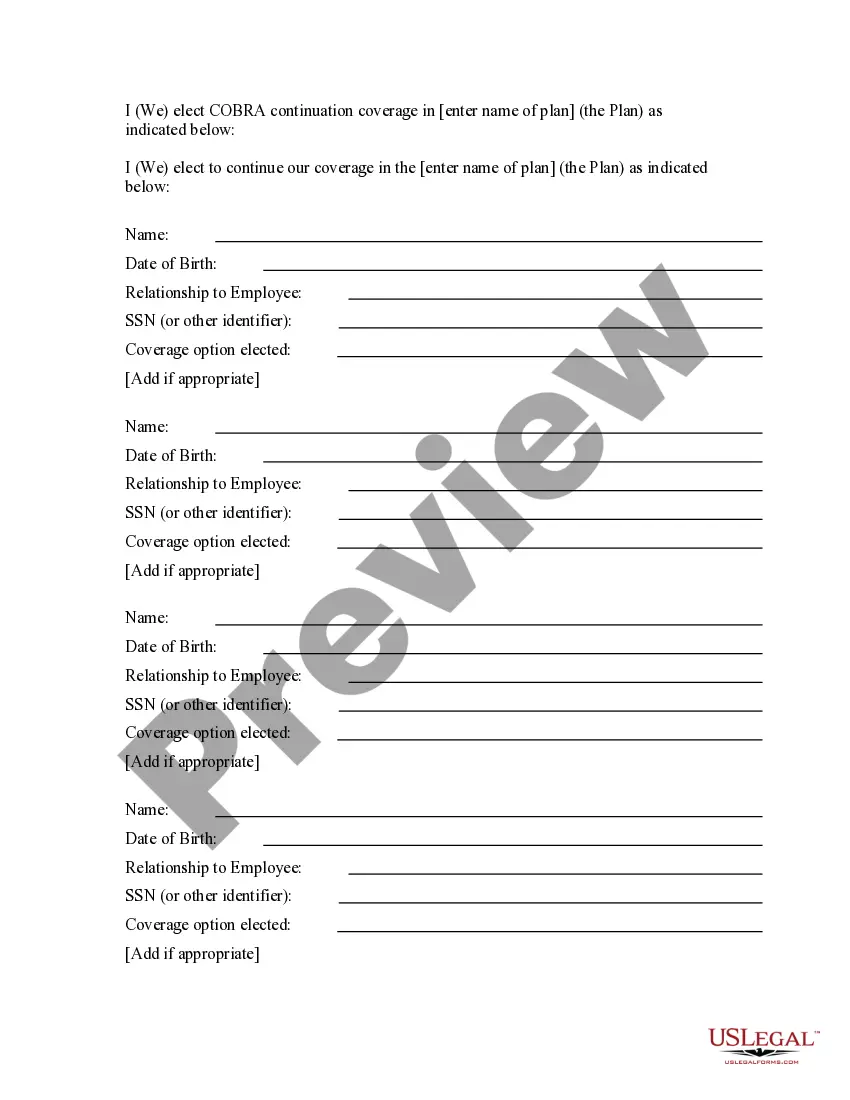
Steps to Fill Out the Election Form
Completing the COBRA Continuation Coverage Election Form is essential for maintaining your health insurance coverage. Follow these steps to ensure proper submission:
- Begin by filling out your personal information, including your name, date of birth, and relationship to the employee.
- Select the coverage option you wish to continue.
- Include the necessary social security number or other identifier.
- Sign the form and enter your contact details at the end.
Make sure to send the completed form to the specified address, post-marked by the due date provided in your notice.
Eligibility for COBRA Benefits
This form is intended for individuals who have lost their health insurance coverage due to specific qualifying events, including:
- End of employment.
- Reduction in hours of employment.
- Death of the employee.
- Divorce or legal separation.
- Enrollment in Medicare.
- Child aging out of dependent status.
Each of these events triggers the right to elect COBRA continuation coverage for eligible family members.
Understanding Your Rights Under COBRA
COBRA is governed by federal law and ensures that group health plans provide continuation coverage options to employees and their families. As mandated by the Consolidated Omnibus Budget Reconciliation Act (COBRA), this law requires that employees be informed of their right to health coverage upon the occurrence of a qualifying event.
Understanding this legal framework is crucial for beneficiaries to protect their health insurance rights and make informed decisions.
What Comes with the COBRA Election Notice?
The COBRA Election Notice consists of several vital components that detail your rights:
- Date of notice
- Details of the Plan
- Instructions on how to elect coverage
- Deadlines for electing coverage
- Payment information for coverage
Each of these elements is critical for ensuring that you navigate the continuation coverage process correctly.
Avoiding Errors on Your Election Form
When completing the COBRA Election Form, avoid common pitfalls to ensure your coverage remains intact:
- Missing the submission deadline. Be aware of the due dates.
- Inaccurate personal information can lead to processing delays.
- Failing to include all qualified beneficiaries can impact your coverage.
- Not signing the form or neglecting to provide contact information.
By being mindful of these mistakes, you can prevent potential issues with your COBRA coverage.
Understanding COBRA Payment Requirements
To continue your COBRA coverage, it is crucial to understand the payment structure:
- Each qualified beneficiary may be required to pay up to 102 percent of the cost of the coverage.
- Your first payment must be made within 45 days of electing coverage.
- Subsequent payments should be made on time to avoid interruption of coverage.
Review your payment options and confirm the amounts required with the Plan Administrator to maintain your coverage.
How to fill out COBRA Continuation Coverage Election Notice?
Among lots of free and paid samples that you’re able to get online, you can't be certain about their accuracy. For example, who created them or if they are qualified enough to take care of the thing you need them to. Always keep calm and utilize US Legal Forms! Discover COBRA Continuation Coverage Election Notice samples created by skilled legal representatives and get away from the expensive and time-consuming procedure of looking for an lawyer or attorney and then having to pay them to draft a papers for you that you can easily find yourself.
If you have a subscription, log in to your account and find the Download button next to the form you’re trying to find. You'll also be able to access all your earlier saved files in the My Forms menu.
If you’re making use of our platform the very first time, follow the instructions below to get your COBRA Continuation Coverage Election Notice fast:
- Make certain that the document you find is valid where you live.
- Review the file by reading the description for using the Preview function.
- Click Buy Now to start the ordering process or find another example using the Search field in the header.
- Choose a pricing plan and create an account.
- Pay for the subscription using your credit/debit/debit/credit card or Paypal.
- Download the form in the needed file format.
Once you have signed up and purchased your subscription, you can use your COBRA Continuation Coverage Election Notice as many times as you need or for as long as it remains valid where you live. Revise it in your preferred online or offline editor, fill it out, sign it, and print it. Do much more for less with US Legal Forms!
Form popularity
FAQ
The insurance company. COBRA Election Notice. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. The election notice describes their rights to continuation coverage and how to make an election.
Notices properly mailed are generally considered provided on the date sent, regardless of whether they're actually received. 1. COBRA Initial Notice must be provided. Within 30 days after the employee first becomes enrolled in the group health plan.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
1. You never received your COBRA enrollment packet. Contact your former employer or your health plan administrator.Your former employer must notify your health plan administrator within 30 days after your "qualifying event" death, job termination, reduced hours of employment or eligibility for Medicare.
An employer that is subject to COBRA requirements is required to notify its group health plan administrator within 30 days after an employee's employment is terminated, or employment hours are reduced.
Plan Administrator has 14 days to provide a COBRA election notice to the former employee/qualified beneficiary. Qualified beneficiary has 60 days from the date of the notification to make an election to continue enrollment in the plan(s). Qualified beneficiary has 45 days to pay the first premium.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The employer must notify the plan within 30 days of the event. You (the covered employee or one of the qualified beneficiaries) must notify the plan if the qualifying event is divorce, legal separation, or a child's loss of dependent status under the plan.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.