Texas COBRA Continuation Coverage Election Form
Description
How to fill out COBRA Continuation Coverage Election Form?
US Legal Forms - one of the largest collections of legal documents in America - offers a range of legal template options you can download or print.
By utilizing the website, you can find thousands of forms for business and personal purposes, categorized by types, states, or keywords. You can access the latest versions of forms such as the Texas COBRA Continuation Coverage Election Form in moments.
If you already have a subscription, Log In and download the Texas COBRA Continuation Coverage Election Form from the US Legal Forms library. The Download option will be visible for every form you view. You can access all previously saved forms from the My documents section of your account.
Make any necessary changes. Fill out, edit, print, and sign the downloaded Texas COBRA Continuation Coverage Election Form.
Any template you add to your account has no expiration date and is yours indefinitely. Therefore, if you wish to download or print another copy, simply navigate to the My documents section and click on the form you need. Access the Texas COBRA Continuation Coverage Election Form through US Legal Forms, which is the most comprehensive library of legal document templates. Utilize countless professional and state-specific templates that cater to your business or personal requirements.
- If you're using US Legal Forms for the first time, here are simple instructions to get you started.
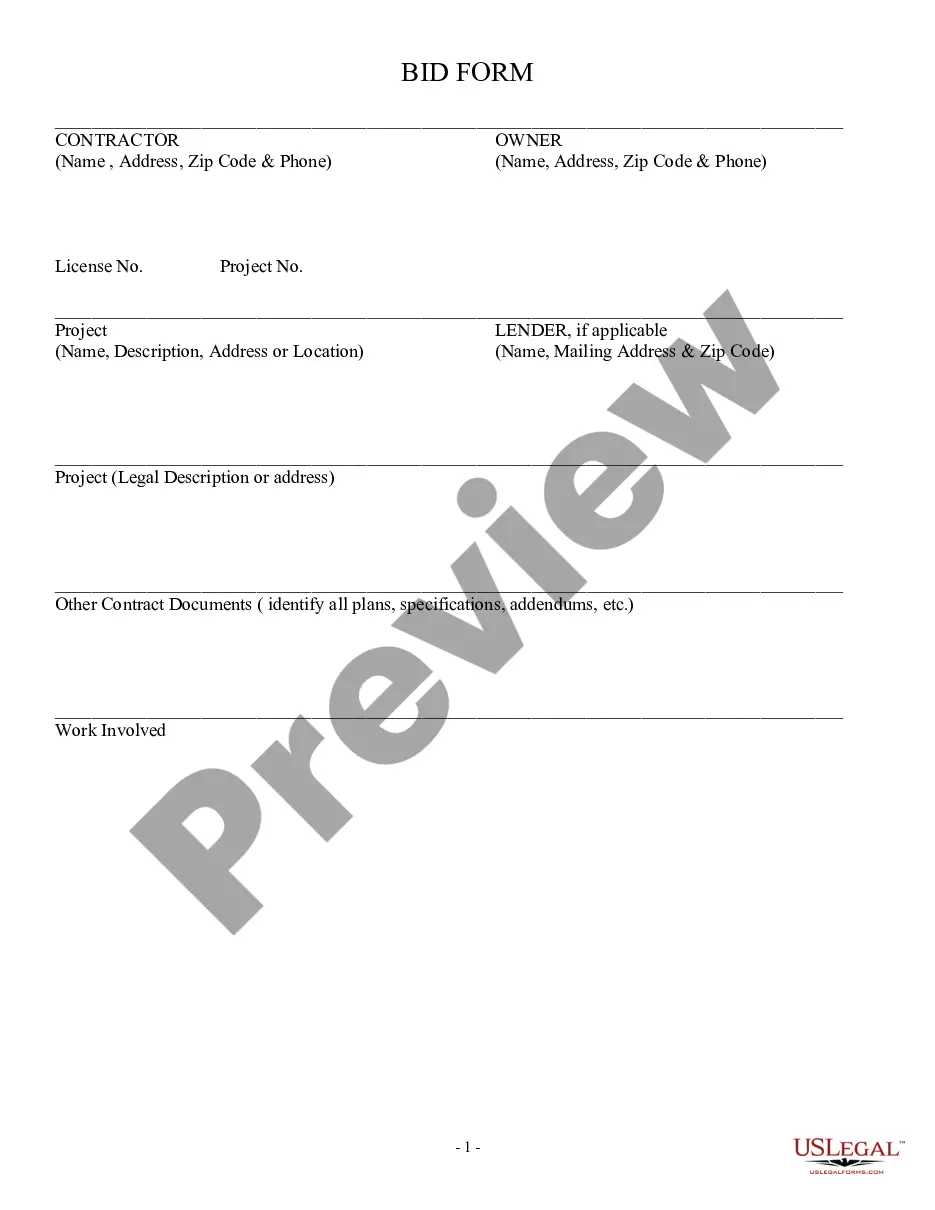
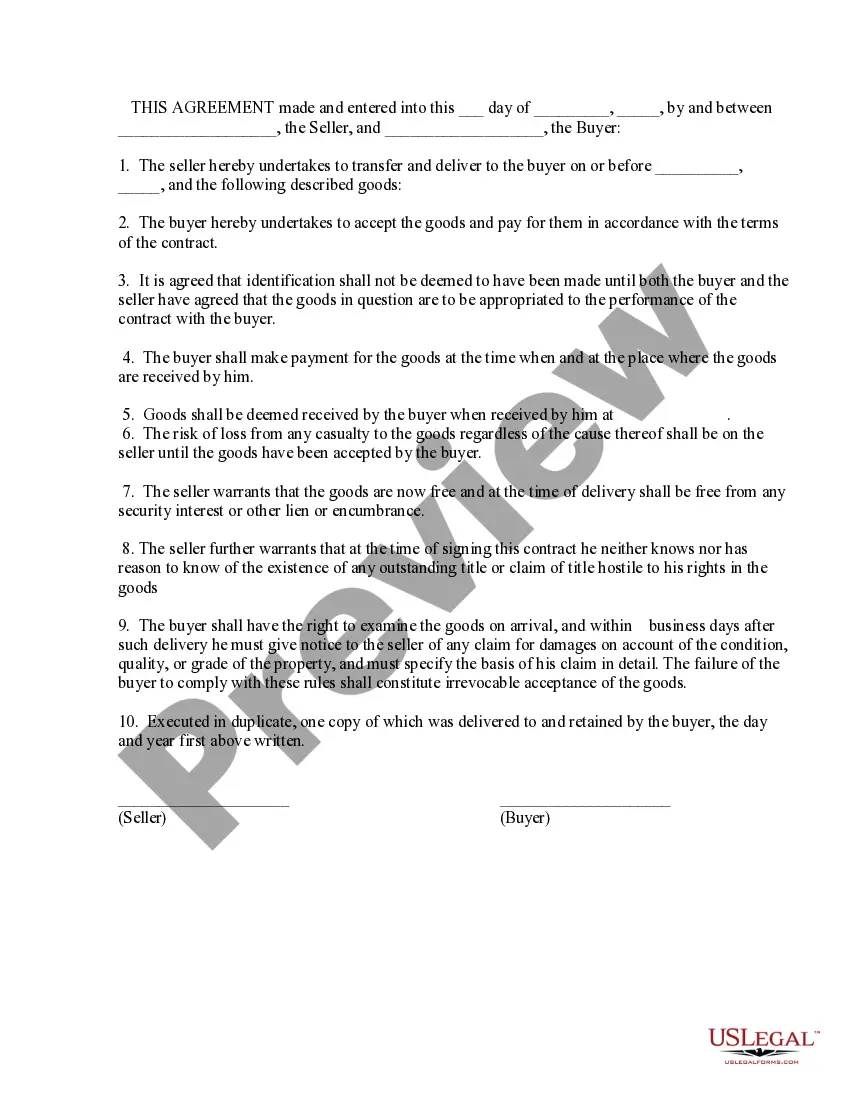
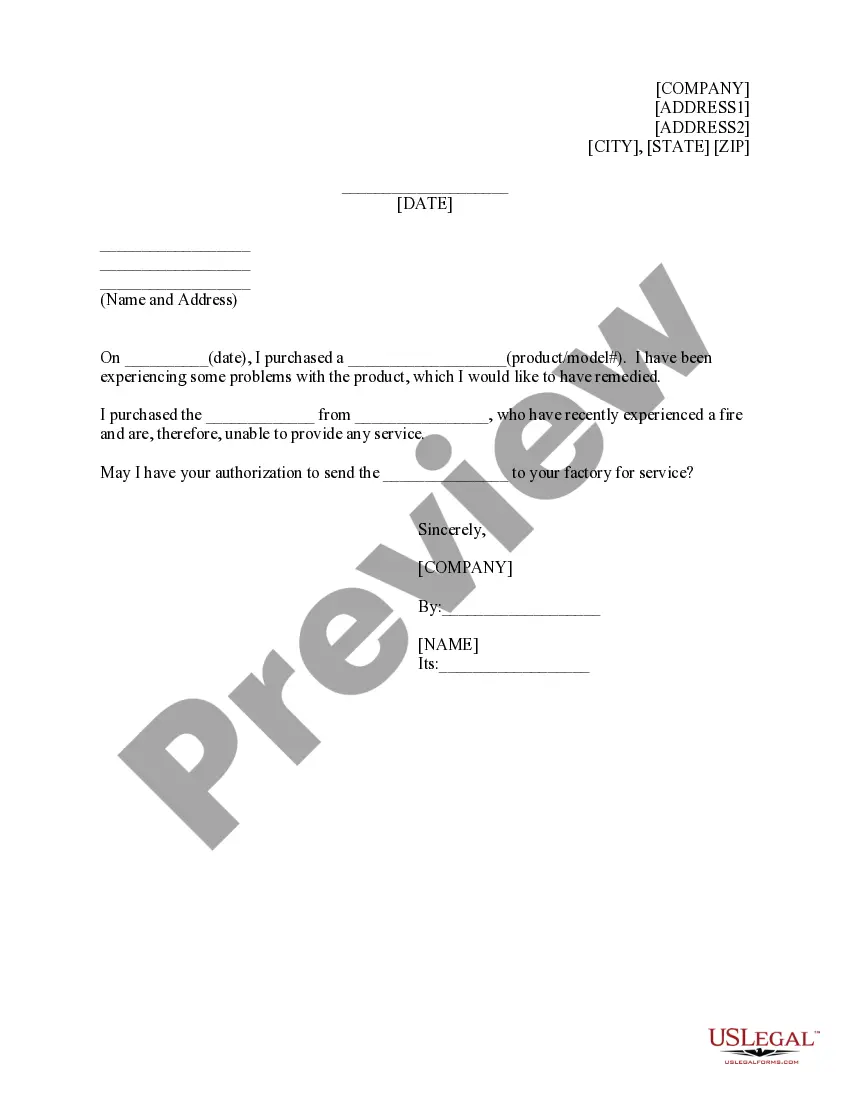
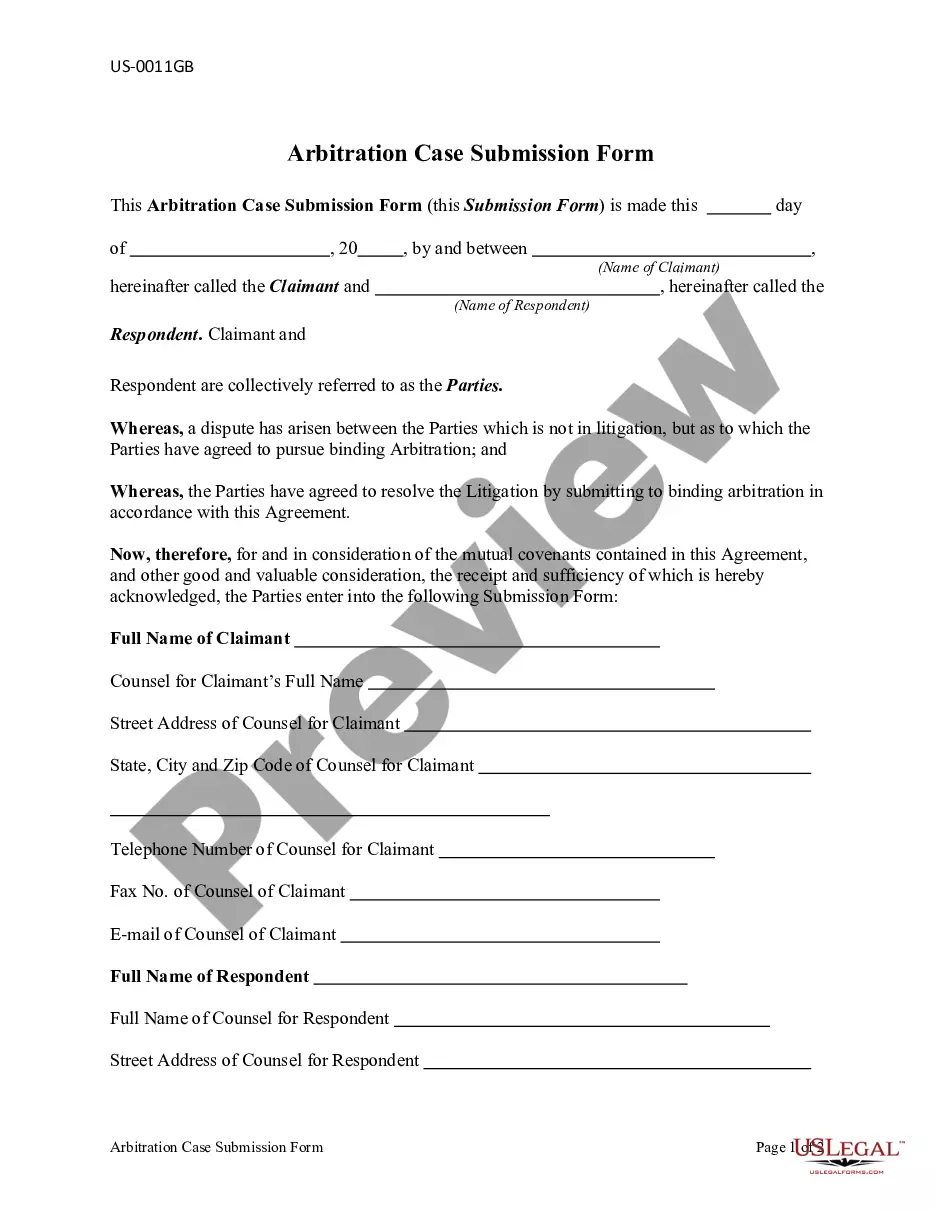
- Ensure you’ve selected the correct form for your city/region. Click the Preview button to review the contents of the form. Read the form description to confirm you’ve chosen the correct one.
- If the form doesn’t meet your needs, use the Search box at the top of the page to find one that does.
- If you’re happy with the form, confirm your choice by clicking the Buy Now button. Then select the payment plan you prefer and enter your information to create an account.
- Complete the transaction. Use your Visa, Mastercard, or PayPal account to process the payment.
- Choose the file format and download the form to your device.
Form popularity
FAQ
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Texas's COBRA LawTexas has its own mini-COBRA law. The Small Employer Health Insurance Availability Act grants employees insurance continuation rights if the company has 2 to 50 employees.
Texas regulations require continuation coverage for a period of 9 months from the date of loss of coverage if the Qualifying Event is termination.
State law allows employees of smaller employers (fewer than 20 employees) to keep the same. group health insurance coverage for up to nine months after loss of a job or loss of coverage. because of a reduction in work hours. This is called state continuation.
For groups subject to COBRA, Texas law allows an additional six (6) months of coverage after COBRA ends. The law applies only to fully insured groups. COBRA participants are eligible for the additional six (6) months of continuation coverage after 18, 29, or 36 months of COBRA coverage.
STATE CONTINUATION: If you are not eligible for COBRA or if you have exhausted your COBRA coverage, Texas law provides you with coverage continuation rights.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Under Texas state continuation, you and your family may remain covered under your former employer's health plan for up to nine months if you are not eligible for COBRA.