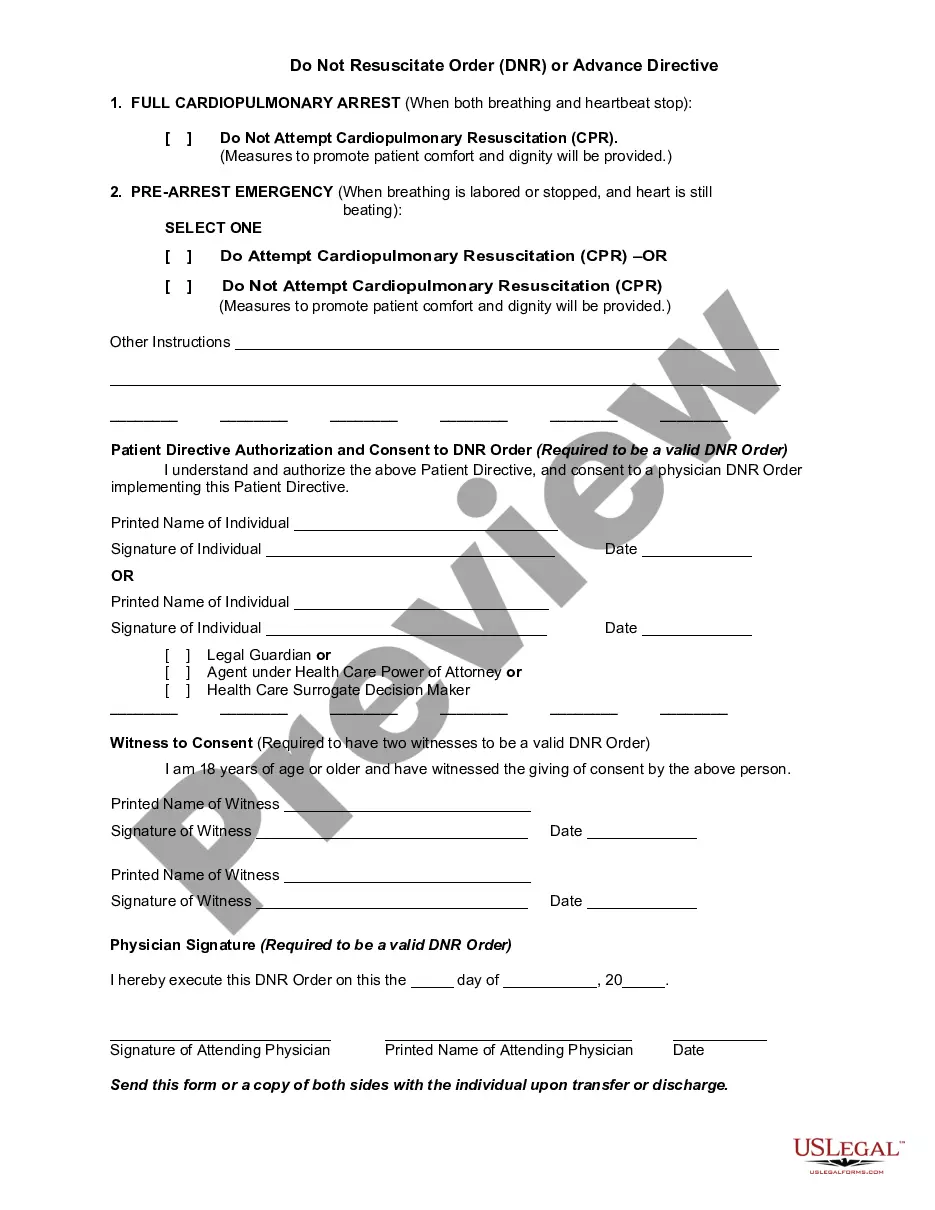
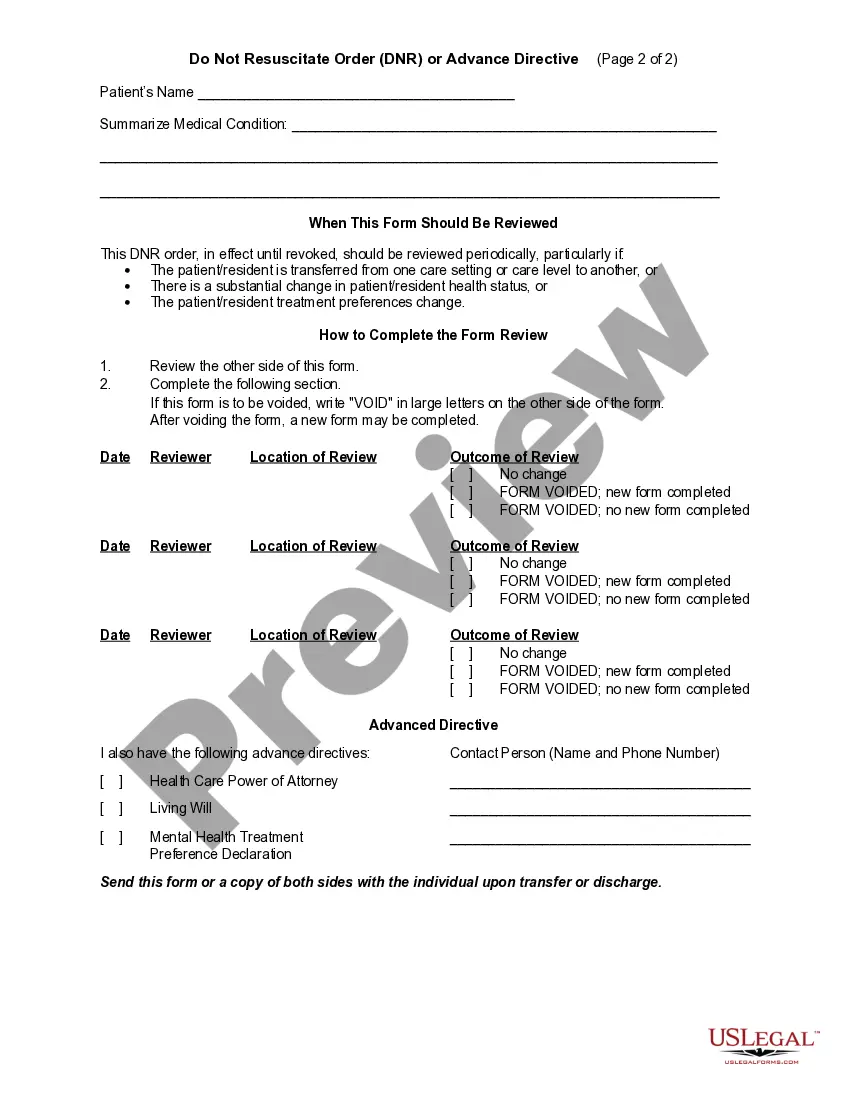
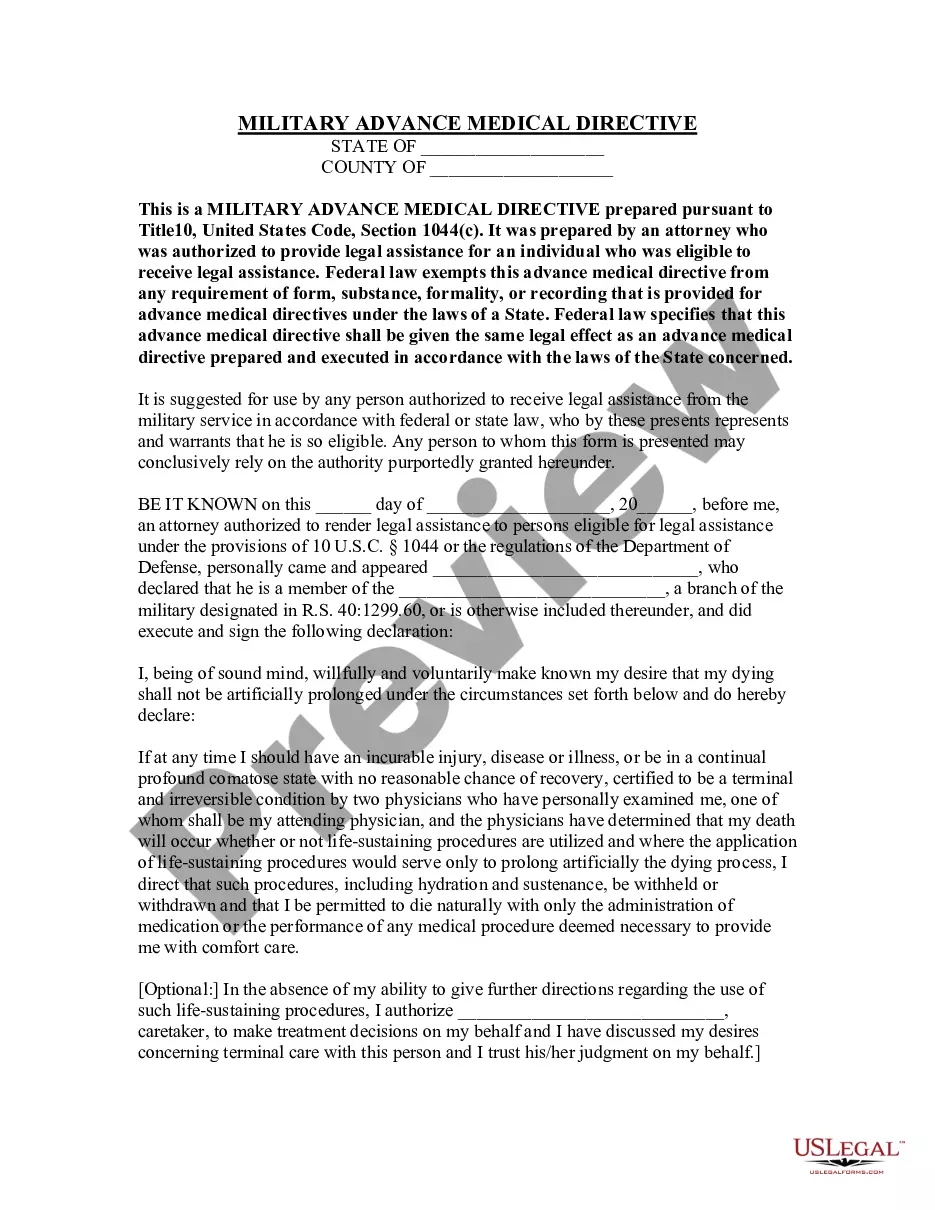
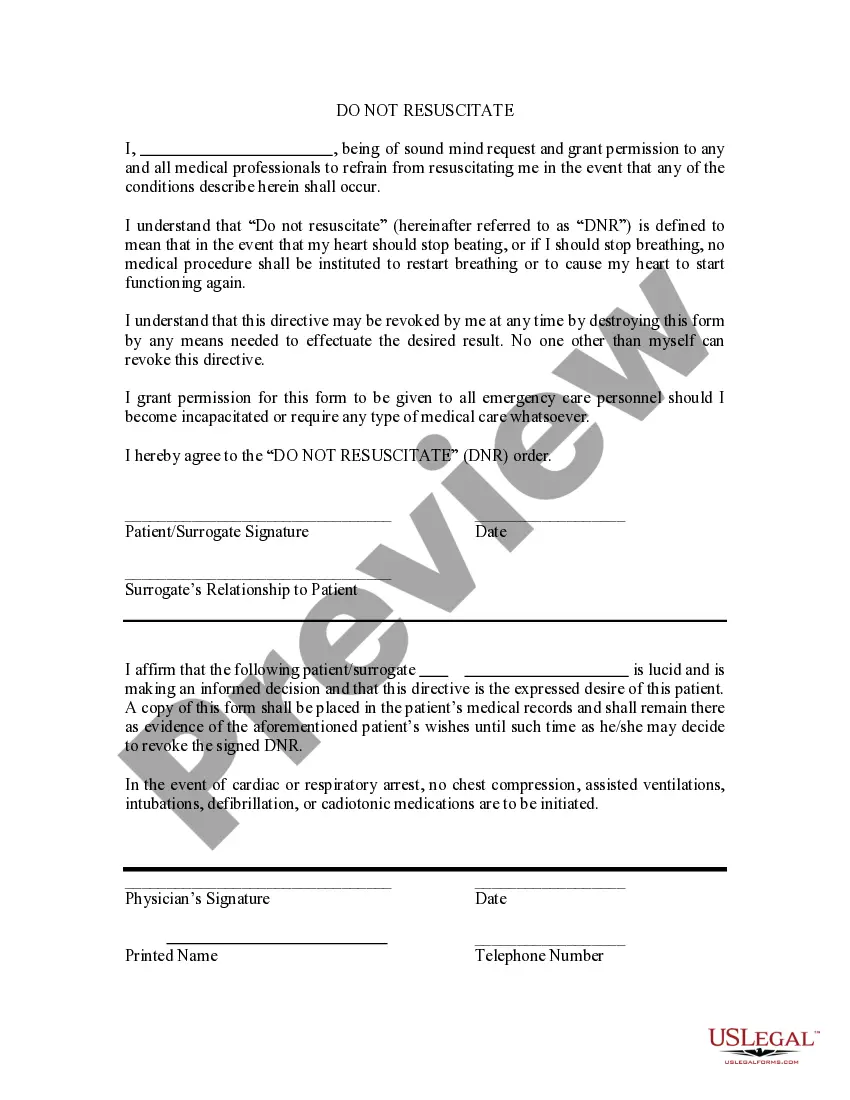
A do not resuscitate (DNR) order is a request not to have cardiopulmonary resuscitation (CPR) if your heart stops or if you stop breathing. Unless given other instructions, hospital staff will try to help all patients whose heart has stopped or who have stopped breathing. A DNR order is put in your medical chart by your doctor. DNR orders are accepted by doctors and hospitals in all states.
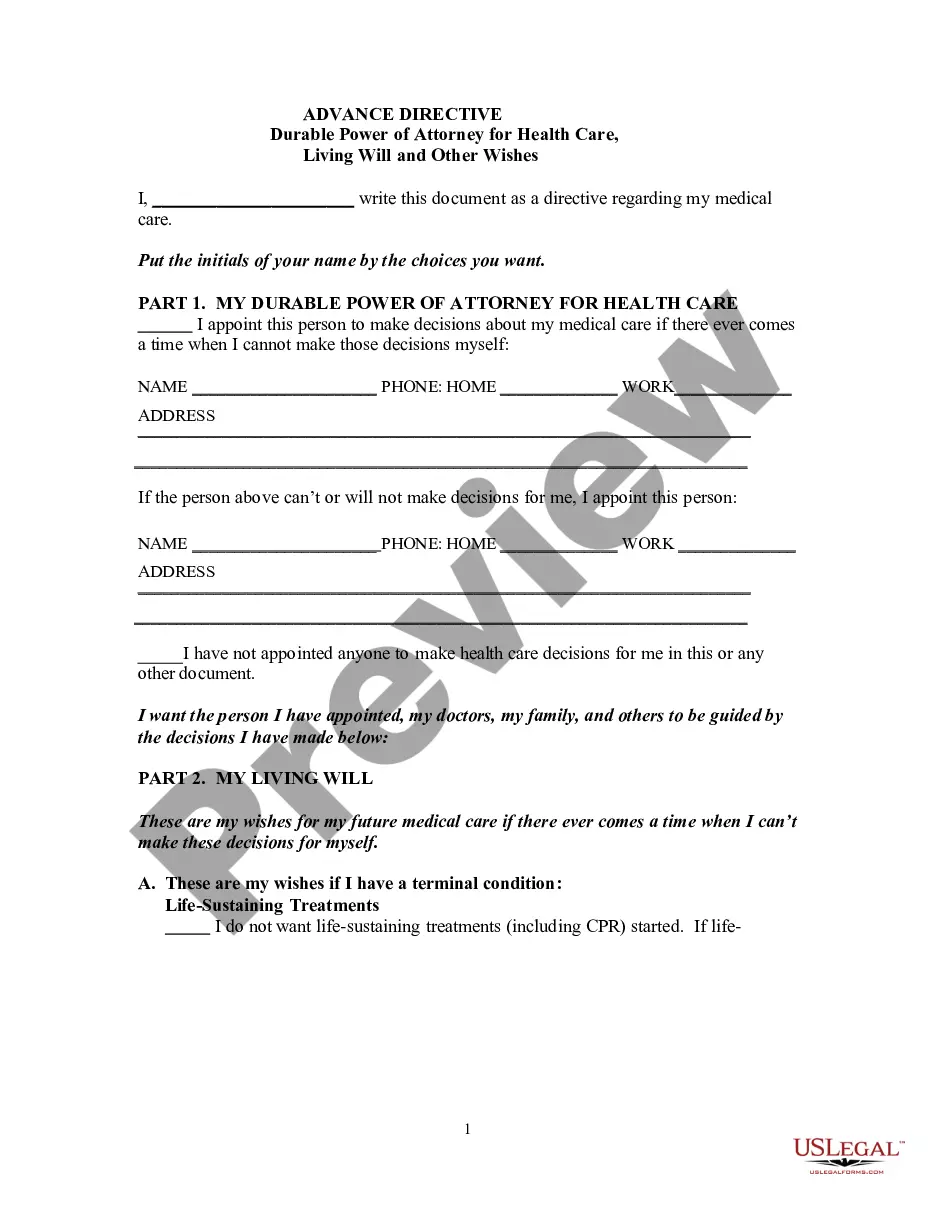
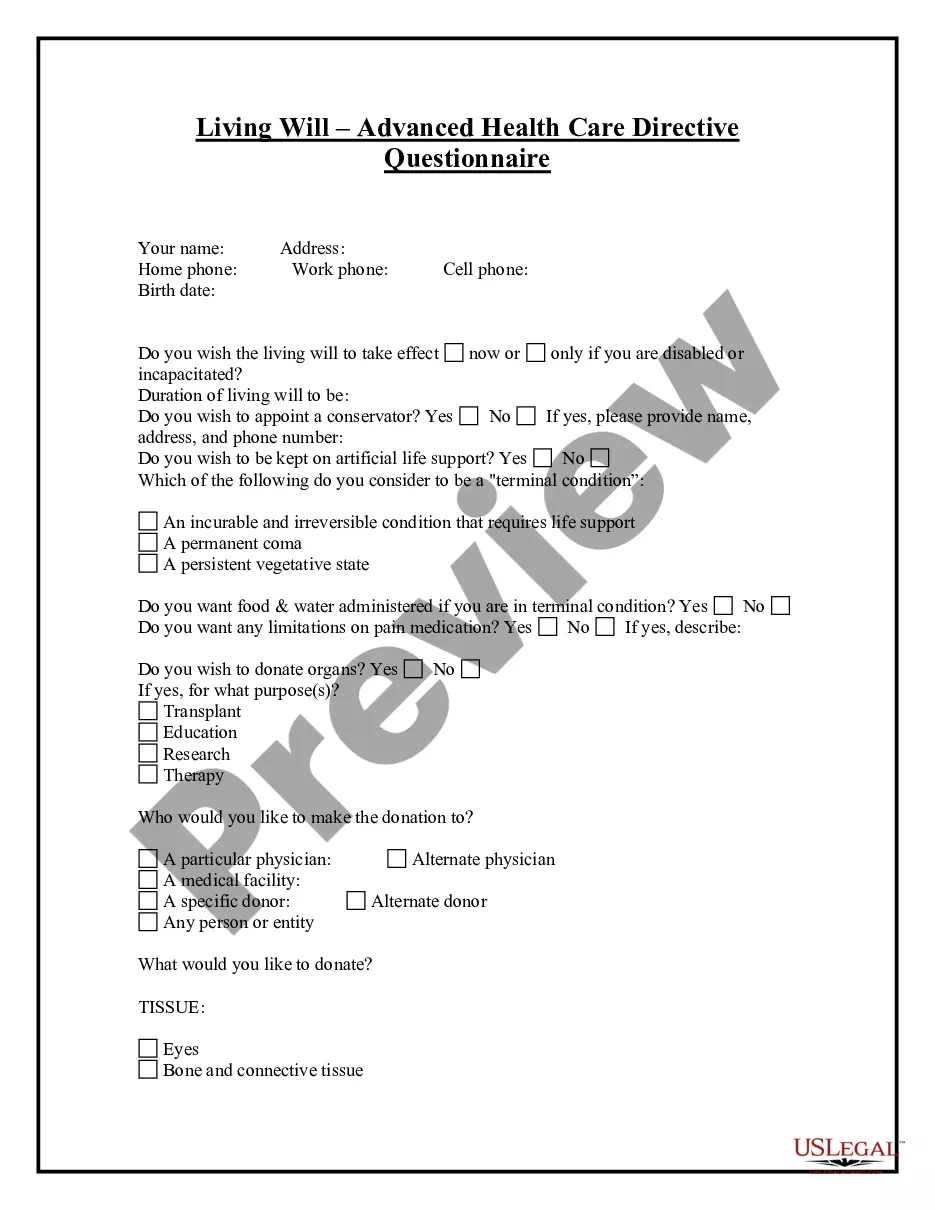
This form is a generic example that may be referred to when preparing such a form for your particular state. It is for illustrative purposes only. Local laws should be consulted to determine any specific requirements for such a form in a particular jurisdiction.