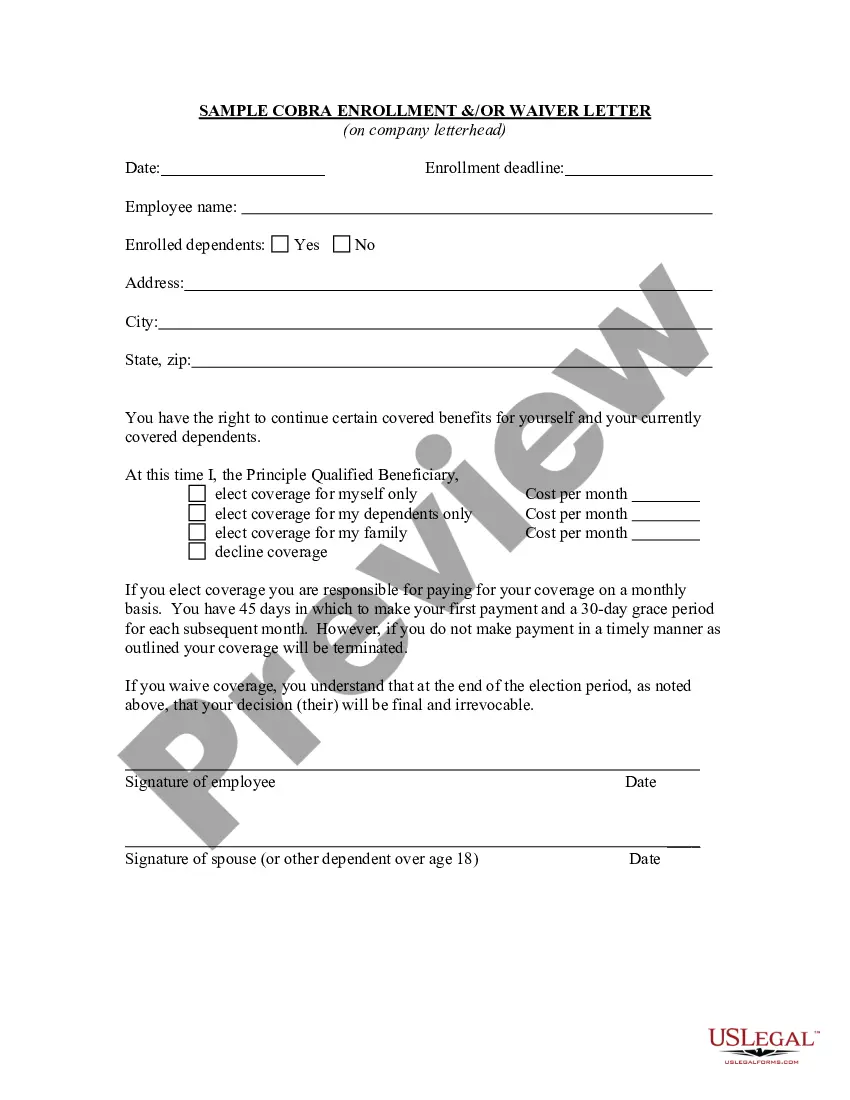
South Dakota Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
Locating the appropriate legitimate document template can be a struggle.
Of course, there are countless online templates readily available, but how will you acquire the valid form you seek.
Utilize the US Legal Forms website. The service provides a vast array of templates, such as the South Dakota Sample COBRA Enrollment and/or Waiver Letter, which can be utilized for both business and personal purposes.
You can view the form using the Review feature and read its description to verify it is suitable for you.
- All of the forms are reviewed by experts and comply with state and federal regulations.
- If you are already a registered user, Log In to your account and click on the Download button to access the South Dakota Sample COBRA Enrollment and/or Waiver Letter.
- Use your account to browse the valid documents you have previously purchased.
- Visit the My documents section of your account to obtain another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple steps for you to follow.
- First, ensure that you have chosen the correct form for your locality.
Form popularity
FAQ
Once COBRA coverage is canceled, there is no option for reinstatement. Note that waiting until the end of the grace period to make payment may not allow enough time within the grace period to reconcile payment if your check is lost in the mail or is rejected by your bank.
Draft a letter stating facts why the COBRA benefits must be reinstated. The letter must provide your full legal name, address, Social Security number and COBRA policy number. The letter should be in proper business format and is best if free from all spelling and grammatical errors.
Cal-COBRA applies to employers with 2-19 employees, whereas federal COBRA applies to employers with more than 20 employees. Cal-COBRA offers coverage for up to 36 months, while federal COBRA offers coverage for 18 months for the former employee and up to 36 months for any dependents.
Under federal COBRA, employers with 20 or more employees are usually required to offer COBRA coverage. COBRA applies to plans maintained by private-sector employers (including self-insured plans) and those sponsored by most state and local governments.
Under COBRA, a person who has been terminated for gross misconduct may be denied COBRA. Gross misconduct is not specifically defined by COBRA, but when based on an employer's practice or policy it could include misrepresentation during the hiring process or falsifying information on a Form I-9.
If you feel the non-commencement or termination of your benefits under the Federal COBRA regulations was in error, you have the right to file an appeal by writing a letter which explains why you believe the coverage should be reinstated.
If the employer's health plan administrator doesn't provide you the opportunity to elect COBRA coverage, by law, they will be fined by the US Department of Labor. When you continue on your former group health plan, you pay your portion, the subsidy the employer paid and a 2% administration fee.
Cal-COBRA applies to employers and group health plans that cover from two to 19 employees. It covers indemnity policies, preferred provider organizations (PPOs) and health maintenance organizations (HMOs), but not self-insured plans. Unlike federal COBRA, church plans are covered under Cal-COBRA.
Employers do not have to offer COBRA coverage to: Employees who are not yet eligible for a group health plan. Eligible employees who declined to participate in a group health plan. Individuals who are enrolled for benefits under Medicare.
Codified Laws Sec. 58-18-7). Continuation coverage for 18 months must be provided to employees upon leaving employment or the termination of the coverage by the insurer and their eligible dependents (S.D. Codified Laws Sec.