Pennsylvania Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
You might spend hours online searching for the proper legal document template that satisfies the state and federal regulations you require.
US Legal Forms offers thousands of legal documents that can be reviewed by professionals.
It is easy to download or print the Pennsylvania Notice of Qualifying Event from Employer to Plan Administrator from your service.
First, make sure you have selected the correct document template for your county/town of choice. Check the form outline to ensure you have chosen the appropriate form. If available, utilize the Preview button to review the document template as well.
- If you possess a US Legal Forms account, you are able to Log In and click the Download button.
- After that, you can complete, modify, print, or sign the Pennsylvania Notice of Qualifying Event from Employer to Plan Administrator.
- Every legal document template you purchase is yours permanently.
- To obtain another copy of any purchased form, go to the My documents tab and click the respective button.
- If you are using the US Legal Forms website for the first time, follow the straightforward instructions below.
Form popularity
FAQ
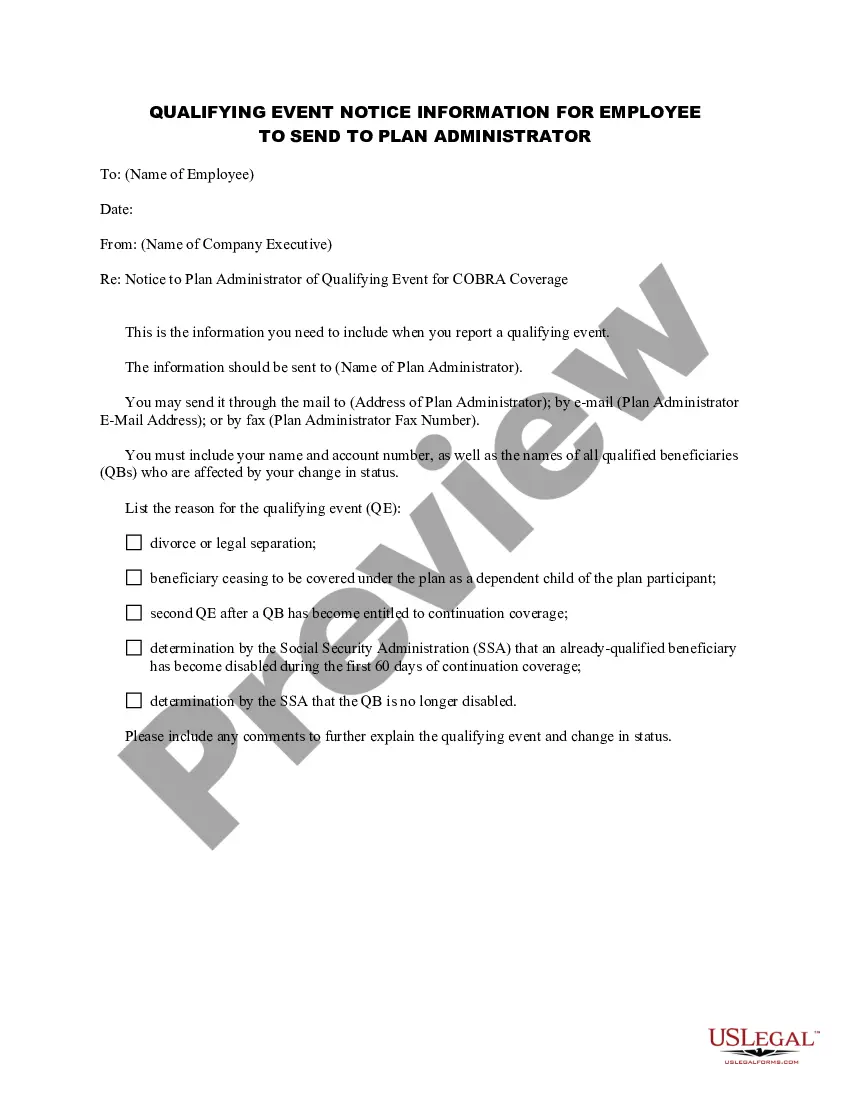
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
For disabled QBs who receive an 11-month COBRA extension (29 months in total), you can charge up to 150% of the group rate. Many states have regulations that are similar to federal COBRA. These state regulations are known as mini-COBRA.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Virginia: The Virginia mini-COBRA law provides for twelve months of continuing coverage for small businesses. The employer has an obligation to issue a notice to the employee within 14 days of learning that a person covered under the health plan is no longer eligible for coverage.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
In Pennsylvania, companies with 50 or more full-time employees must provide health insurance coverage. Businesses in Pennsylvania that have 50+ full-time employees are considered applicable large employers, which means they may face penalties if they fail to offer health benefits.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.