Pennsylvania Hospital Audit Program
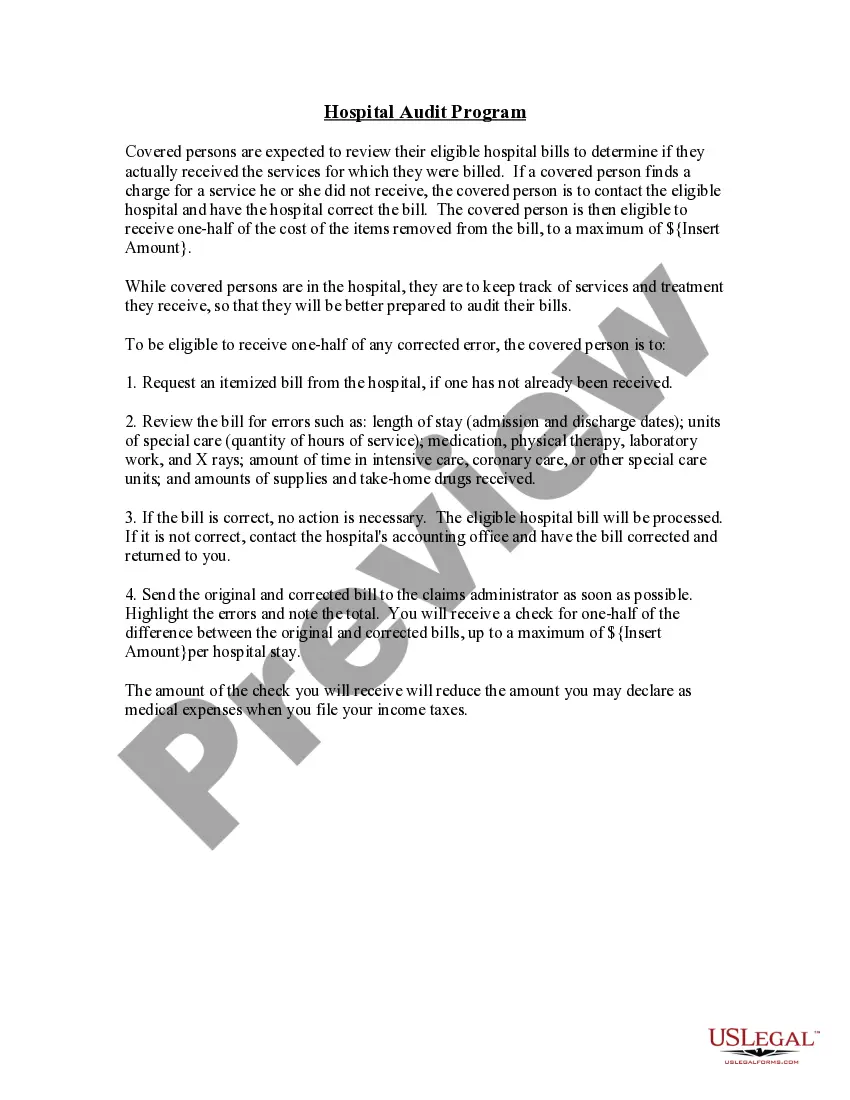
Description
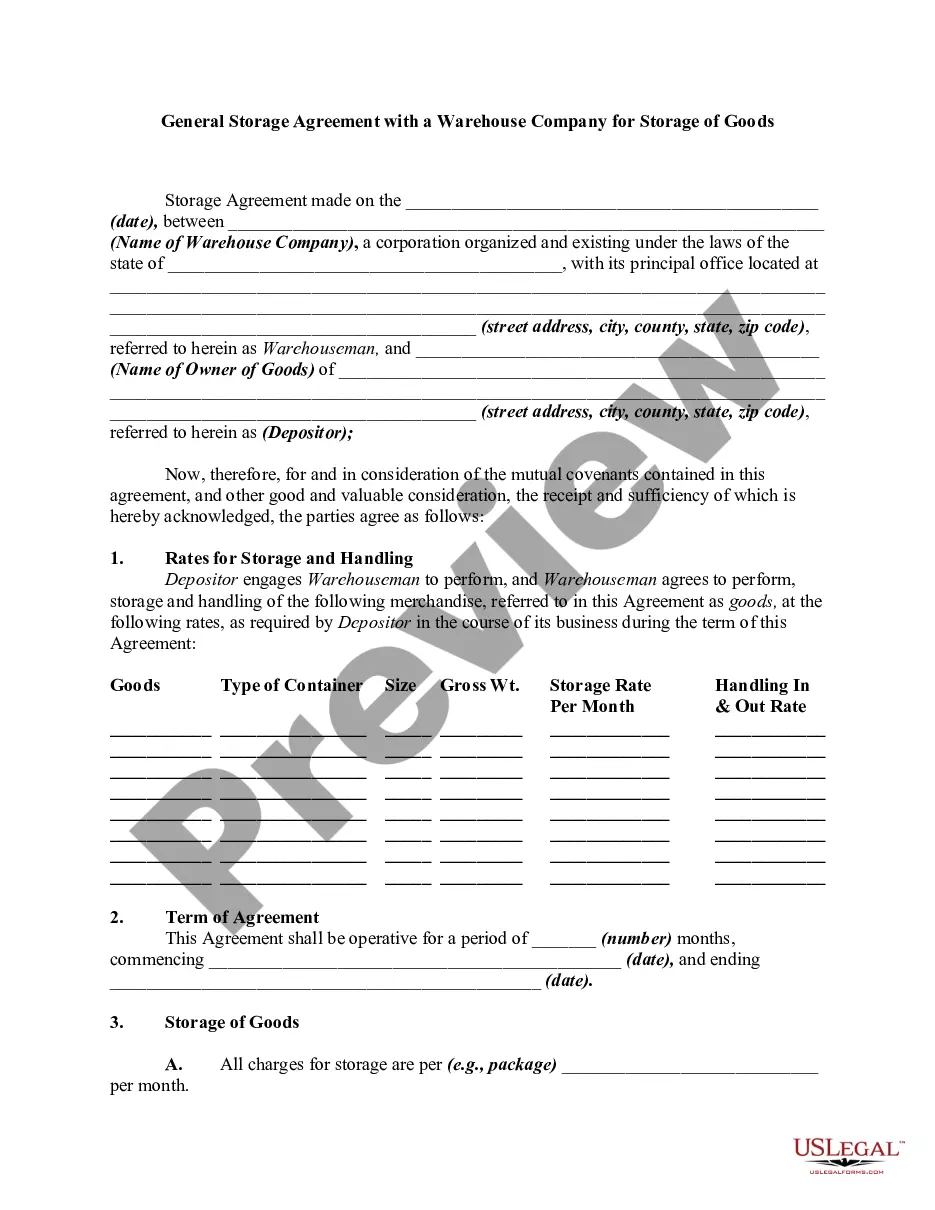
How to fill out Hospital Audit Program?
US Legal Forms - one of the most important collections of legal templates in the USA - offers a vast array of legal document templates that you can download or print.
By utilizing the website, you can discover thousands of templates for commercial and personal use, categorized by types, states, or keywords. You can access the latest versions of templates like the Pennsylvania Hospital Audit Program in just moments.
If you already possess a subscription, Log In and download the Pennsylvania Hospital Audit Program from the US Legal Forms library. The Download button will appear on each template you view. You can access all previously acquired templates in the My documents section of your account.
Complete the payment. Use your credit card or PayPal account to finalize the transaction.
Select the format and download the template to your device. Edit. Complete, modify, and print/sign the downloaded Pennsylvania Hospital Audit Program. Each template added to your account has no expiration date and is yours forever. Thus, if you want to download or print another copy, simply visit the My documents section and click on the template you require. Access the Pennsylvania Hospital Audit Program with US Legal Forms, the most extensive collection of legal document templates. Utilize a multitude of professional and state-specific templates that fulfill your commercial or personal needs and requirements.
- Ensure you have selected the correct template for your area/region.
- Click the Preview button to examine the form's content.
- Review the form description to verify that you have chosen the right template.
- If the template does not fit your needs, utilize the Search field at the top of the screen to find one that does.
- Once you are satisfied with the form, confirm your selection by clicking the Get now button.
- Then, select your preferred pricing plan and provide your information to register for an account.
Form popularity
FAQ
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
Audit of Income of HospitalsBills should be verified with the fees/charges structure. Concession and waiver on account of fees and other charges should be verified. Bills should be verified with cash receipt book, counterfoil of receipts and cash book. Verification of arrears of bills should be done.
Recovery Auditors who choose to review a provider using their Adjusted ADR limit must review under a 6-month look-back period, based on the claim paid date.
Civil monetary penalties (CMPs) of up to $1,000,000 as adjusted annually2 may be imposed on reporting entities if they fail to report information in a timely, accurate, or complete manner.
What Triggers a Medicare Audit? A key factor that often triggers an audit is claiming reimbursement for a higher than usual frequency of services over a period of time compared to other health professionals who provide similar services.
Medicare RACs perform audit and recovery activities on a postpayment basis, and claims are reviewable up to three years from the date the claim was filed.
RACs review claims on a post-payment basis and will be able to look back three years from the date the claim was paid.
Feff CMS program audits are intended to measure a sponsoring organizationsMedicare Advantage Organizations (MAOs), Prescription Drug Plans (PDPs), and Medicare-Medicaid Plans (MMPs) compliance with all Medicare Parts C and D program requirements.
Recovery Auditors who choose to review a provider using their 0.5% baseline annual ADR limit may review under a 3-year look-back period, per CMS approval.
After the provider submits the requested universes, auditors will assess the data provided and determine whether any other information is necessary. This phase will last six weeks. Field work by auditors - Auditors will conduct webinar audits and evaluate sample data from the submitted universes.