Oregon Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
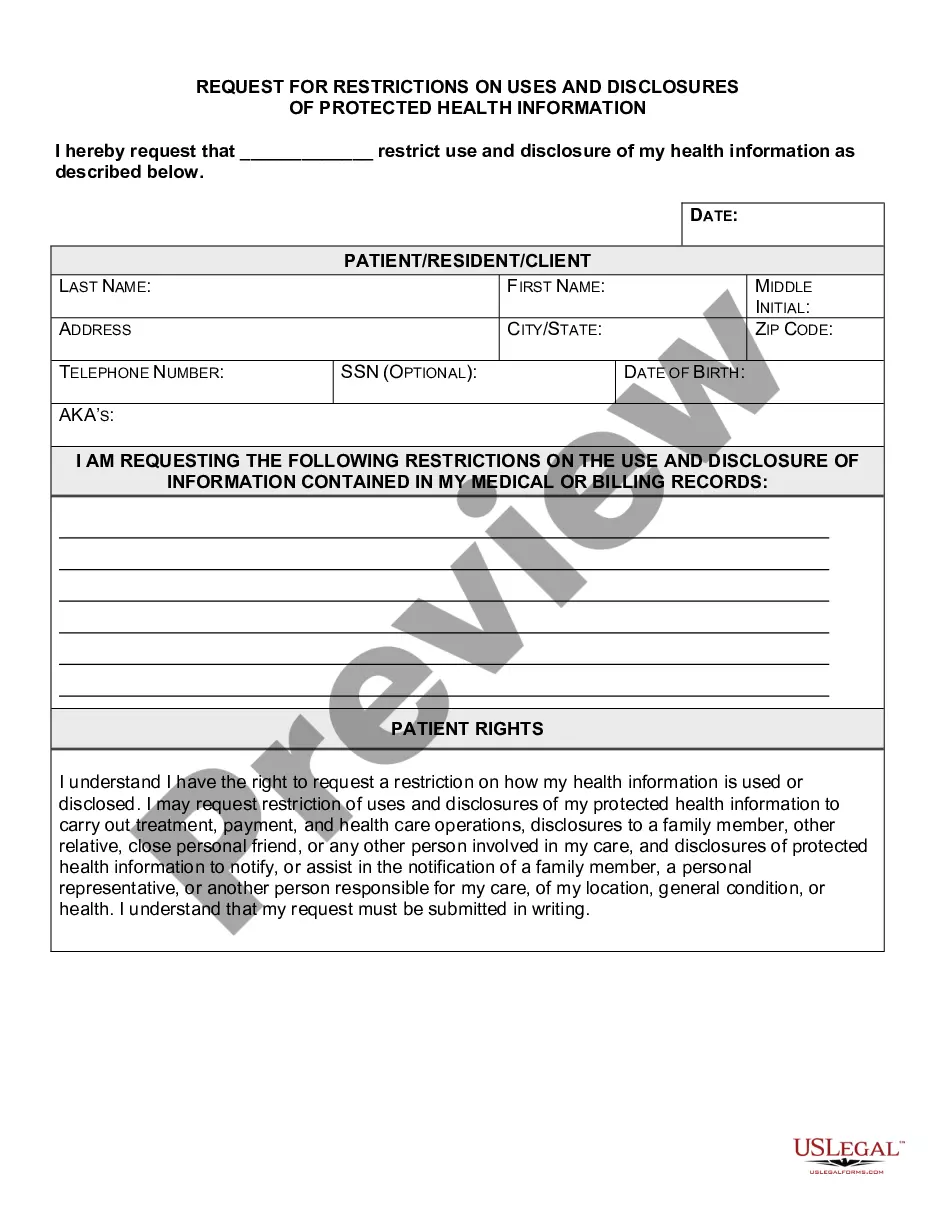
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
If you need to thoroughly review, download, or create legal document templates, utilize US Legal Forms, the largest collection of legal forms accessible online.
Employ the site’s straightforward and convenient search feature to find the documents you require.
Many templates for business and personal purposes are organized by categories and states, or keywords.
Step 4. Once you find the form you need, click the Buy now button. Choose the payment plan you prefer and enter your credentials to create an account.
Step 5. Complete the payment process. You may use your credit card or PayPal account to finalize the transaction.
- Use US Legal Forms to obtain the Oregon Request for Limitations on Uses and Disclosures of Protected Health Information in just a few clicks.
- If you are a current US Legal Forms member, Log In to your account and click the Download button to acquire the Oregon Request for Limitations on Uses and Disclosures of Protected Health Information.
- You can also access forms you previously saved in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow these directions.
- Step 1. Confirm you have selected the form for your specific city/state.
- Step 2. Use the Preview option to review the form’s content. Don’t forget to read the details.
- Step 3. If you are dissatisfied with the form, use the Search field at the top of the screen to find alternative versions of the legal document format.
Form popularity
FAQ
Yes, a covered entity can refuse a request to restrict PHI disclosures to health plans, even if the individual pays in full out of pocket. However, if a patient pays for a service completely and requests a restriction, the entity must comply. Understanding your rights under the Oregon Request for Restrictions on Uses and Disclosures of Protected Health Information can empower you in these situations. Consider consulting uslegalforms for specialized guidance on making effective requests.
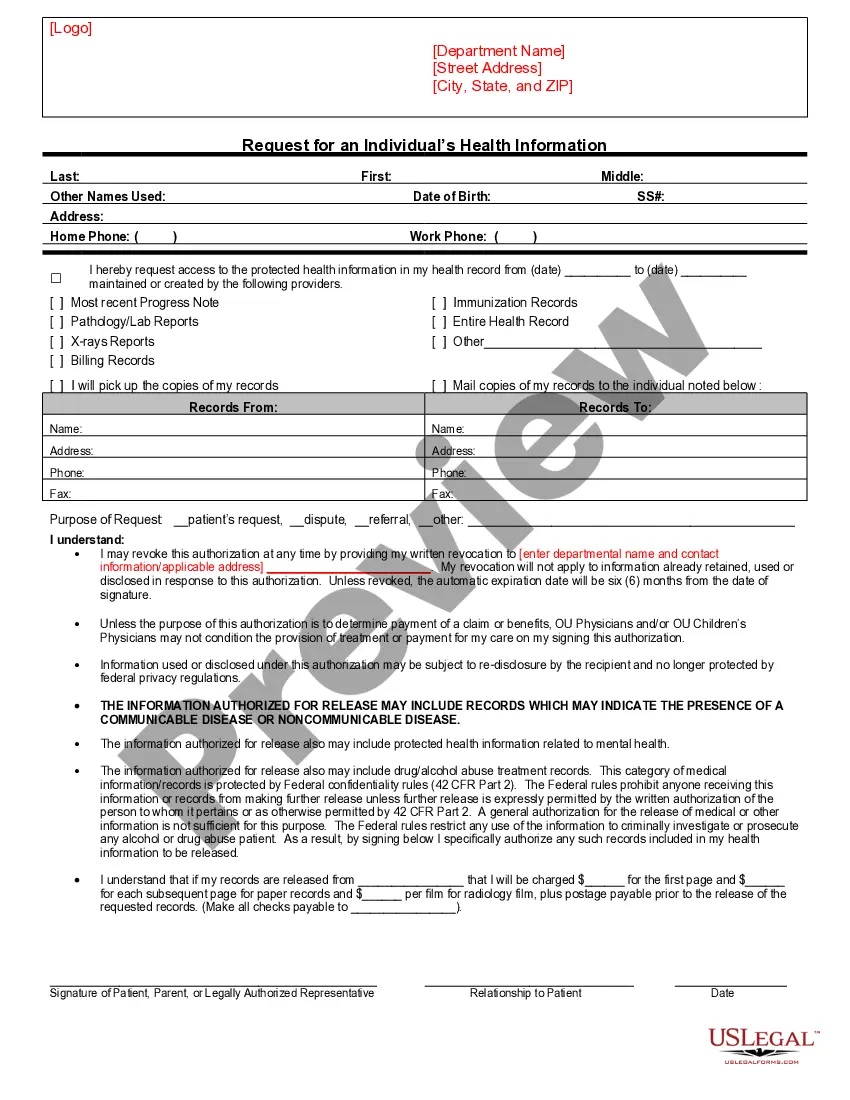
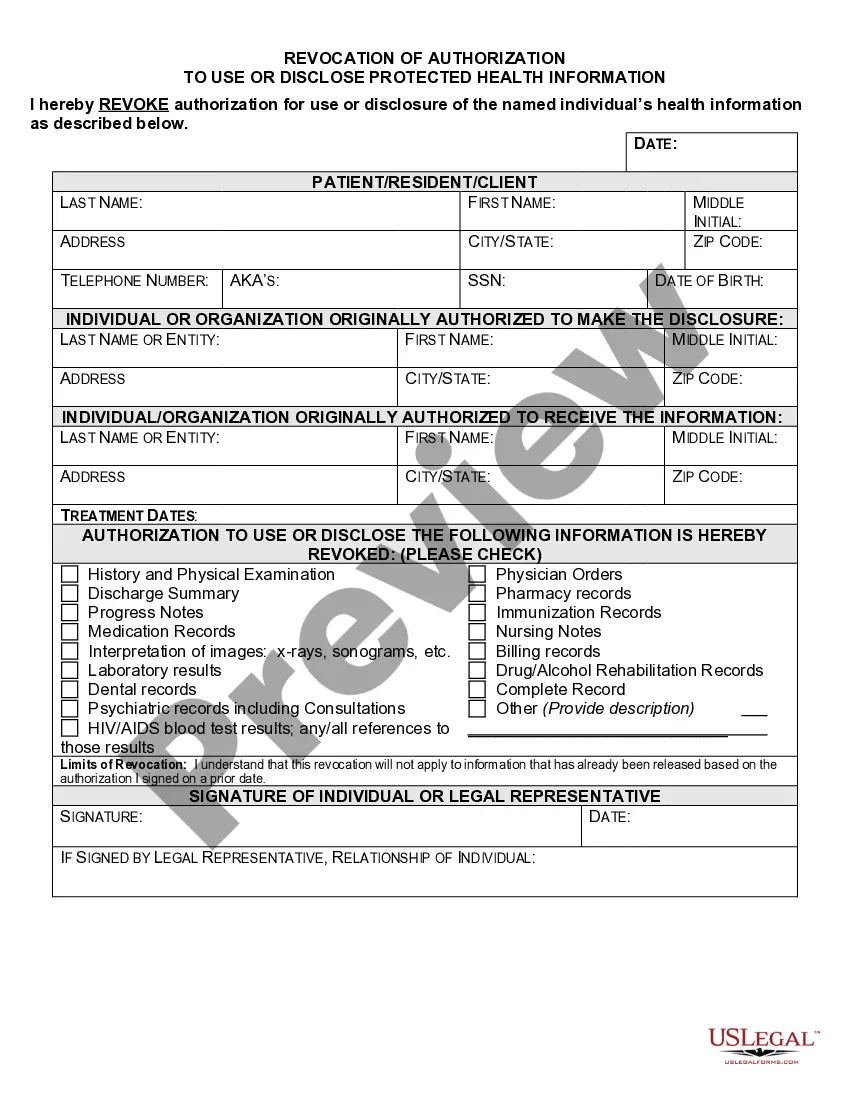
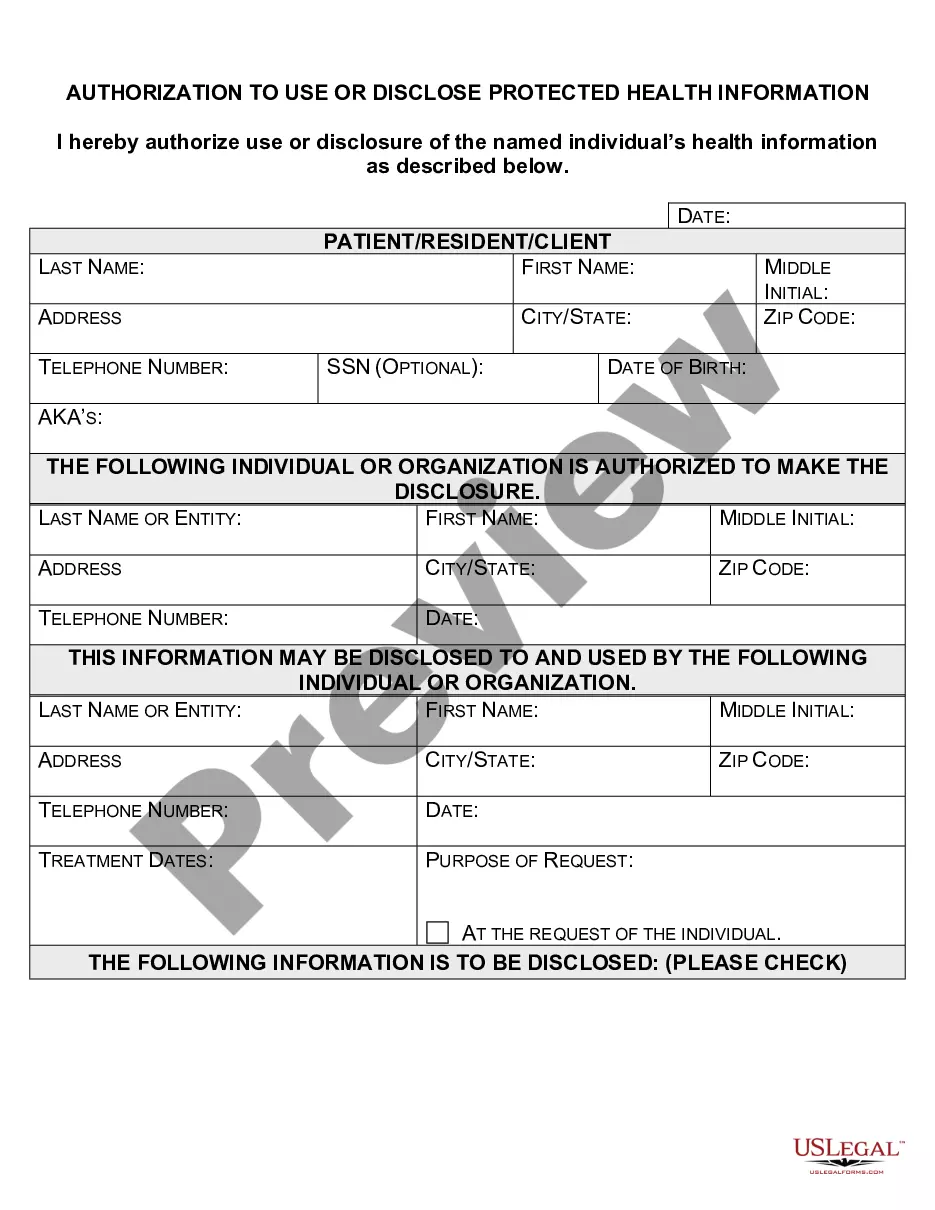
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
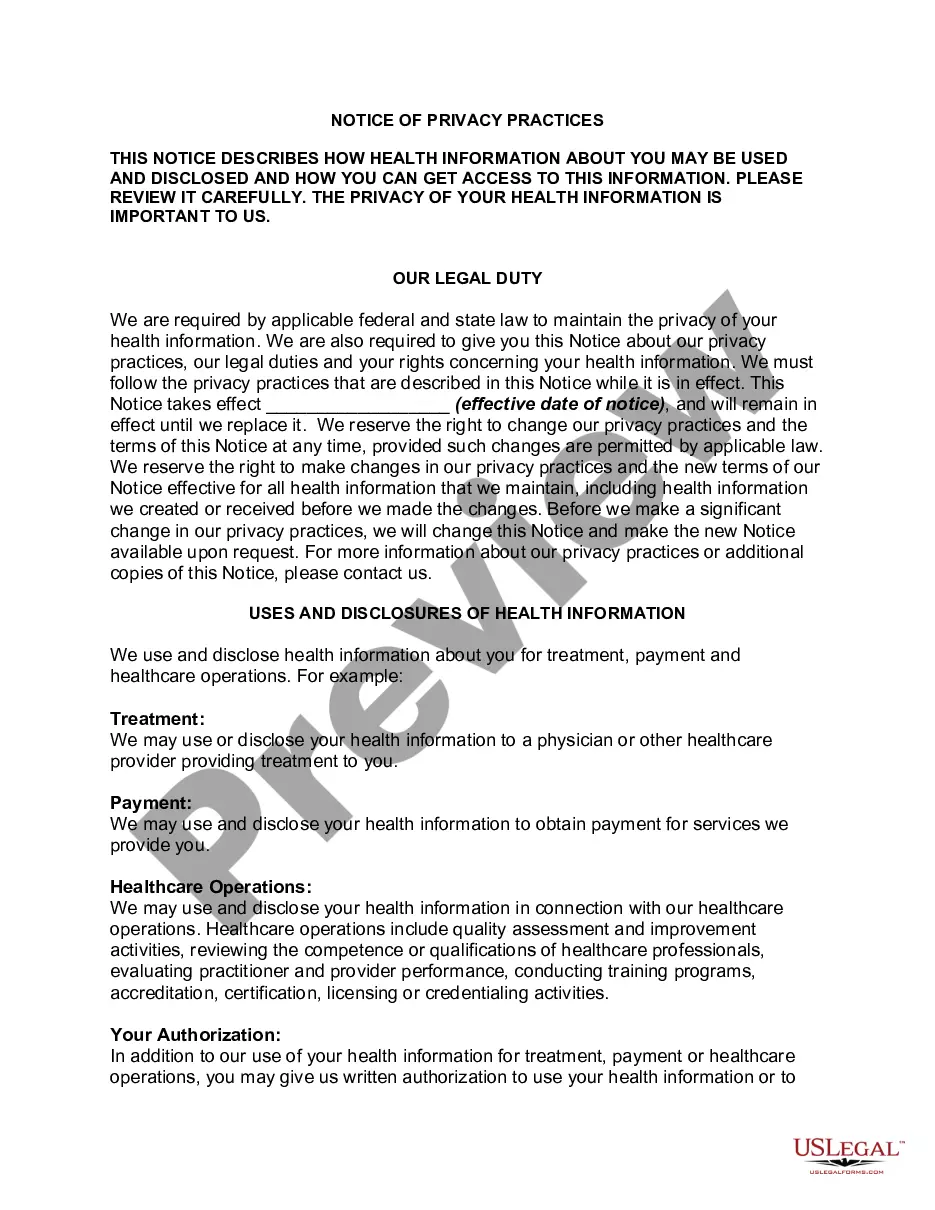
A covered entity must obtain the individual's written authorization for any use or disclosure of protected health information that is not for treatment, payment or health care operations or otherwise permitted or required by the Privacy Rule.
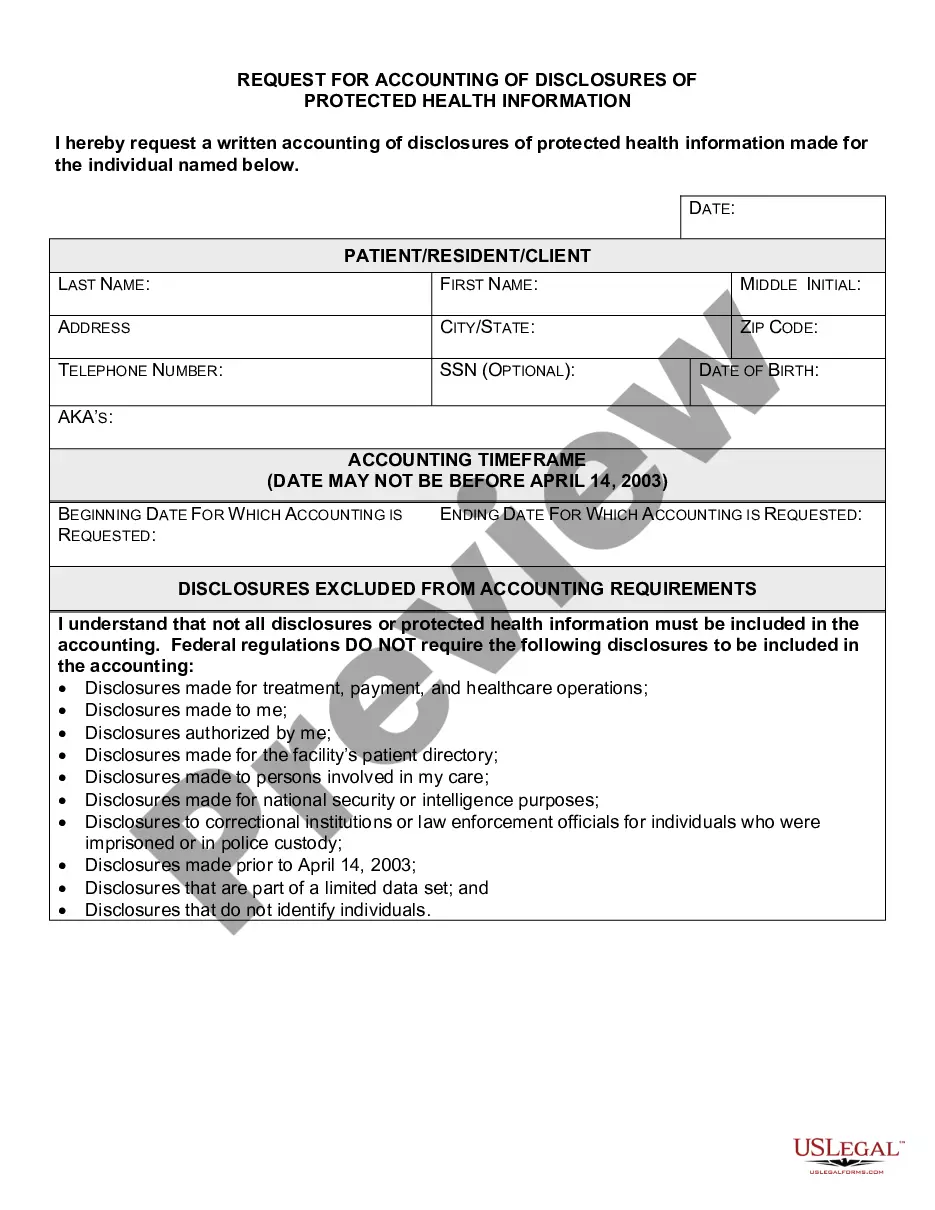
"Minimum Necessary" means, when protected health information is used, disclosed, or requested, reasonable efforts must be taken to determine how much information will be sufficient to serve the intended purpose.
A signed HIPAA release form must be obtained from a patient before their protected health information can be shared with other individuals or organizations, except in the case of routine disclosures for treatment, payment or healthcare operations permitted by the HIPAA Privacy Rule.
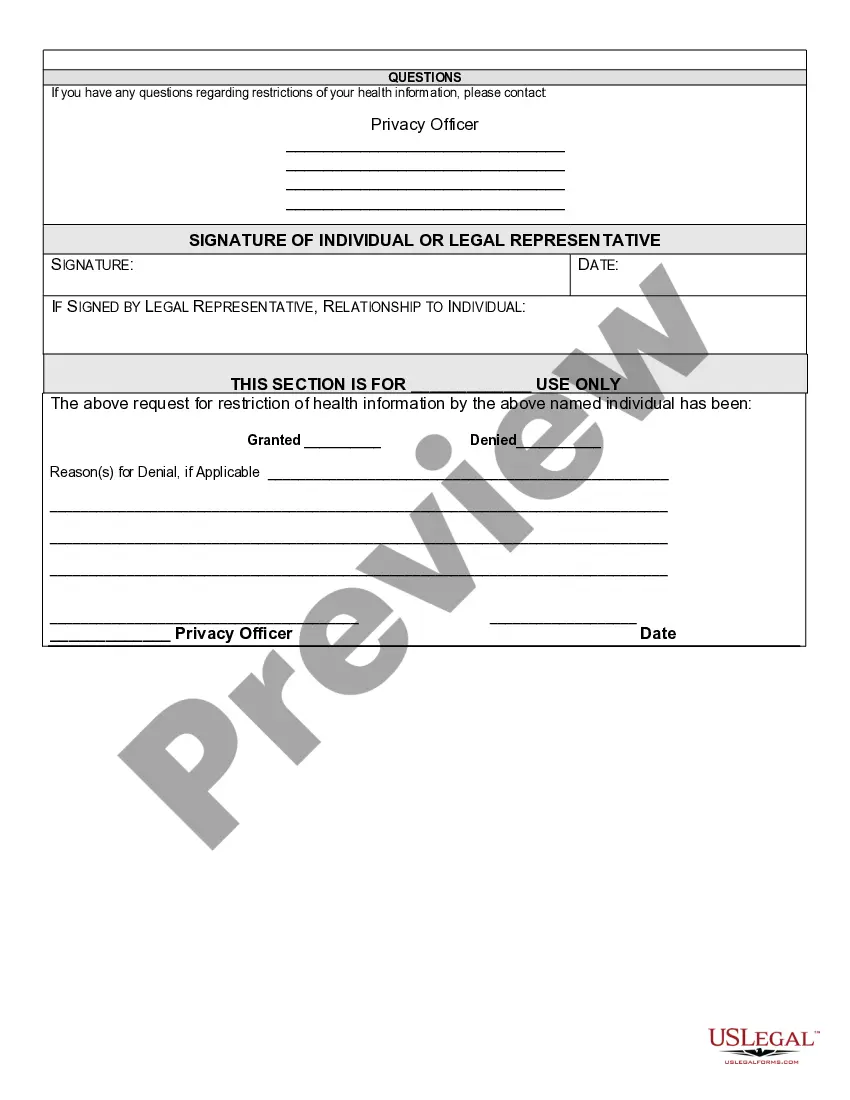
A completed and approved request for restriction on a disclosure to health plans form must be filed in the episode of care covered by the payment (whether electronic or paper) with easy access to that document. The form must also clearly identify the episode of care covered by the payment.
When a patient requests that information not be disclosed to a specified individual or entity, the Request Restrictions on Use and Disclosure of PHI form must be completed and signed. An authorized healthcare professional will review the request and determine if it can be accommodated.
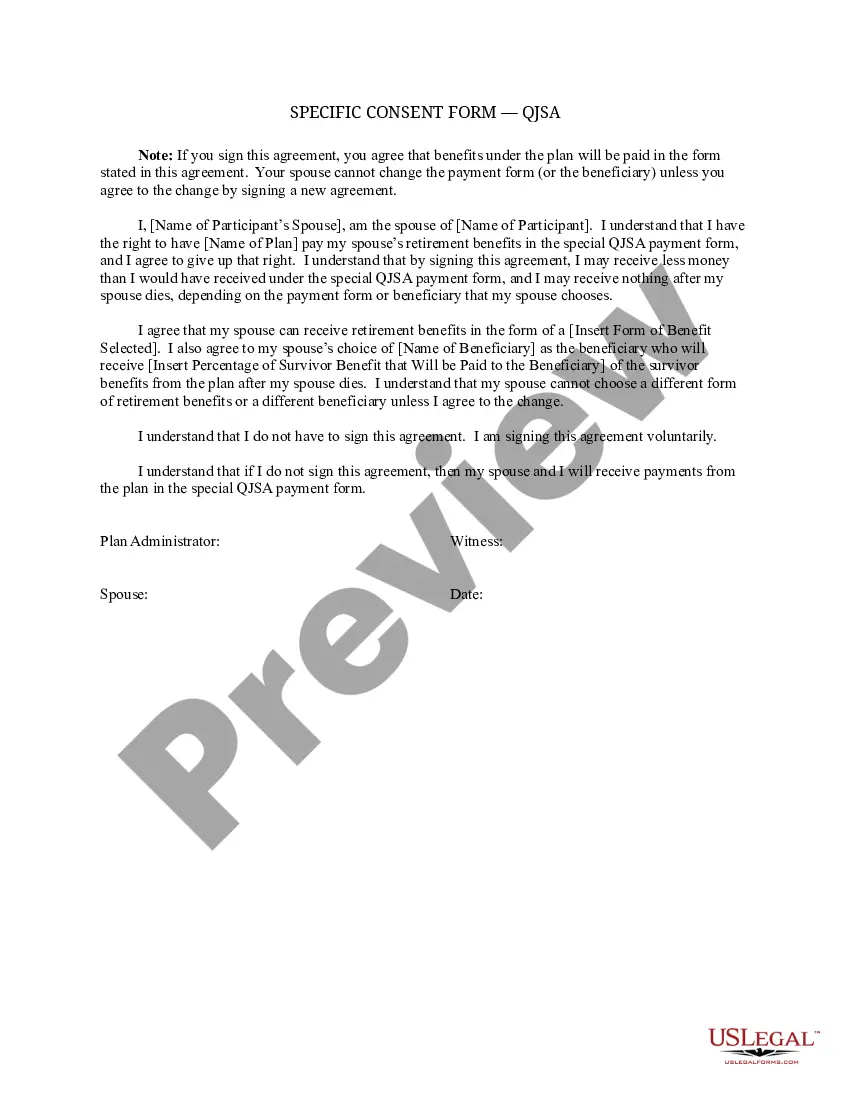
What is a patient required to do in order for a request to restrict the use or disclosure of their PHI to their health plan to be granted? The Privacy Rule allows for a patient to request that no information be shared with others even to the point of not acknowledging the patient's presence in the covered entity.
The HIPAA Privacy Rule provides individuals with the right to inspect their PHI held in a designated record set, either in addition to obtaining copies or in lieu thereof, and requires covered entities to arrange with the individual for a convenient time and place to inspect the PHI.
A covered entity such as a doctor must agree to an individual's request to restrict disclosure of her PHI to a health plan if: the disclosure is for the purpose of carrying out payment or health care operations and is not required by law; and.