Oklahoma Notice of Qualifying Event from Employer to Plan Administrator
Description
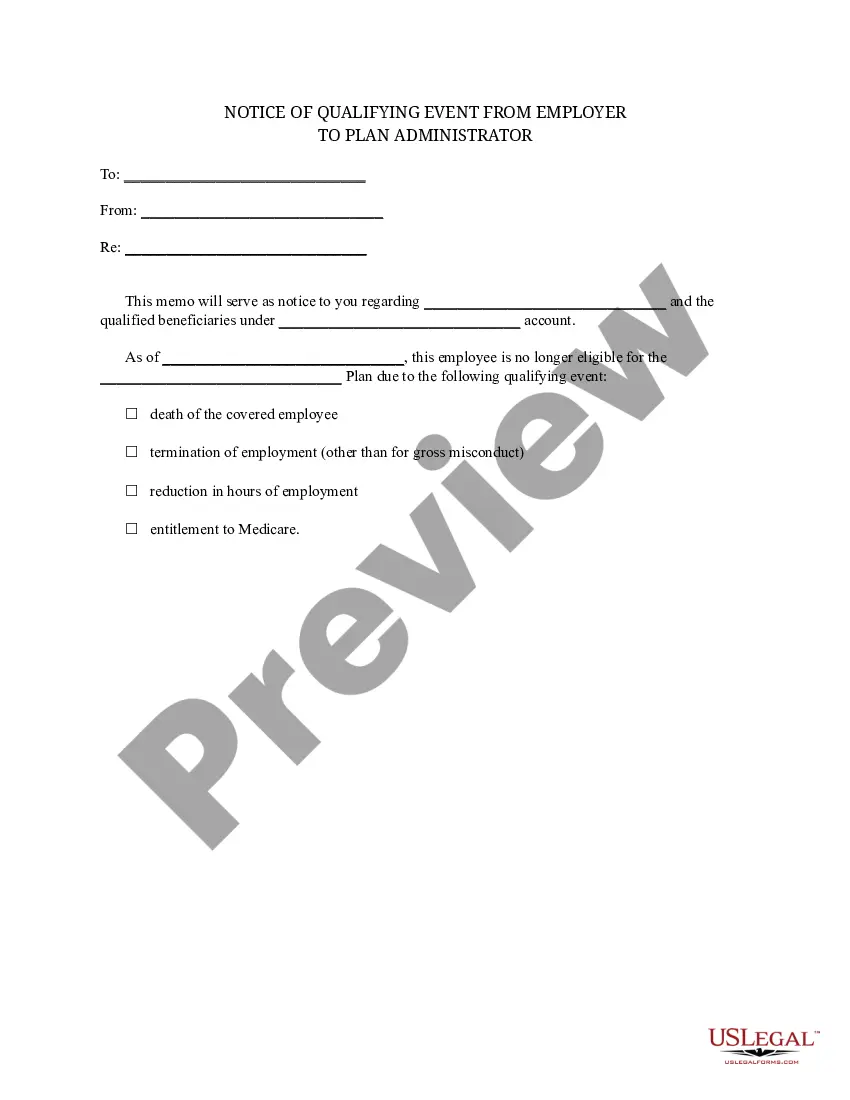
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
US Legal Forms - one of the largest collections of legal documents in the United States - offers a broad selection of legal document templates that you can download or generate.
By using the website, you can discover numerous forms for business and personal purposes, organized by categories, states, or keywords.
You can retrieve the latest versions of forms like the Oklahoma Notice of Qualifying Event from Employer to Plan Administrator in moments.
If the document does not meet your needs, use the Search area at the top of the screen to find one that fits.
If you are satisfied with the form, confirm your choice by clicking the Get now button. Then, select your preferred pricing plan and provide your information to register for an account.
- If you already have a subscription, Log In and download the Oklahoma Notice of Qualifying Event from Employer to Plan Administrator in the US Legal Forms collection.
- The Download button will appear on every document you view.
- You can access all previously downloaded documents in the My documents section of your account.
- If you wish to use US Legal Forms for the first time, here are simple steps to get started.
- Ensure you have chosen the right document for your city/county.
- Review the Preview button to examine the document’s content.
Form popularity
FAQ
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section.Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.More items...
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
How to Administer Cal-COBRANotifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.