Nevada Individual Notice of Preexisting Condition Exclusion
Description
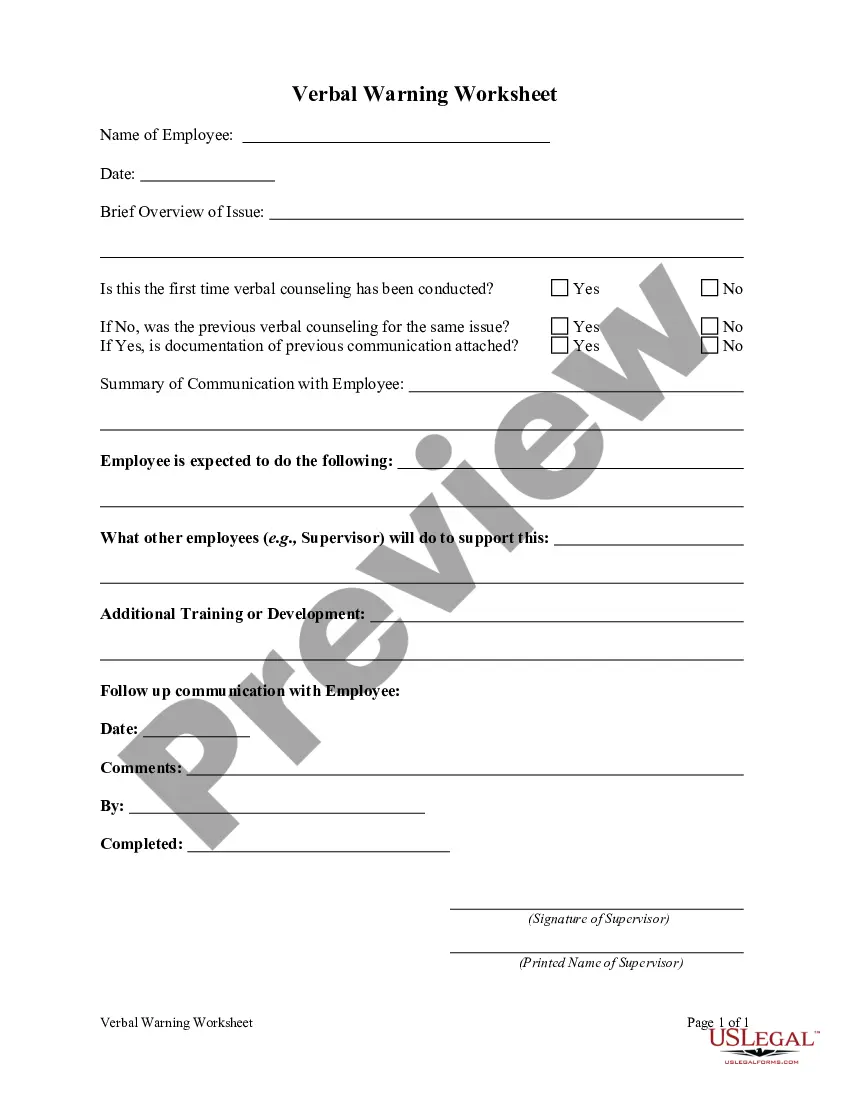
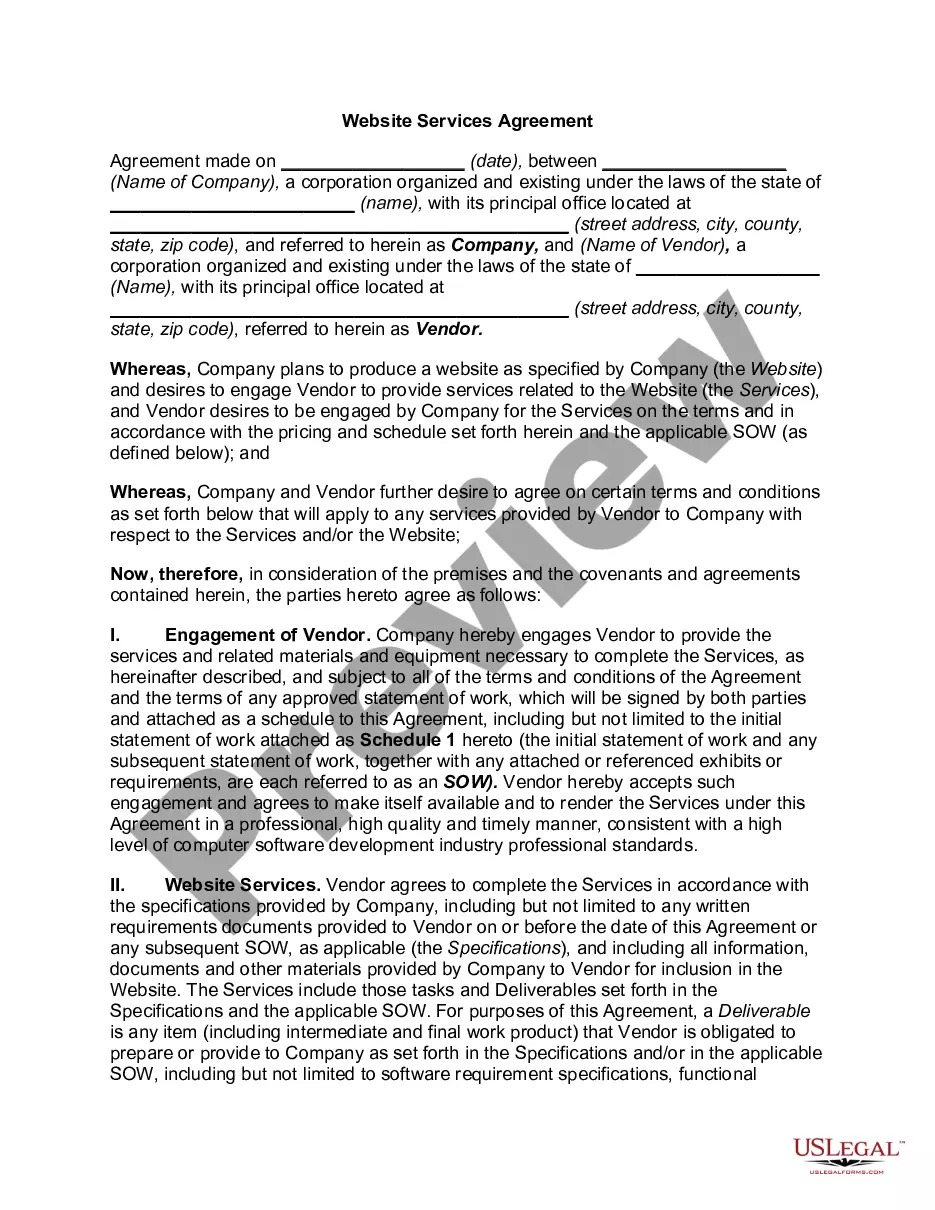
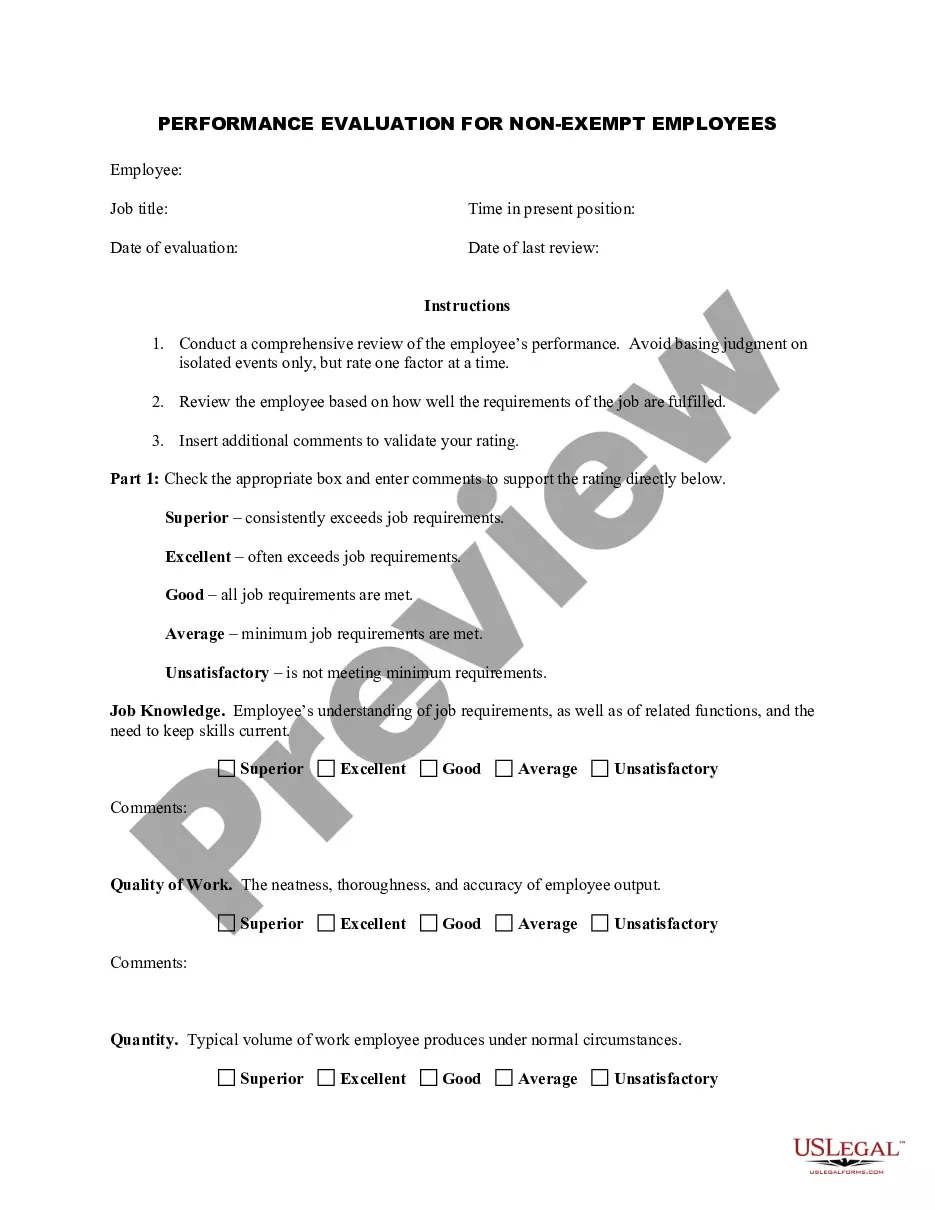
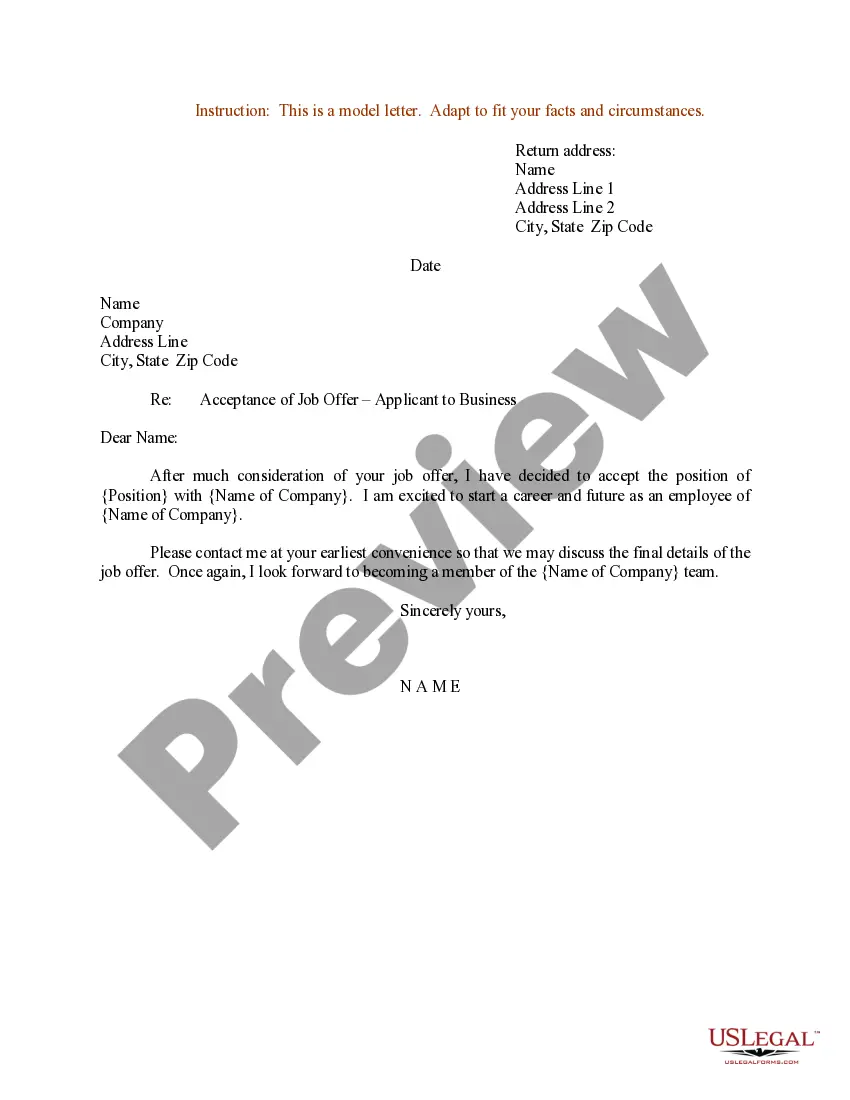
How to fill out Individual Notice Of Preexisting Condition Exclusion?
It is feasible to allocate time online trying to discover the sanctioned document template that aligns with the federal and state criteria you require.
US Legal Forms offers thousands of legal forms that are evaluated by specialists.
You can easily obtain or print the Nevada Individual Notice of Preexisting Condition Exclusion from the service.
- If you already have a US Legal Forms account, you can Log In and then click the Download button.
- Subsequently, you can complete, modify, print, or sign the Nevada Individual Notice of Preexisting Condition Exclusion.
- Every legal document template you obtain is yours forever.
- To obtain an additional copy of a purchased form, go to the My documents tab and click the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the straightforward instructions below.
Form popularity
FAQ
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
About Nevada's Mini-COBRA Insurance Law When the federal COBRA law doesn't apply, Nevada state statutes gives workers of businesses with 19 or fewer employees the right to continue their employer-sponsored health insurance.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
In Nevada, there are two types of COBRA healthcare continuation coverage: federal COBRA and Nevada COBRA insurance.
Expenses related to the treatment of the listed Conditions, surgeries/treatments as per Table A and Table B below, shall be excluded until the expiry of 24 months and 48 months respectively of continuous coverage after the date of inception of the first policy with us.
For disabled QBs who receive an 11-month COBRA extension (29 months in total), you can charge up to 150% of the group rate. Many states have regulations that are similar to federal COBRA. These state regulations are known as mini-COBRA.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
Here's a look at a few states and their variations: New Jersey: employers with two to 50 employees must comply with the state's Mini-COBRA law. Arkansas, Illinois, Texas, and Nevada: Mini-COBRA laws that apply to all employers, regardless of the number of employees.
COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.