Mississippi General Notice of Preexisting Condition Exclusion
Description
How to fill out General Notice Of Preexisting Condition Exclusion?
If you want to completely acquire, download, or print valid document templates, utilize US Legal Forms, the largest collection of valid forms available online.
Take advantage of the site's user-friendly and convenient search to find the documents you require.
A range of templates for business and personal purposes are organized by categories and states, or keywords.
Step 4. Once you have located the form you need, click on the Purchase now button. Choose the pricing plan you prefer and enter your details to sign up for an account.
Step 5. Process the payment. You can use your credit card or PayPal account to complete the transaction.
- Utilize US Legal Forms to obtain the Mississippi General Notice of Preexisting Condition Exclusion with just a few clicks.
- If you are currently a US Legal Forms customer, Log Into your account and click the Acquire button to get the Mississippi General Notice of Preexisting Condition Exclusion.
- You can also access forms you previously downloaded in the My documents section of your account.
- If this is your first time using US Legal Forms, follow the steps below.
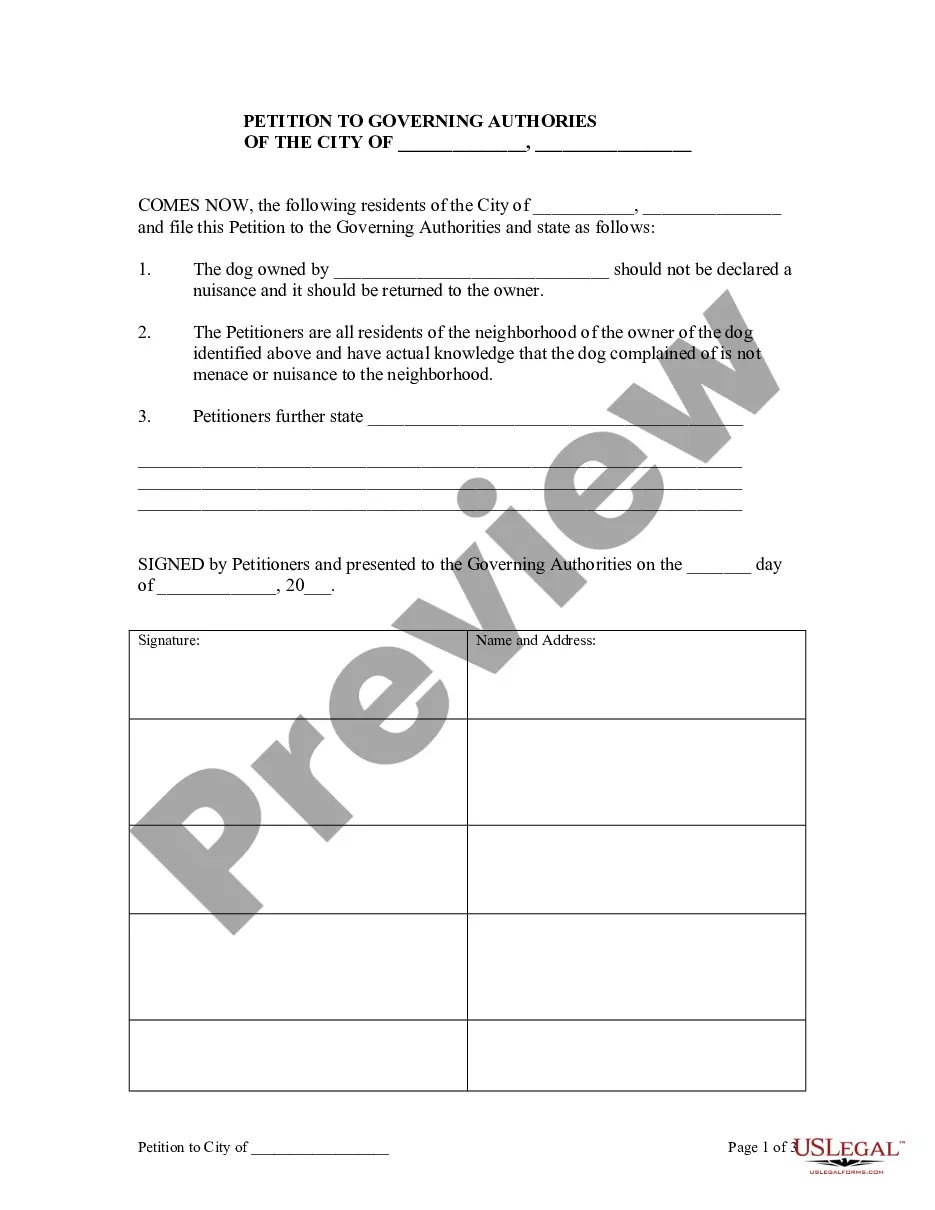
- Step 1. Ensure you have selected the form for the correct city/state.
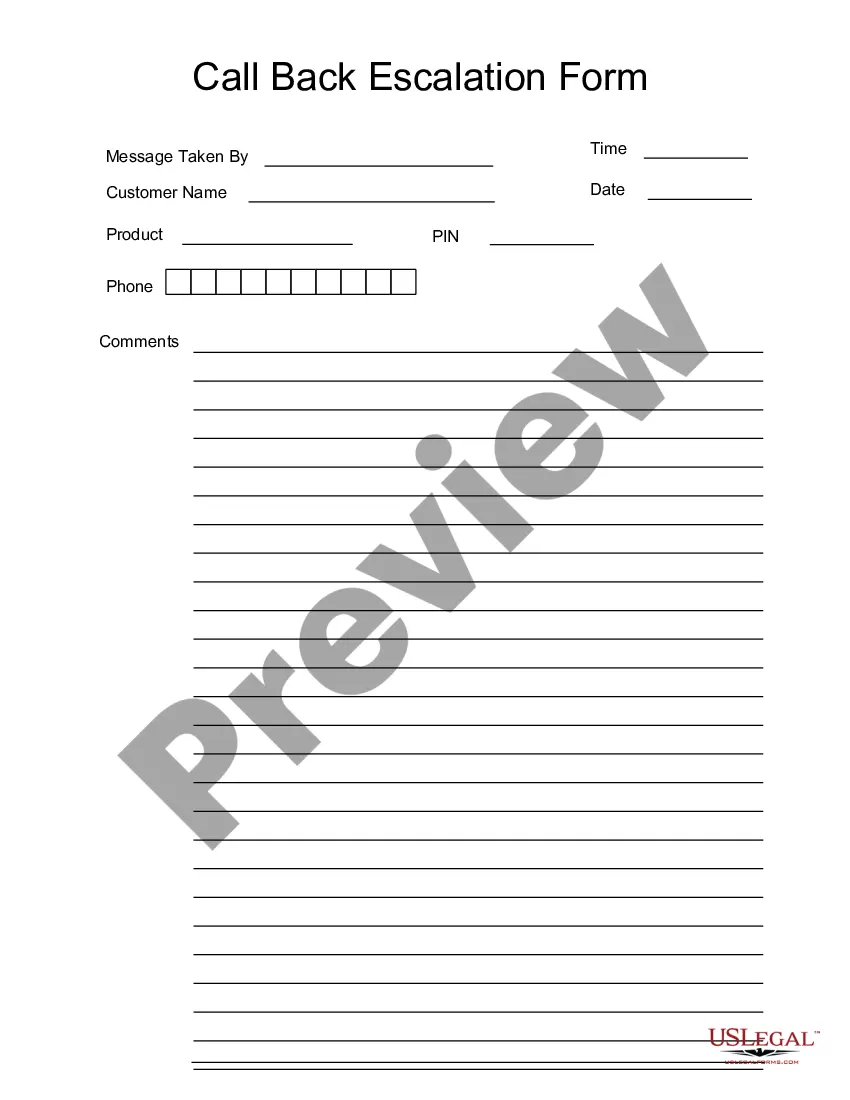
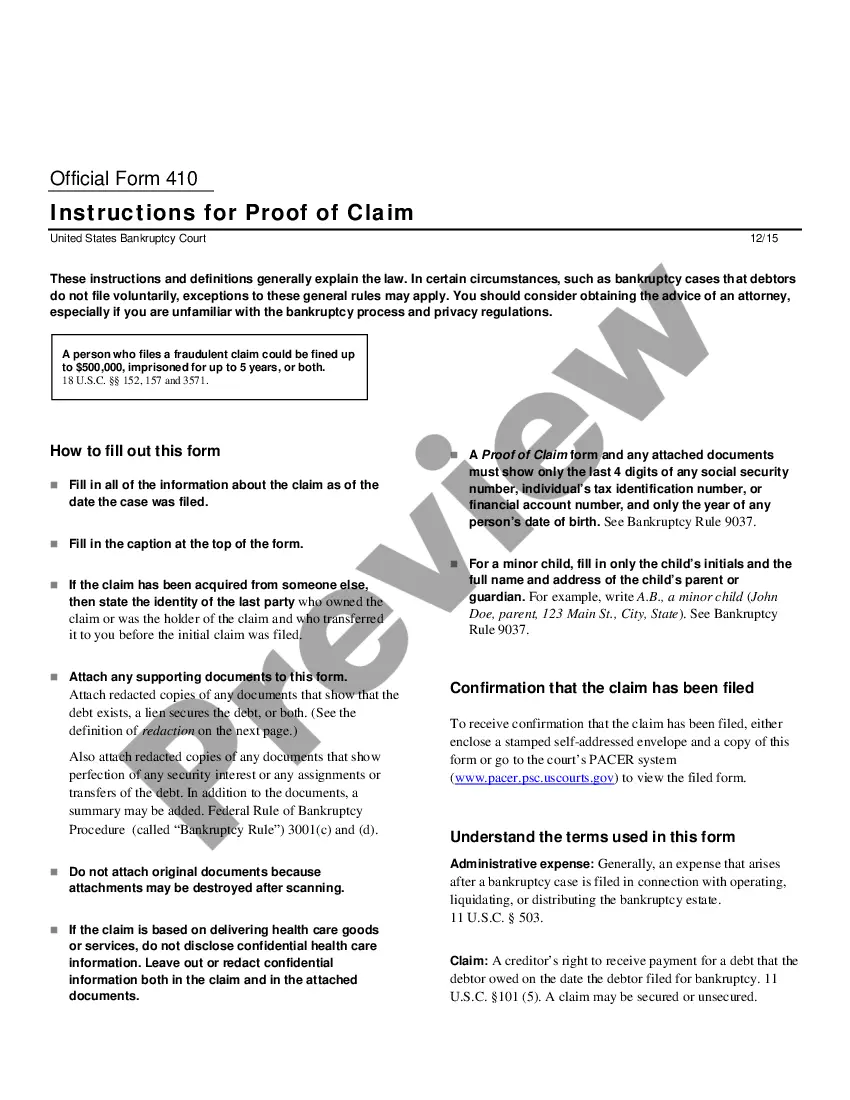
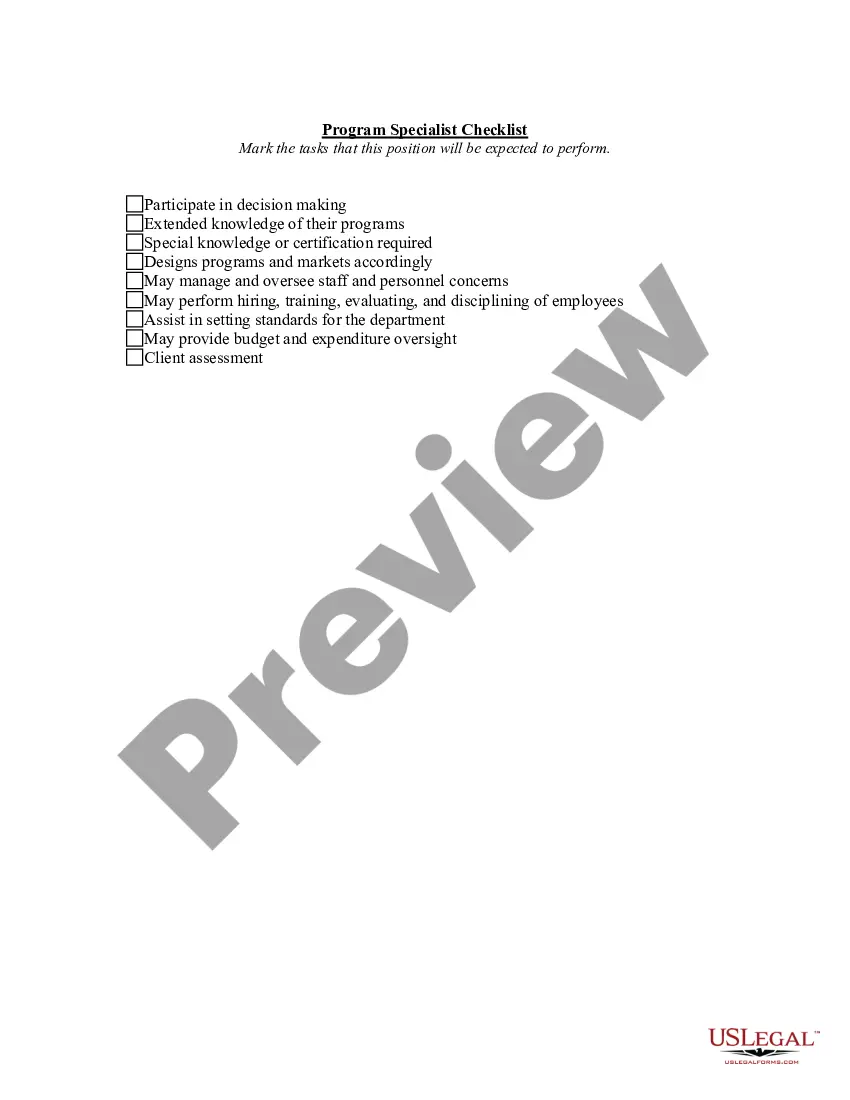
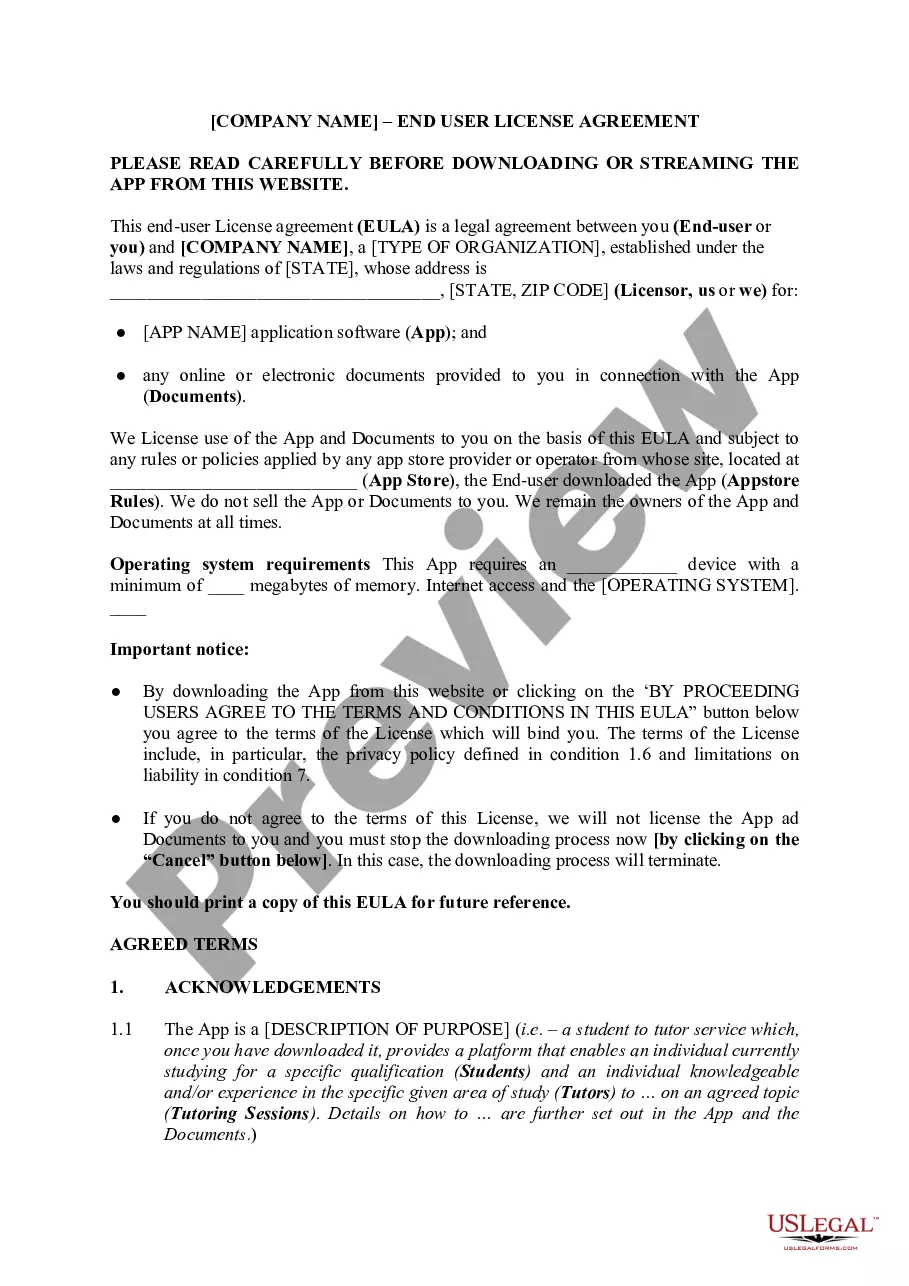
- Step 2. Use the Review option to browse the form’s content. Be sure to read the information.
- Step 3. If you are not satisfied with the form, use the Search area at the top of the screen to find alternative versions of the legal form template.
Form popularity
FAQ
Even if you were unaware of a condition, it can still be classified as pre-existing if it was present before the insurance coverage began. Insurers rely on veterinary records to make these determinations, so be sure to keep thorough documentation. This can be crucial in understanding the implications of the Mississippi General Notice of Preexisting Condition Exclusion.
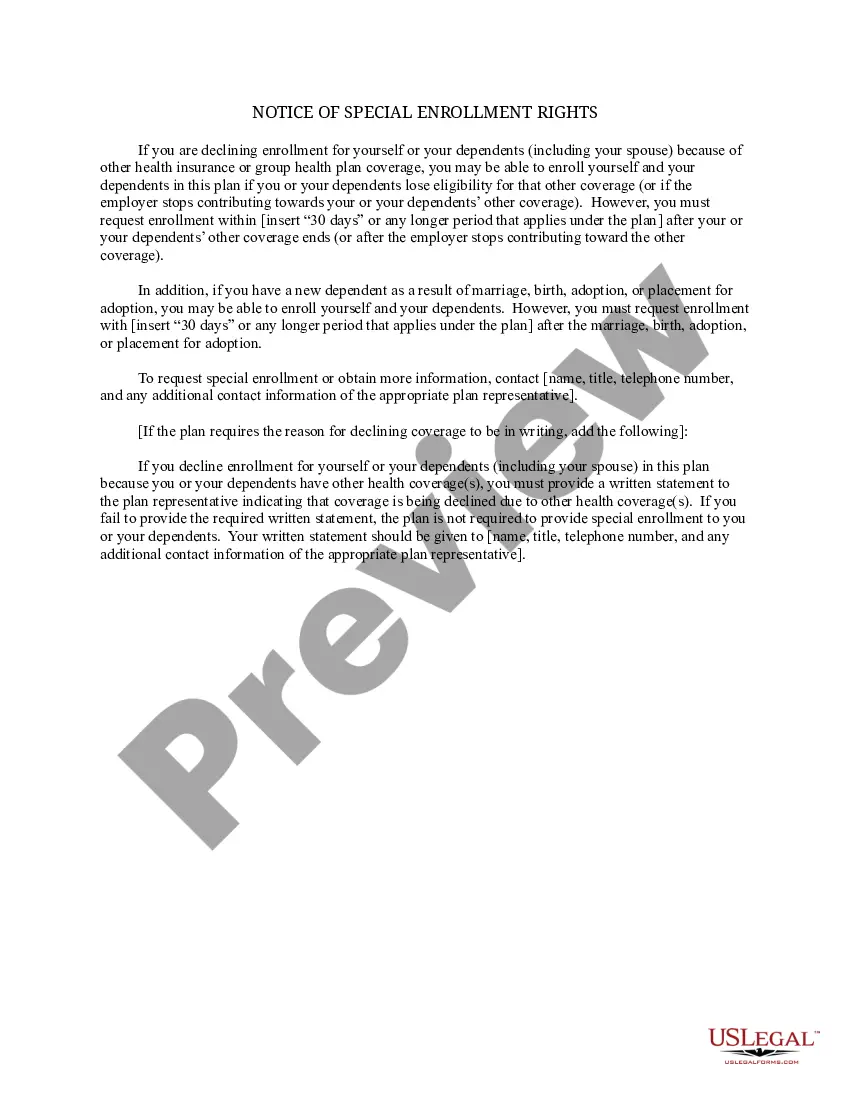
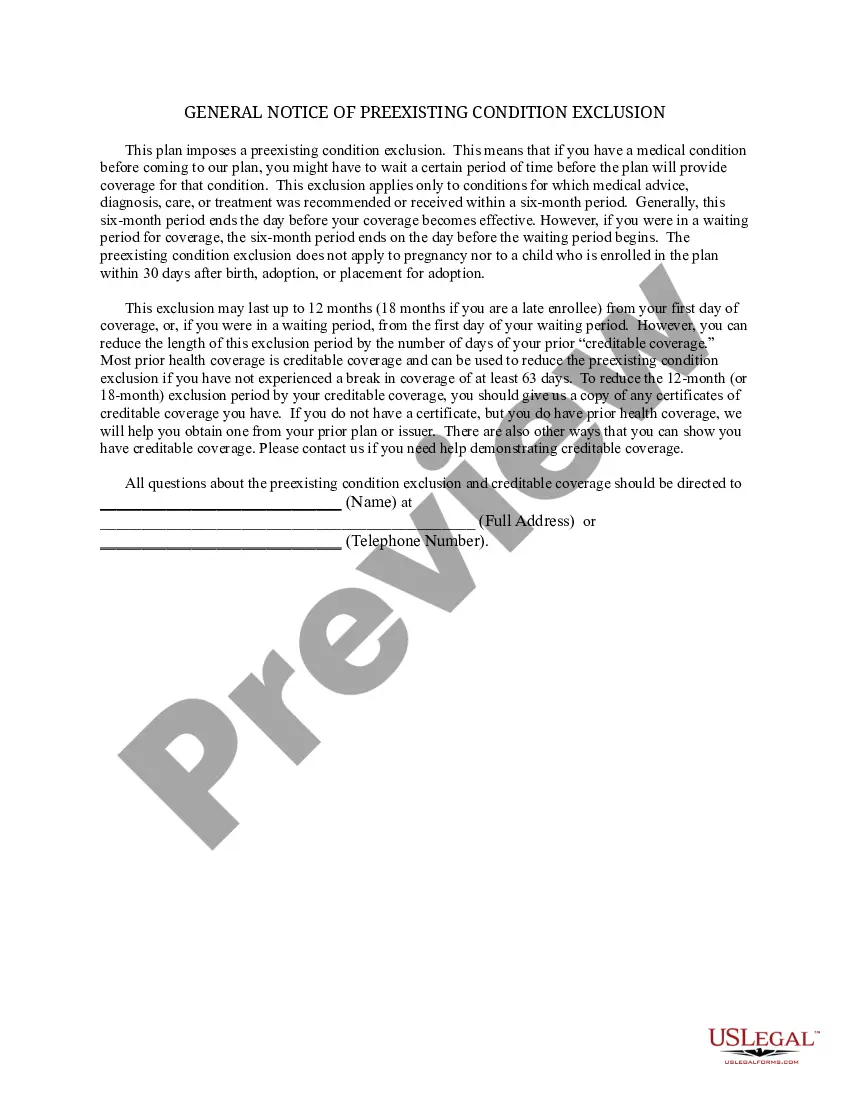
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Employer-based plans and individual health plans cannot deny coverage to people with pre-existing conditions. People under individual health plans that existed before September 23, 2010 known as grandfathered plans, are allowed to use pre-existing condition exclusions.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.