Mississippi Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
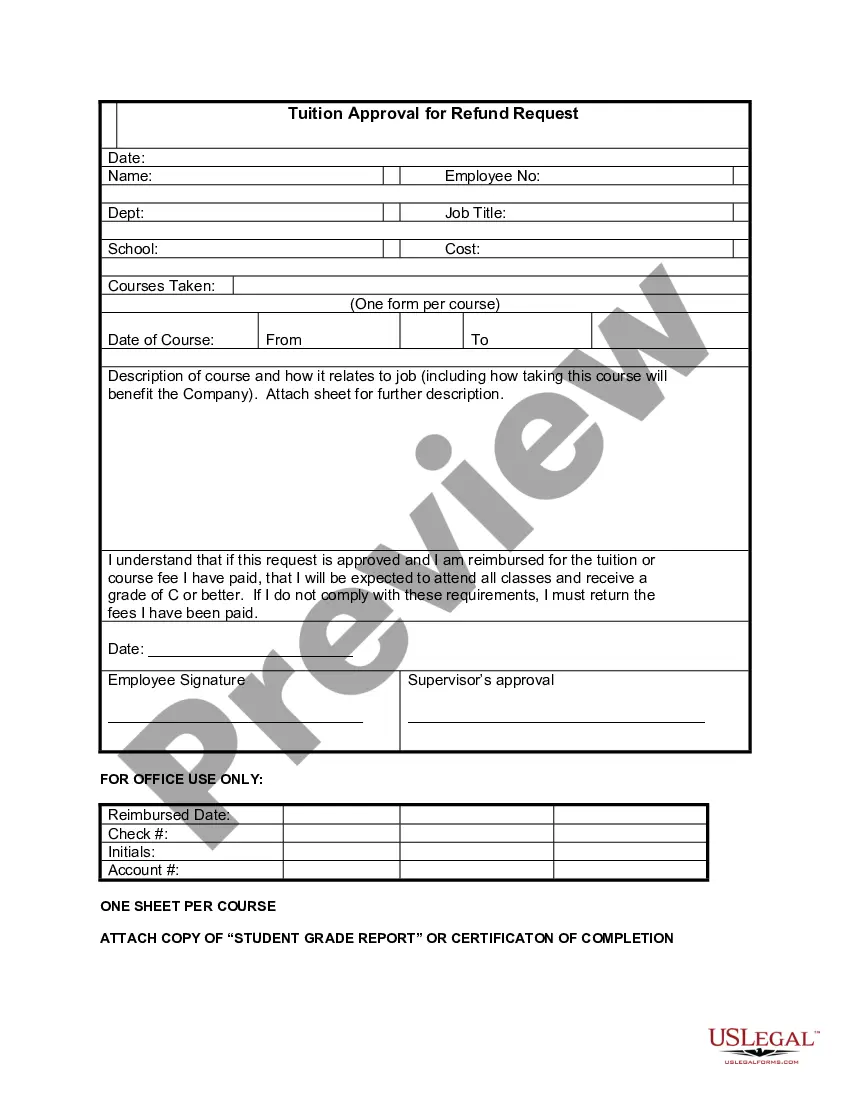
How to fill out Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
It is feasible to spend hours online seeking the authentic document format that complies with the federal and state requirements you require.
US Legal Forms offers thousands of authentic templates that are vetted by experts.
You can easily obtain or create the Mississippi Employer - Plan Administrator Notice to Employee of Unavailability of Continuation from my services.
In order to locate another version of the document, utilize the Search field to find the template that meets your specifications and needs.
- If you already have a US Legal Forms account, you can Log In and click on the Download button.
- After that, you can complete, edit, print, or sign the Mississippi Employer - Plan Administrator Notice to Employee of Unavailability of Continuation.
- Every authentic document template you obtain belongs to you permanently.
- To get another copy of any acquired form, visit the My documents tab and click on the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have chosen the correct document format for the region/city of your choice.
- Check the form description to confirm you have selected the correct type.
Form popularity
FAQ
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
What is Cal-COBRA? Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.
COBRA is an acronym for the Consolidated Omnibus Budget Reconciliation Act, which provides eligible employees and their dependents the option of continued health insurance coverage when an employee loses their job or experiences a reduction of work hours.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
The term continuation coverage refers to the extended coverage provided under the group benefit plan in which an eligible employee or eligible dependent is currently enrolled.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.