Mississippi COBRA Continuation Coverage Election Notice
Description
How to fill out COBRA Continuation Coverage Election Notice?
If you need to full, down load, or produce authorized document templates, use US Legal Forms, the largest collection of authorized kinds, that can be found online. Utilize the site`s basic and convenient look for to get the papers you need. Different templates for organization and individual functions are sorted by groups and claims, or keywords and phrases. Use US Legal Forms to get the Mississippi COBRA Continuation Coverage Election Notice in a handful of mouse clicks.
Should you be previously a US Legal Forms consumer, log in to the profile and click the Download switch to find the Mississippi COBRA Continuation Coverage Election Notice. You can even entry kinds you in the past acquired inside the My Forms tab of your respective profile.
If you work with US Legal Forms initially, follow the instructions listed below:
- Step 1. Be sure you have selected the form for the appropriate town/region.
- Step 2. Use the Preview option to check out the form`s content material. Don`t forget to read through the outline.
- Step 3. Should you be not satisfied with all the type, use the Look for industry near the top of the screen to discover other variations from the authorized type web template.
- Step 4. After you have located the form you need, go through the Purchase now switch. Choose the rates plan you choose and include your references to sign up on an profile.
- Step 5. Procedure the financial transaction. You should use your Мisa or Ьastercard or PayPal profile to finish the financial transaction.
- Step 6. Pick the structure from the authorized type and down load it on the product.
- Step 7. Total, change and produce or sign the Mississippi COBRA Continuation Coverage Election Notice.
Each authorized document web template you acquire is your own property permanently. You might have acces to every type you acquired with your acccount. Click on the My Forms area and select a type to produce or down load again.
Be competitive and down load, and produce the Mississippi COBRA Continuation Coverage Election Notice with US Legal Forms. There are millions of expert and state-specific kinds you can use for your personal organization or individual needs.
Form popularity
FAQ
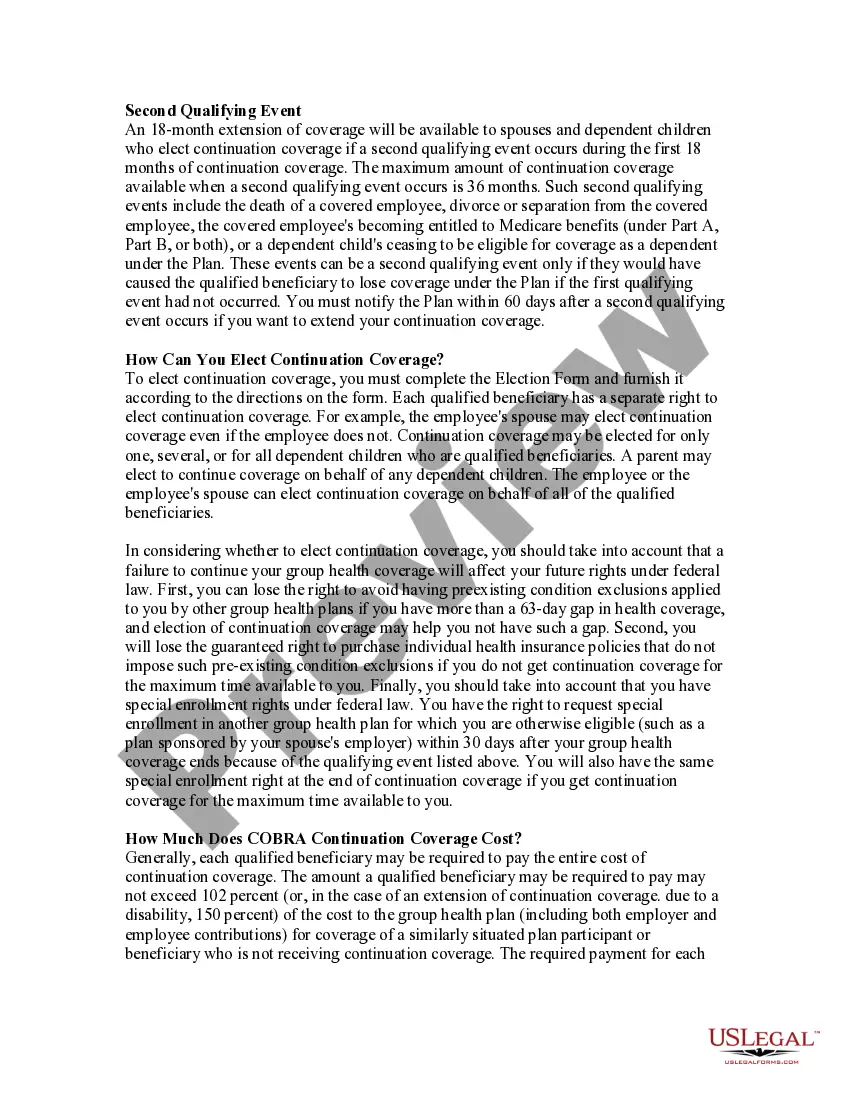
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
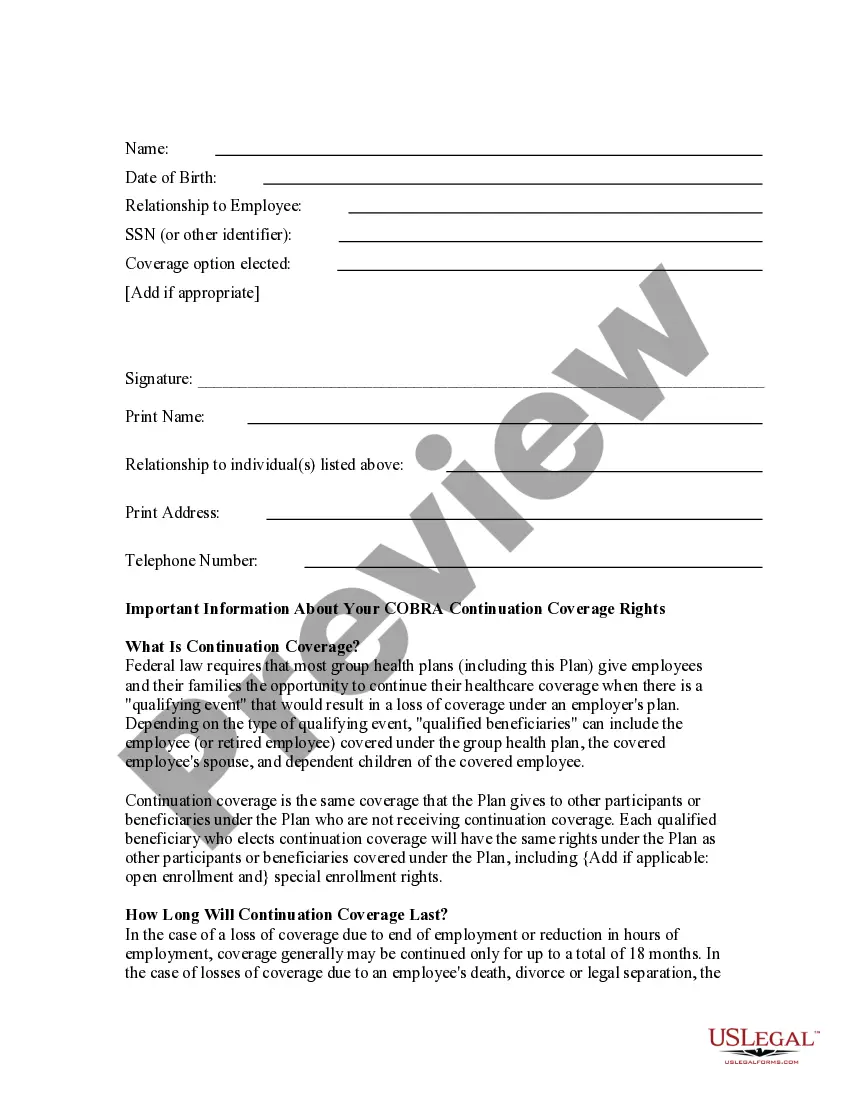
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
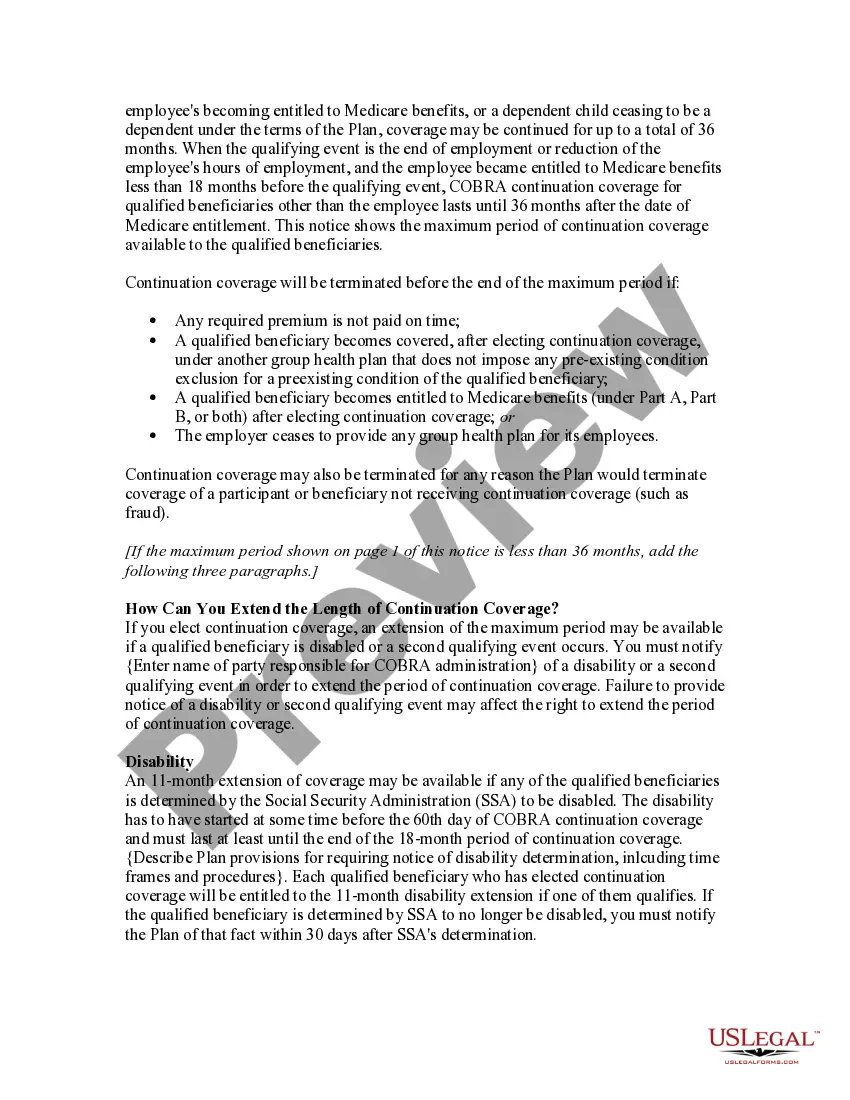
Will I be able to make changes to my plan elections in the future. Yes. Once COBRA continuation coverage is elected and the 60 day election period has passed, you can drop a plan at any time. But, to change between plans or add new plans, you may need to wait until open enrollment.
Under COBRA, a group health plan is any arrangement that an employer establishes or maintains to provide employees or their families with medical care, whether it is provided through insurance, by a health maintenance organization, out of the employer's assets, or through any other means.