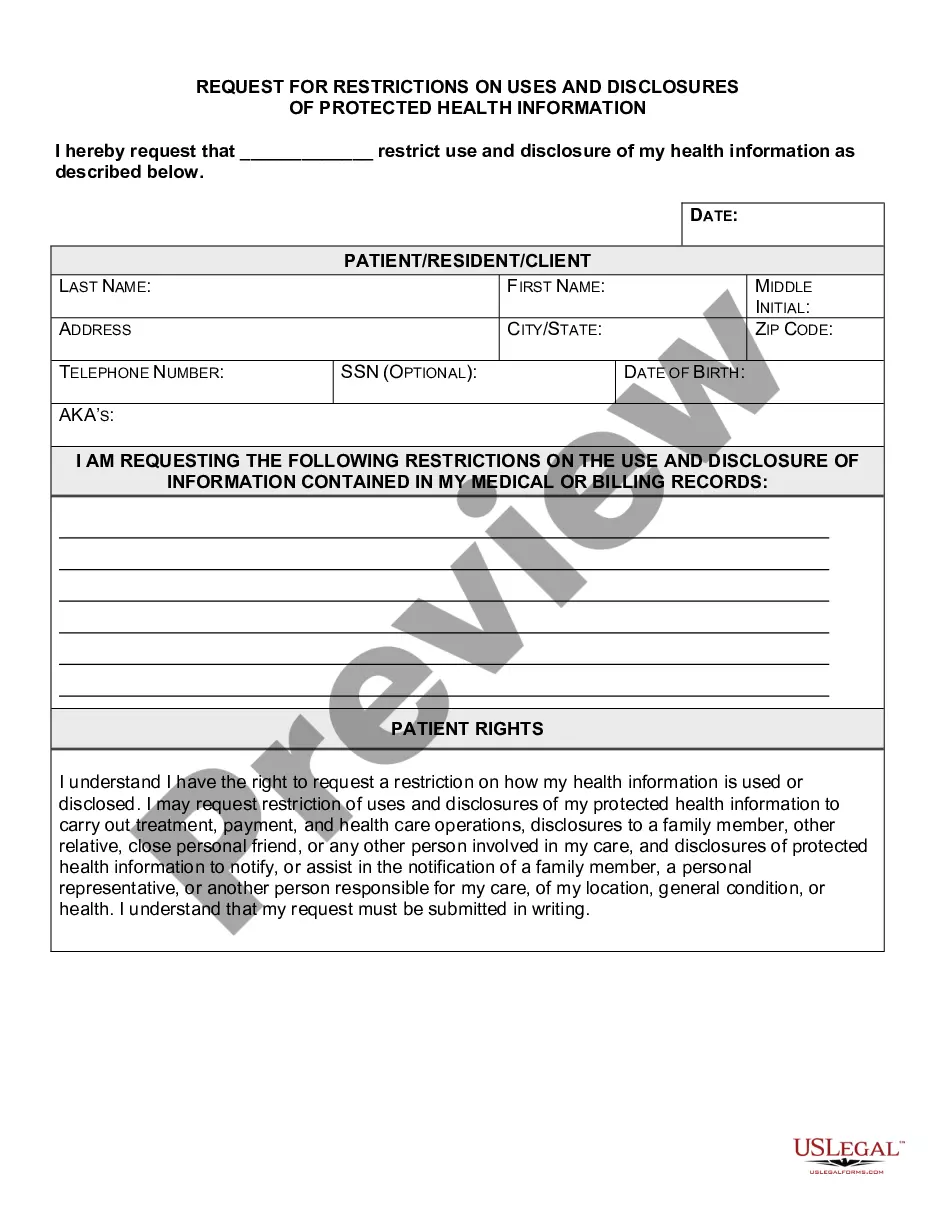
Kentucky Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
Are you presently in a role where you require documents for potential company or particular purposes almost every workday.
There are numerous reliable document templates available online, but finding ones you can trust can be challenging.
US Legal Forms offers a vast selection of form templates, including the Kentucky Request for Limitations on Uses and Disclosures of Protected Health Information, which are designed to comply with federal and state regulations.
If you find the appropriate form, simply click Download now.
Select the pricing plan you prefer, fill out the required details to create your account, and pay for your order using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Kentucky Request for Limitations on Uses and Disclosures of Protected Health Information template.
- If you do not have an account and wish to start using US Legal Forms, follow these instructions.
- Obtain the form you need and ensure it is for the correct city/region.
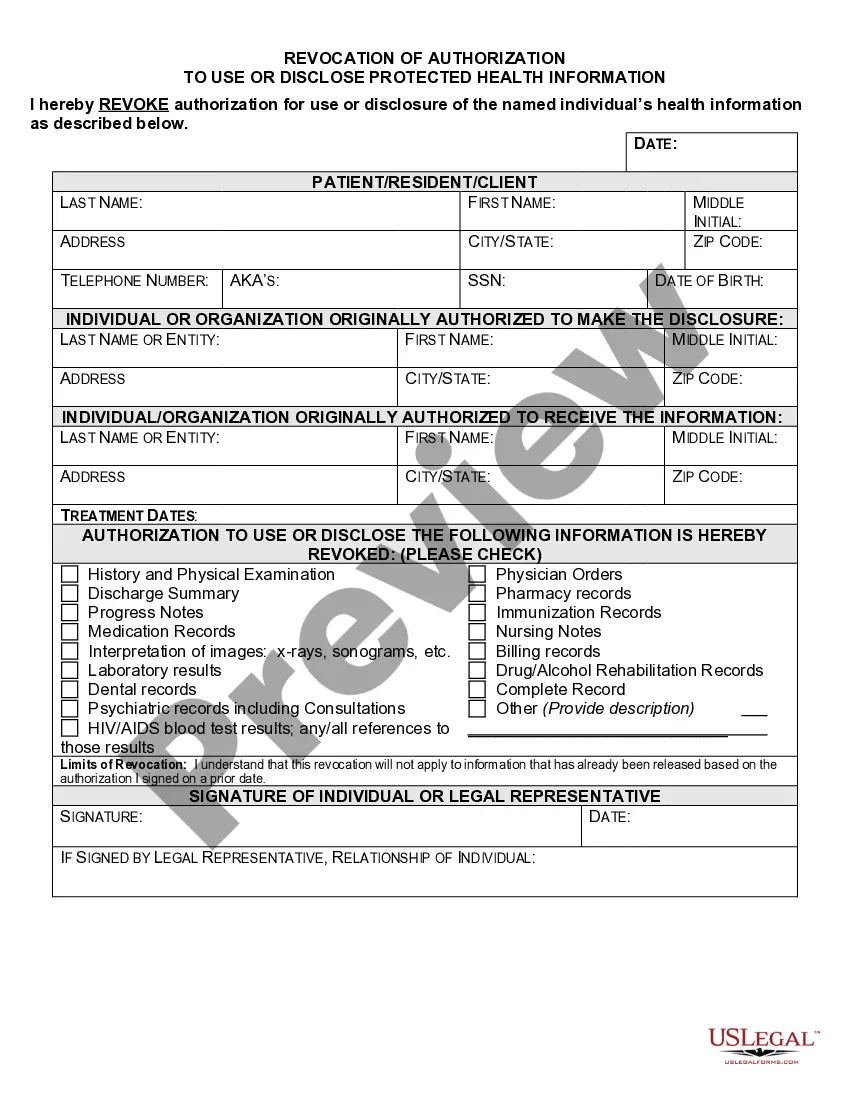
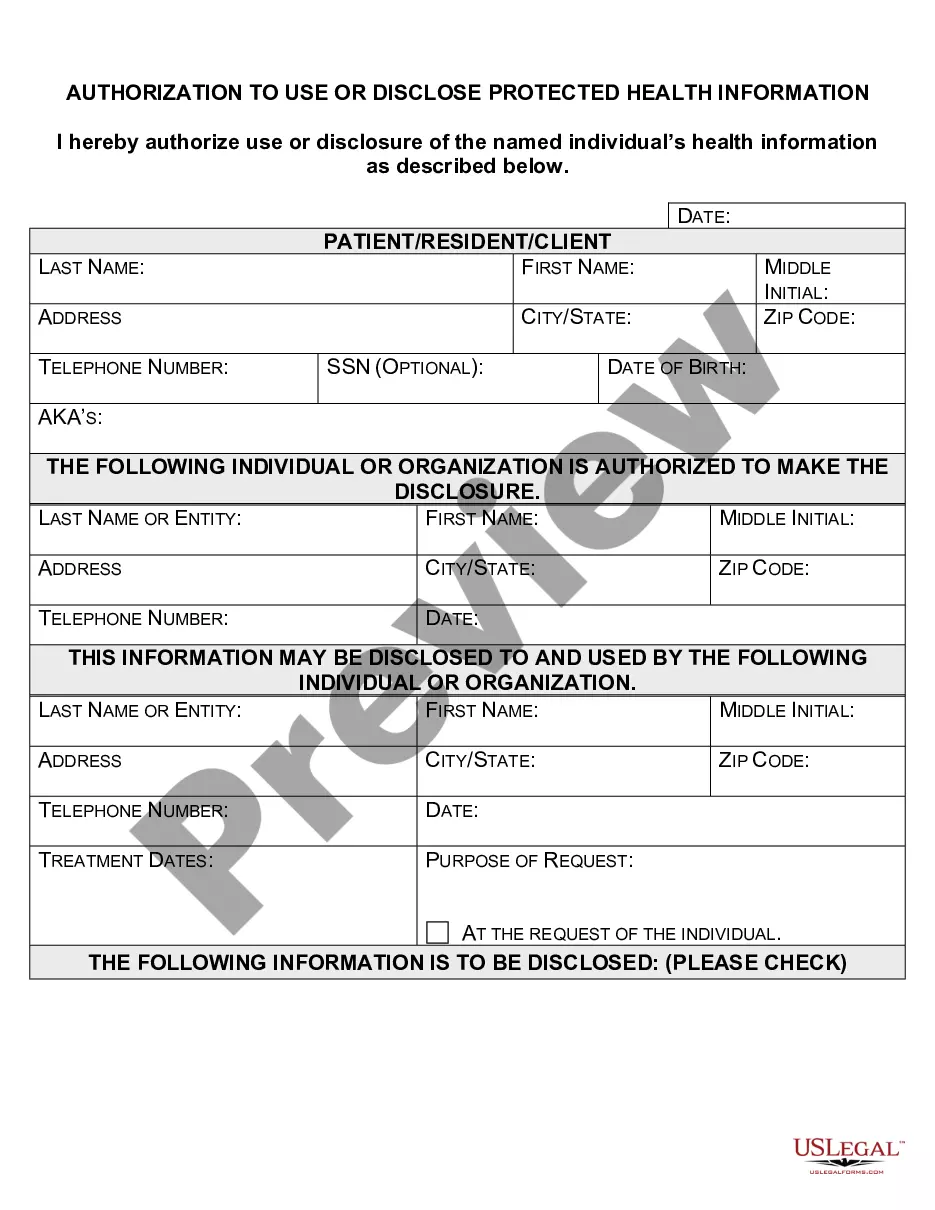
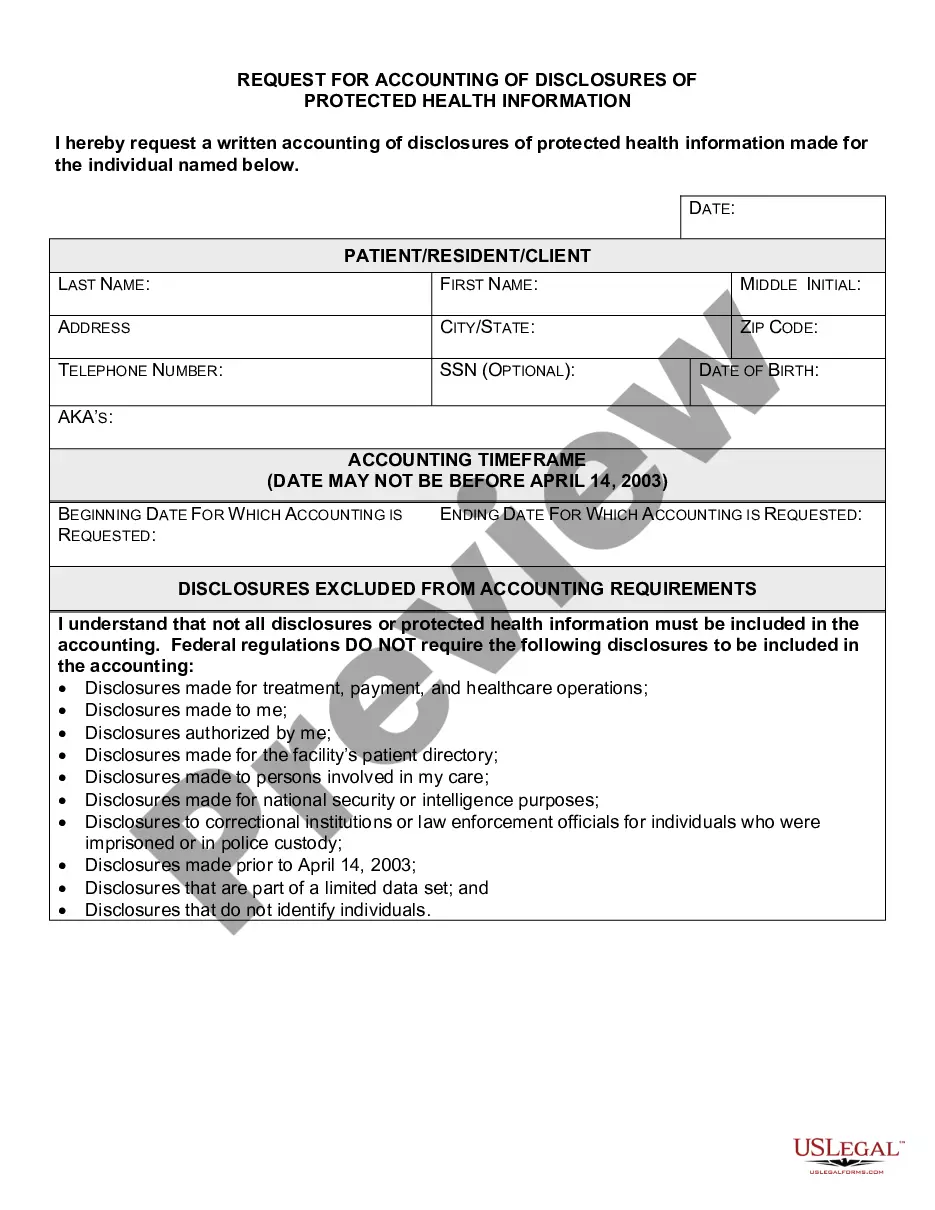
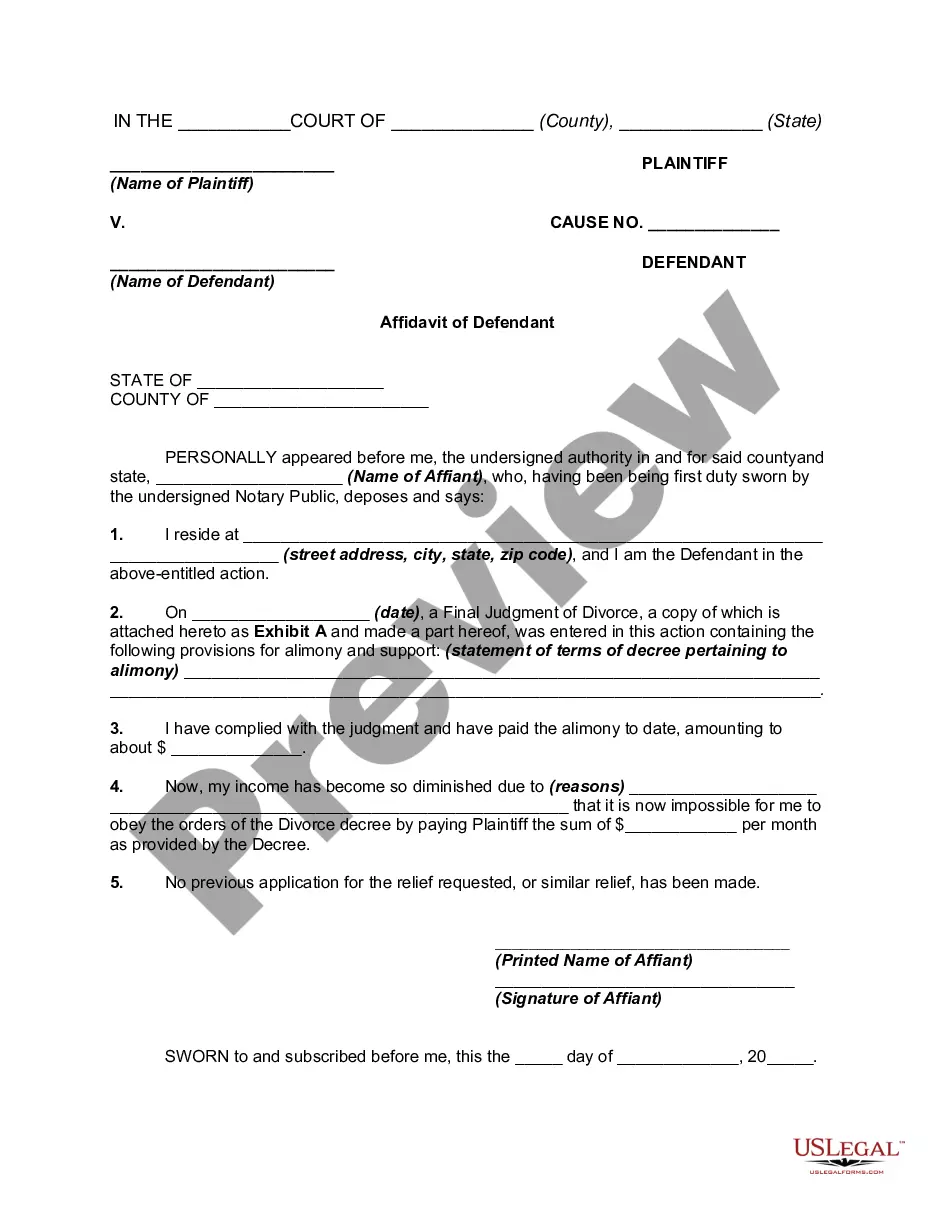
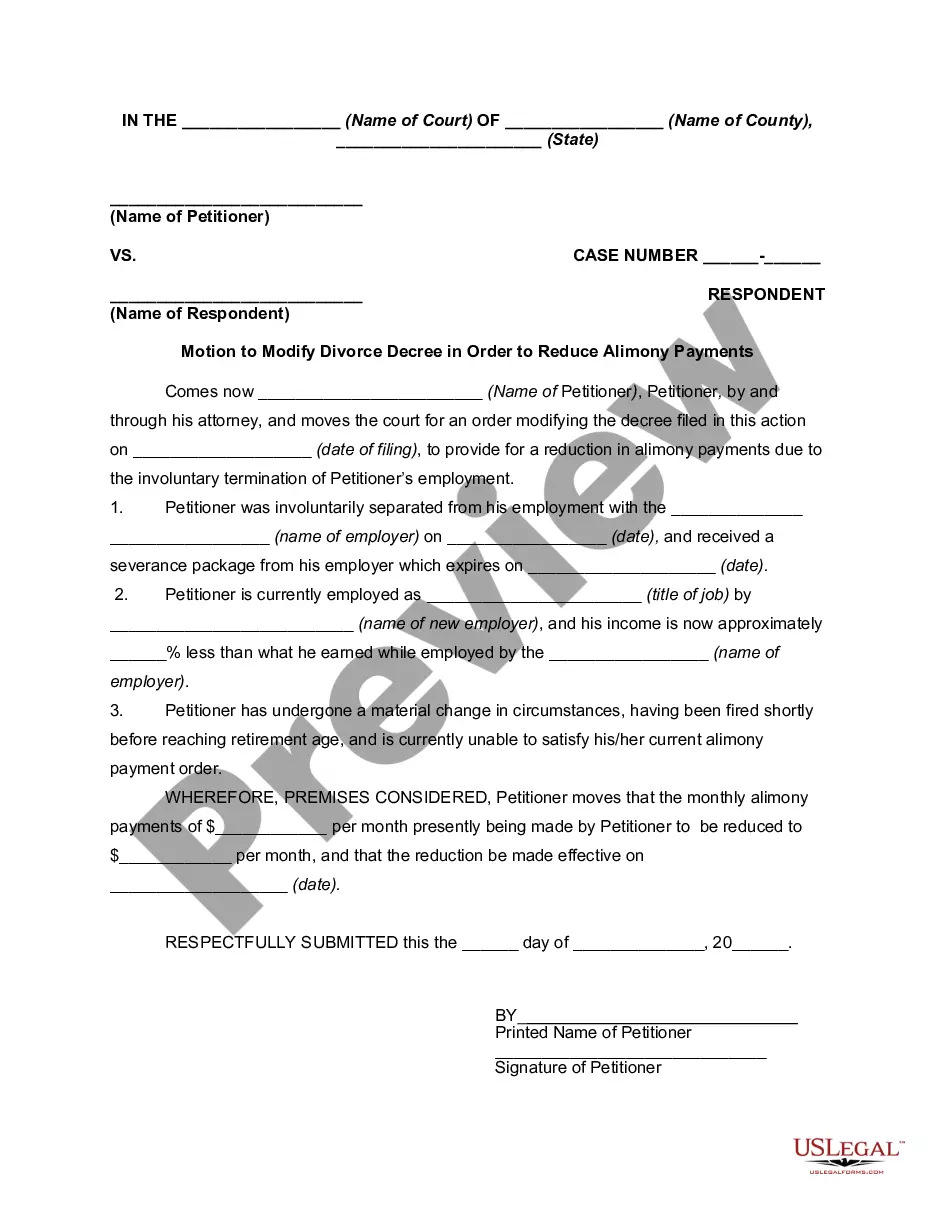
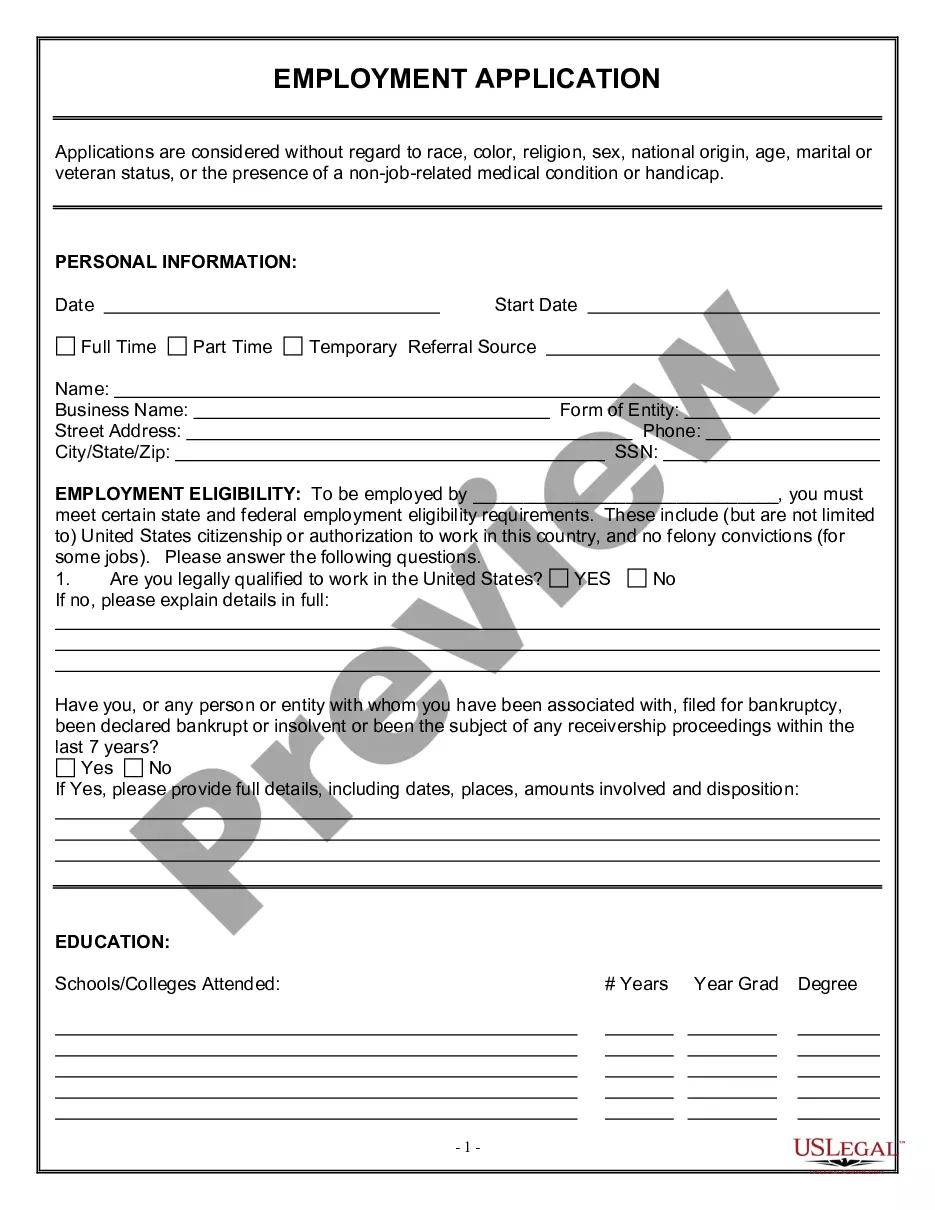
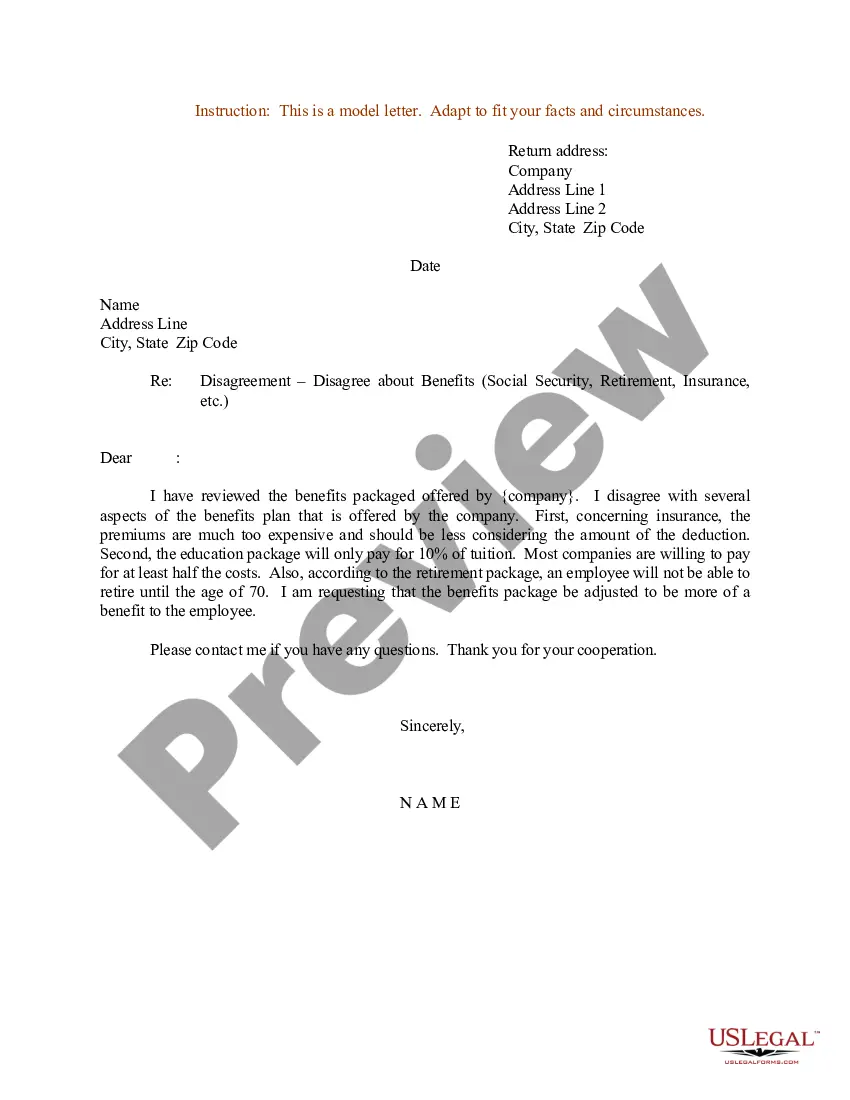
- Use the Preview button to review the document.
- Check the description to ensure you have chosen the right form.
- If the form does not match your needs, use the Search field to find the template that fits your criteria.
Form popularity
FAQ
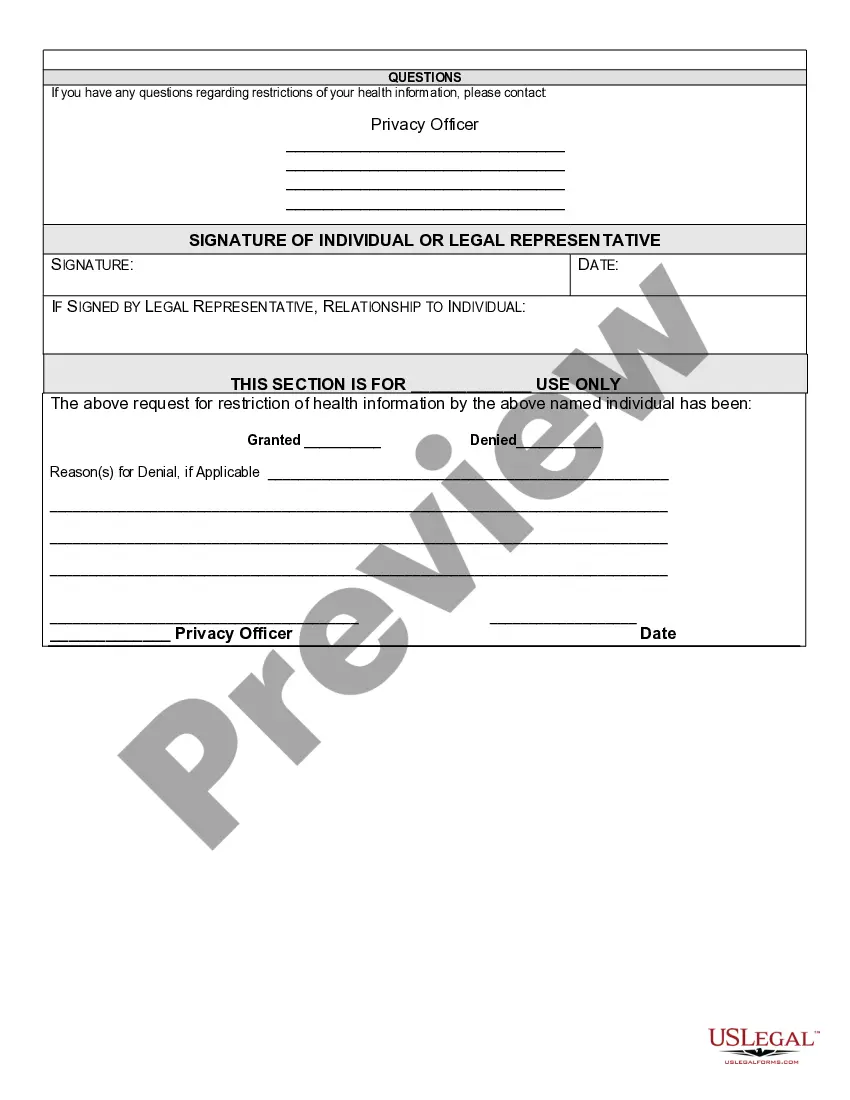
If a covered entity denies access, in whole or in part, to PHI requested by the individual based on one or more permitted grounds, the covered entity must provide a denial in writing to the individual no later than 30 calendar days after the request (or no more than 60 calendar days if the covered entity notified the
Covered entities may disclose protected health information to: Public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability. Public health or other government authorities authorized to receive reports of child abuse and neglect.
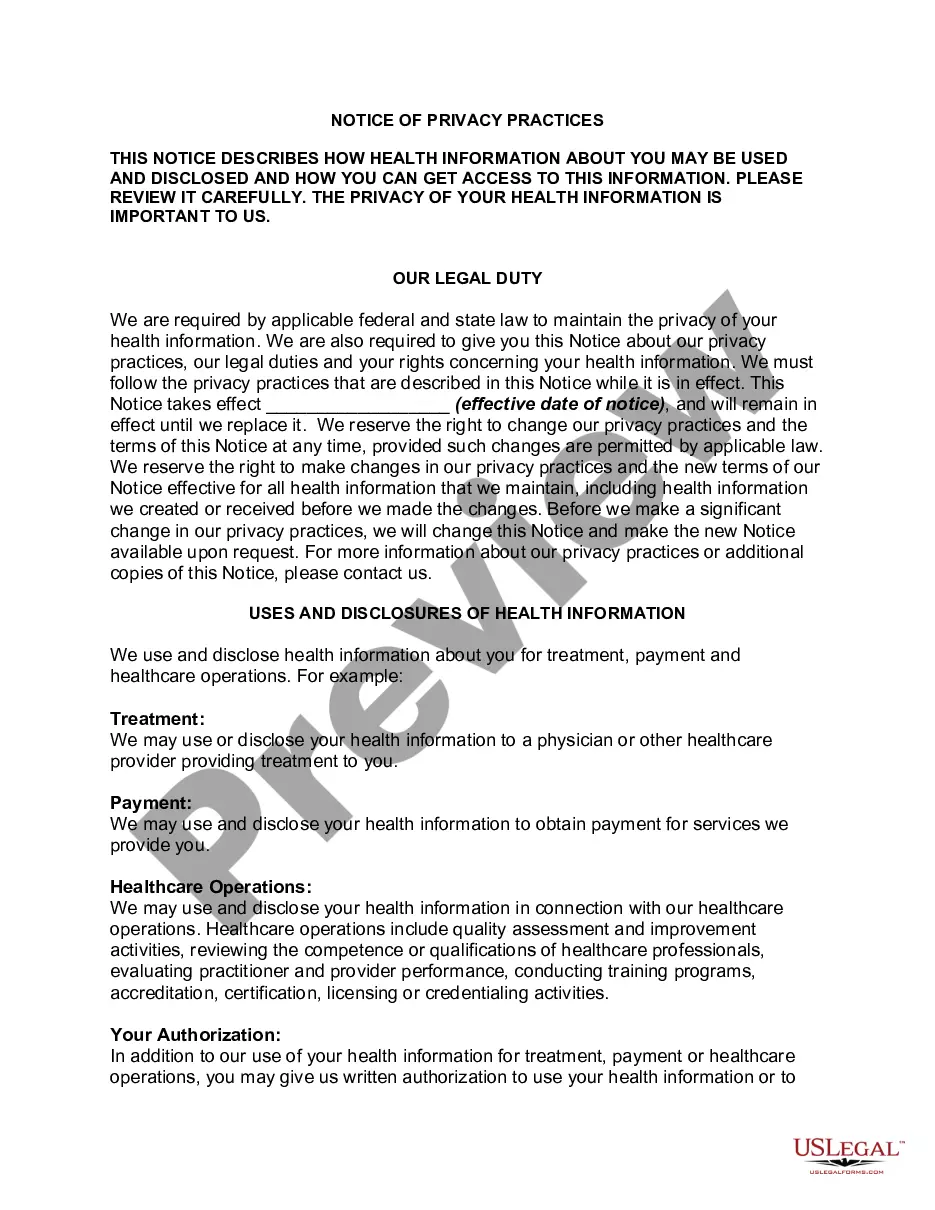
Since its initial adoption, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule has granted individuals the right to request restrictions regarding the use and disclosure of their protected health information (PHI) for treatment, payment, and healthcare operations (TPO).
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
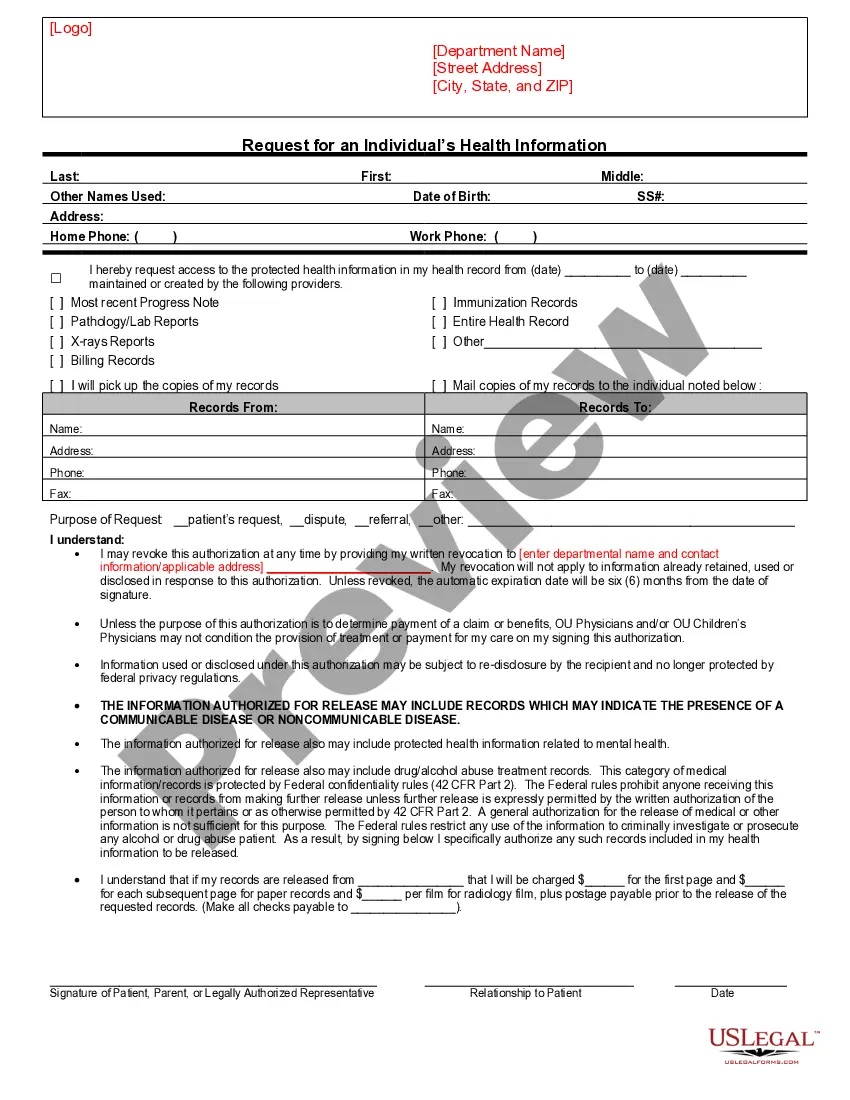
What is a patient required to do in order for a request to restrict the use or disclosure of their PHI to their health plan to be granted? The Privacy Rule allows for a patient to request that no information be shared with others even to the point of not acknowledging the patient's presence in the covered entity.
Unless otherwise required by law, the facility must agree to a patient's request for restrictions or limitations for disclosures to the patient's health plan for payment or health care operations purposes if the patient has paid out of pocket in full for the health care item or service and the PHI pertains solely to
One fact sheet addresses Permitted Uses and Disclosures for Health Care Operations, and clarifies that an entity covered by HIPAA (covered entity), such as a physician or hospital, can disclose identifiable health information (referred to in HIPAA as protected health information or PHI) to another covered entity (or
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
Covered entities may disclose protected health information to: Public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability. Public health or other government authorities authorized to receive reports of child abuse and neglect.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).