Indiana Authorization to Use or Disclose Protected Health Information
Description
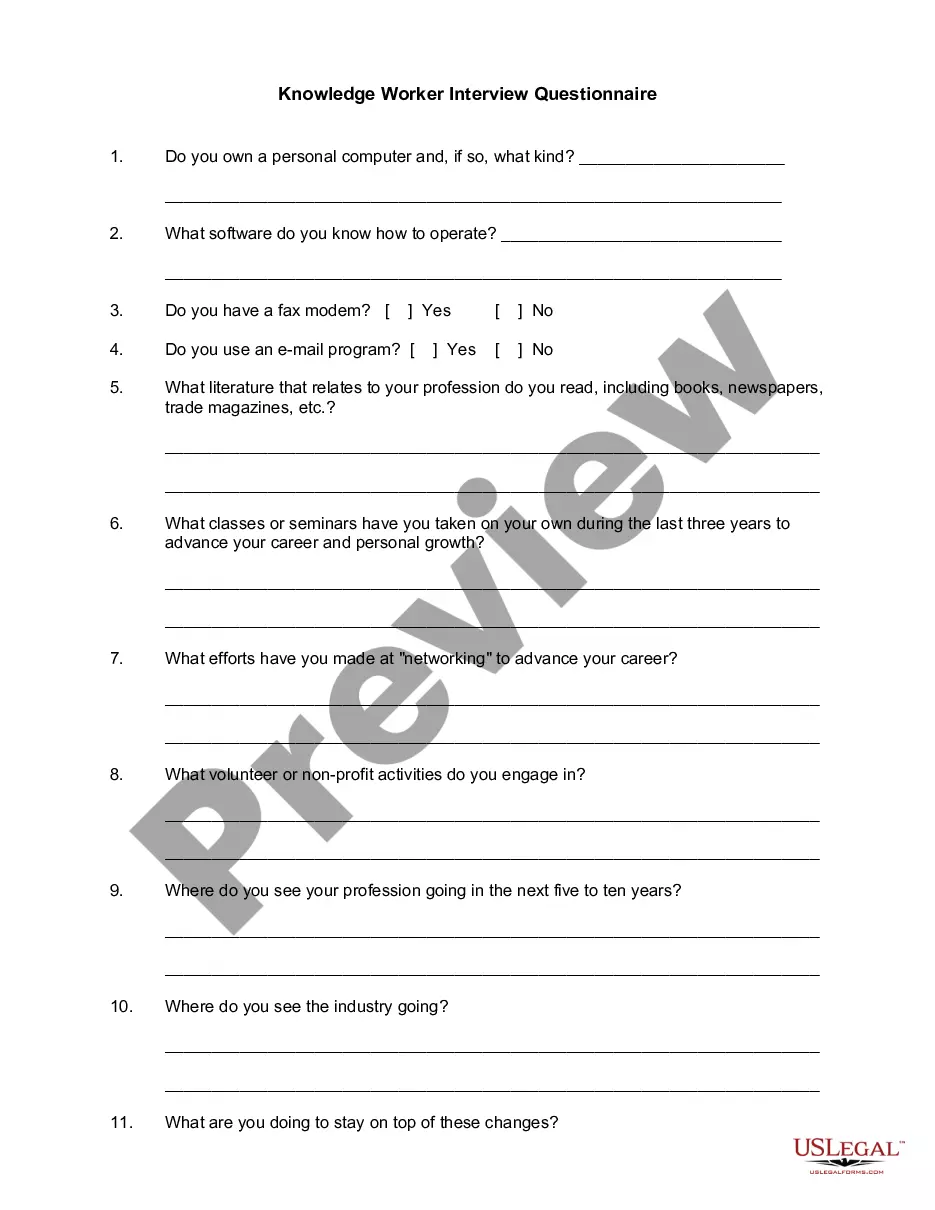
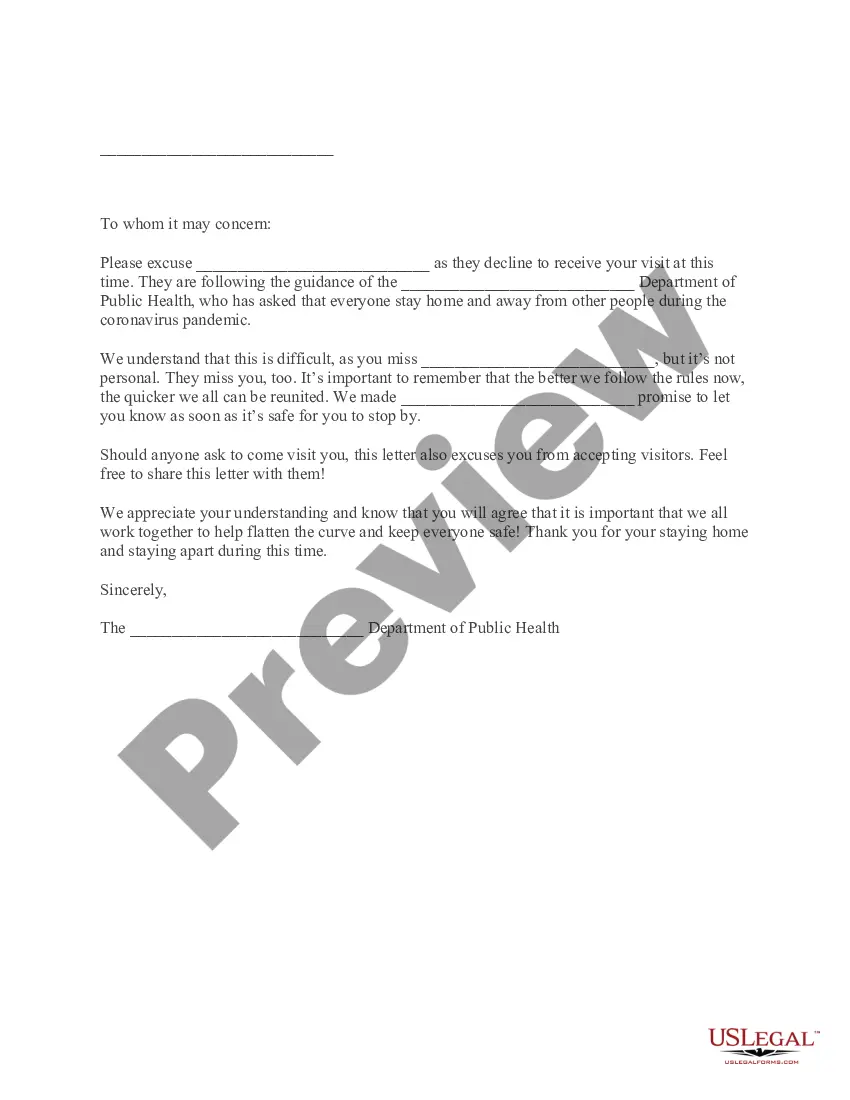
How to fill out Authorization To Use Or Disclose Protected Health Information?
Are you presently in a circumstance where you require to have documents for both professional or personal purposes almost every day.
There are many authorized document templates available online, but finding ones you can trust isn't simple.
US Legal Forms offers thousands of template documents, such as the Indiana Authorization to Use or Disclose Protected Health Information, that are designed to comply with state and federal regulations.
Select the pricing plan you prefer, fill in the required information to create your account, and pay for the transaction using PayPal or a credit card.
Choose a convenient document format and download your copy. You can access all the document templates you have purchased in the My documents menu. You can obtain another copy of the Indiana Authorization to Use or Disclose Protected Health Information at any time, if needed. Just click the desired form to download or print the document template. Use US Legal Forms, one of the largest collections of legal forms, to save time and avoid errors. The service offers professionally created legal document templates that you can utilize for a range of purposes. Create an account on US Legal Forms and start making your life a bit easier.
- If you are already acquainted with the US Legal Forms website and have an account, just Log In.
- After that, you can download the Indiana Authorization to Use or Disclose Protected Health Information template.
- If you don't have an account and want to start using US Legal Forms, follow these steps.
- Obtain the form you need and ensure it is for the correct city/state.
- Use the Review button to scrutinize the form.
- Check the description to ensure you have selected the correct form.
- If the form isn't what you're seeking, use the Search box to find a form that meets your needs and requirements.
- Once you find the appropriate form, click Buy now.
Form popularity
FAQ
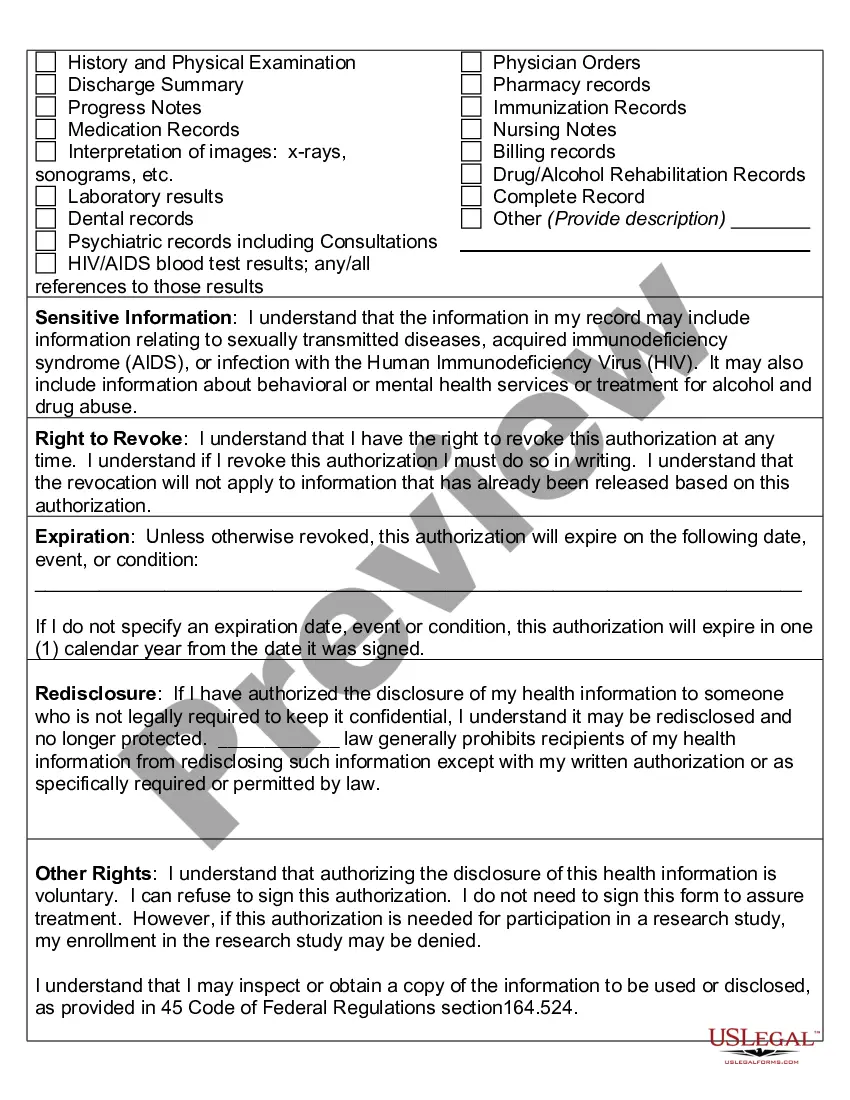
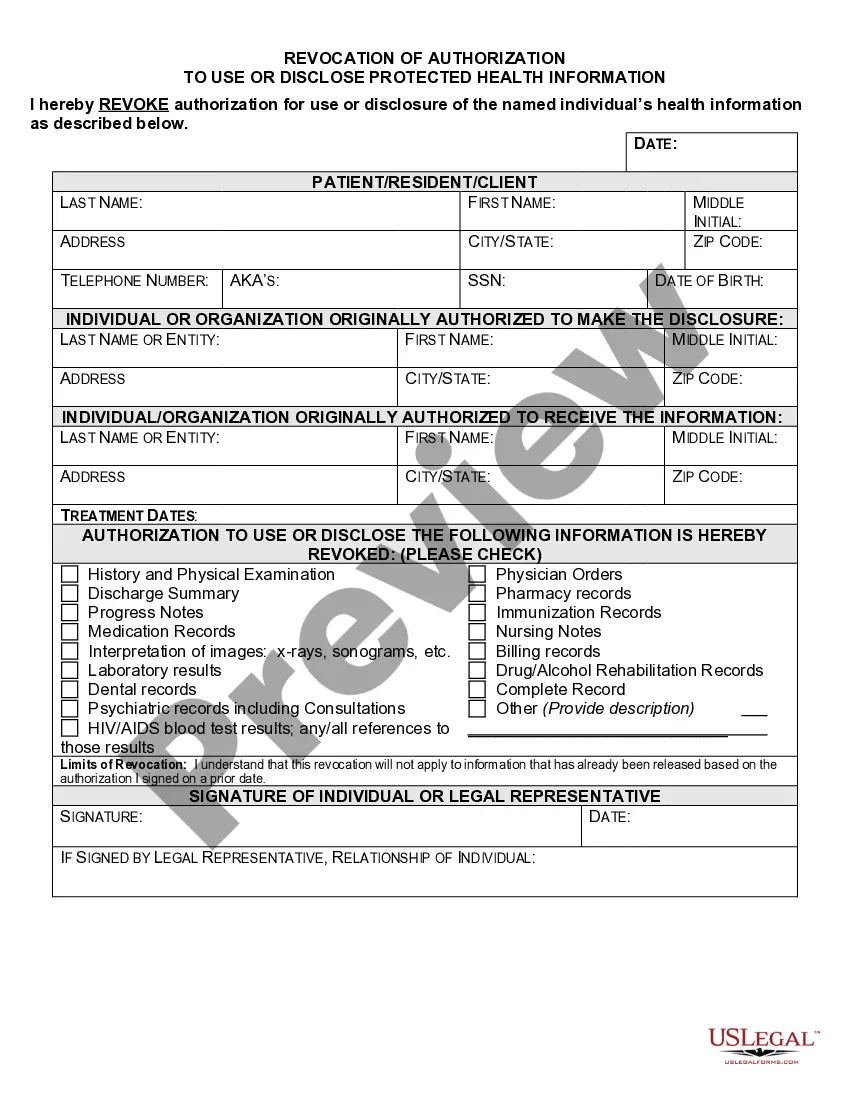
What are two required elements of an authorization needed to disclose PHI? Response Feedback: All authorizations to disclose PHI must have an expiration date and provide an avenue for the patient to revoke his or her authorization. What does the term "Disclosure" mean?
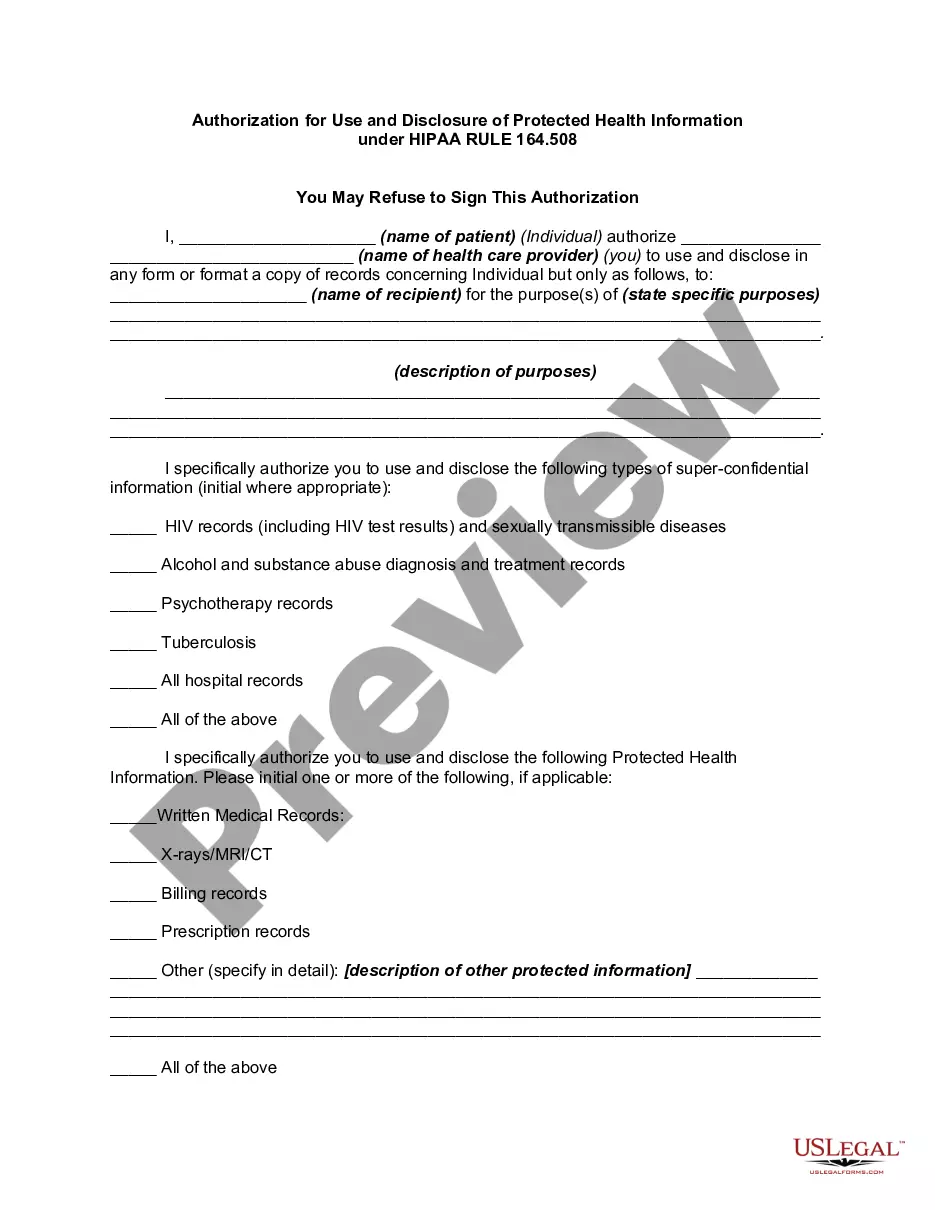
Under the HIPAA Privacy Rule, a covered entity must disclose protected health information in only two situations: (a) to individuals (or their personal representatives) specifically when they request access to, or an accounting of disclosures of, their protected health information; and (b) to the Department of Health
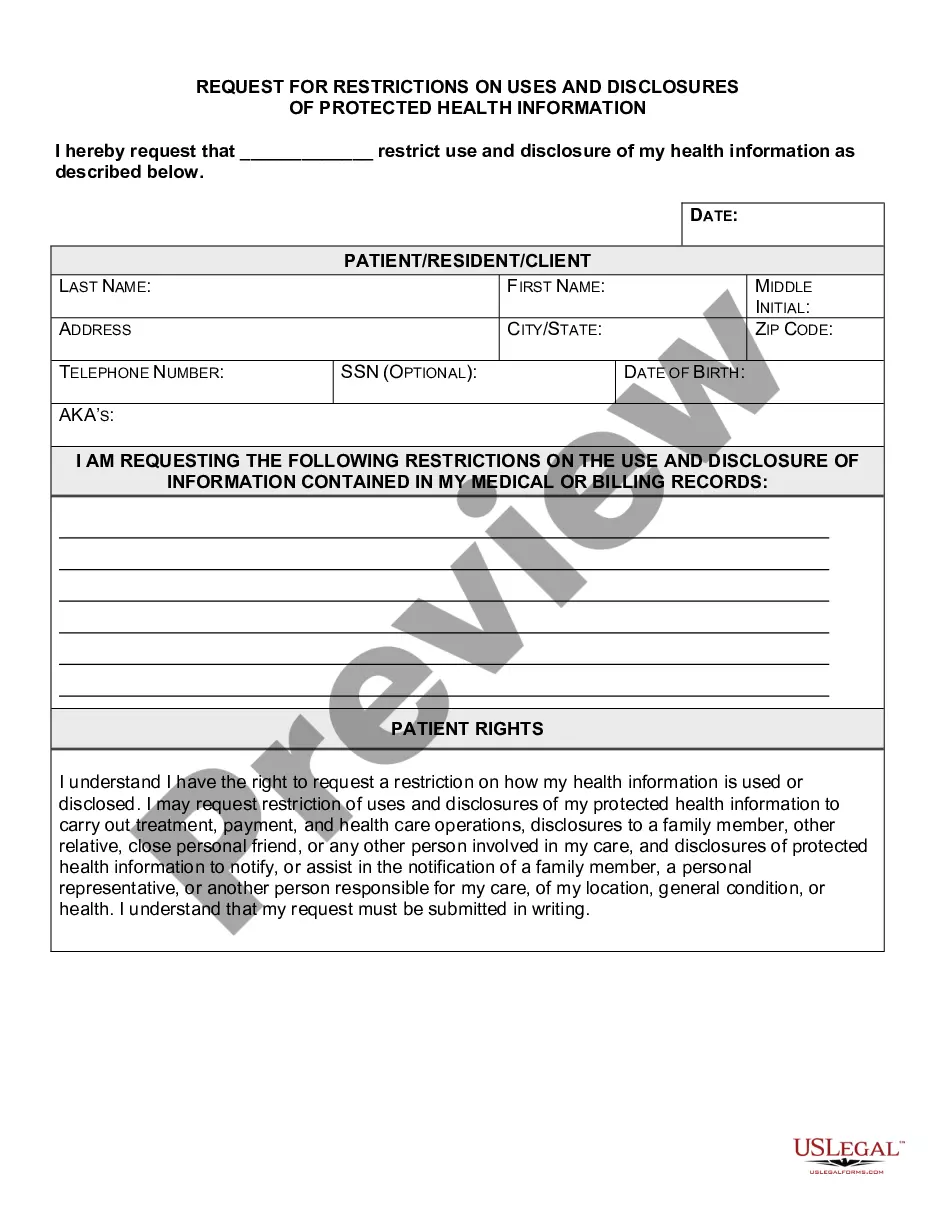
However, PHI can be used and disclosed without a signed or verbal authorization from the patient when it is a necessary part of treatment, payment, or healthcare operations. The Minimum Necessary Standard Rule states that only the information needed to get the job done should be provided.
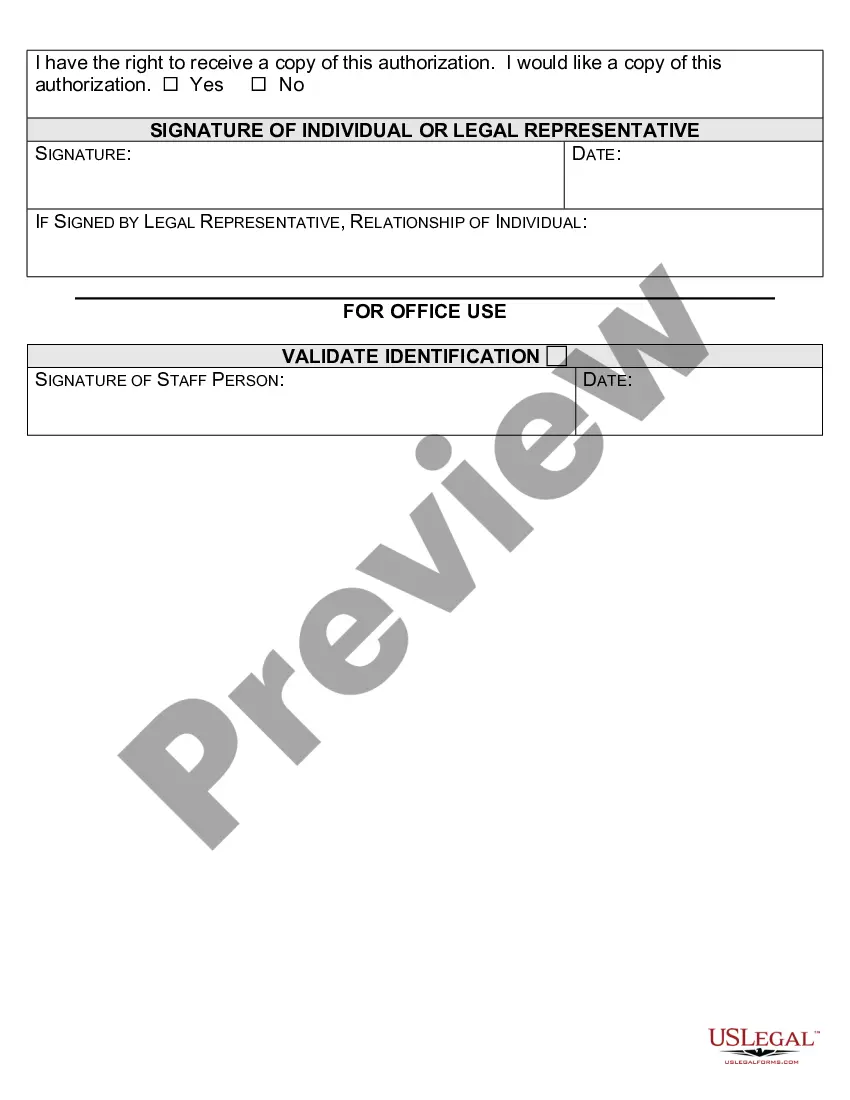
In general, a covered entity may only use or disclose PHI if either: (1) the HIPAA Privacy Rule specifically permits or requires it; or (2) the individual who is the subject of the information gives authorization in writing.
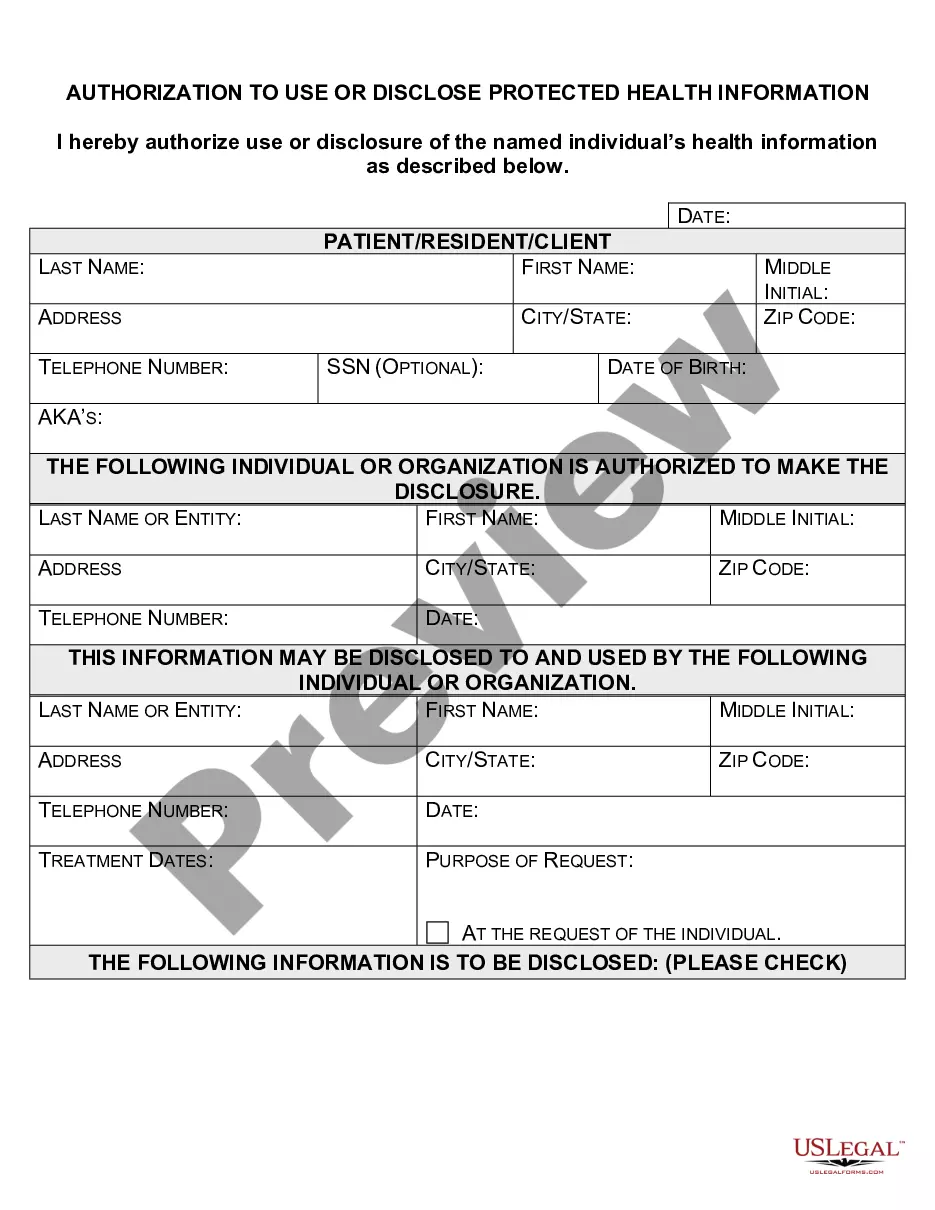
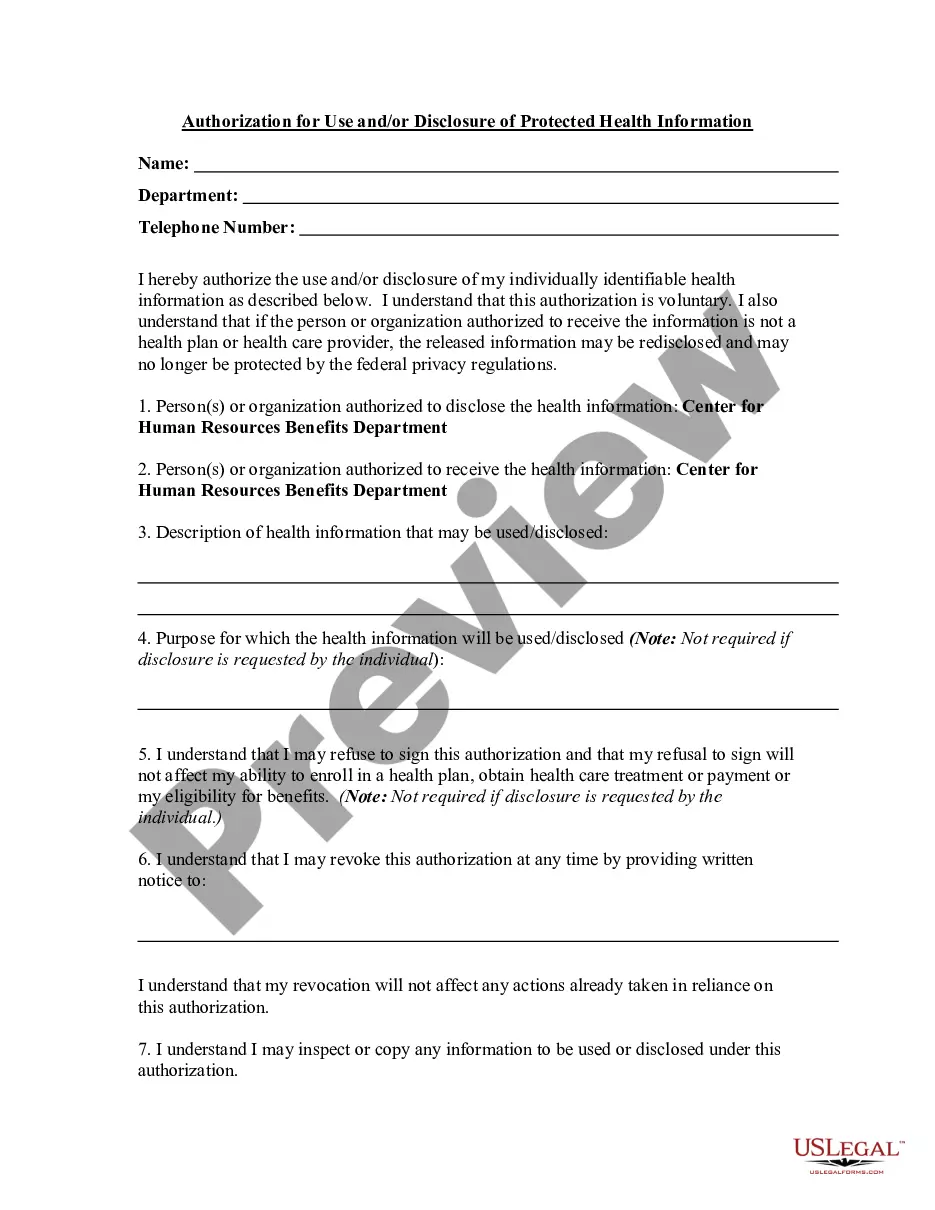
A HIPAA authorization is a detailed document in which specific uses and disclosures of protected health are explained in full. By signing the authorization, an individual is giving consent to have their health information used or disclosed for the reasons stated on the authorization.
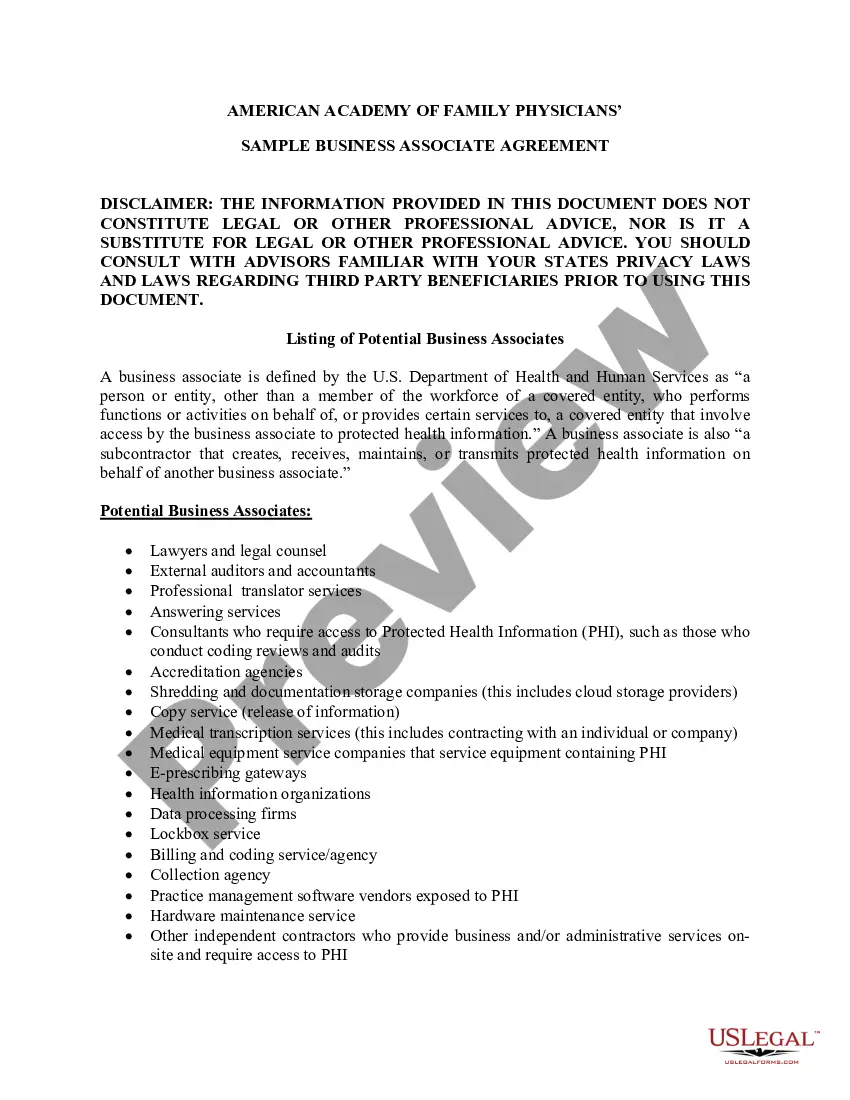
A patient authorization is not required for disclosure of PHI between Covered Entities if the disclosure is needed for purposes of treatment or payment or for healthcare operations. You may disclose the PHI as long as you receive a request in writing.
The HIPAA Privacy Rule requires that an individual provide signed authorization to a covered entity, before the entity may use or disclose certain protected health information (PHI).
Valid HIPAA Authorizations: A ChecklistNo Compound Authorizations. The authorization may not be combined with any other document such as a consent for treatment.Core Elements.Required Statements.Marketing or Sale of PHI.Completed in Full.Written in Plain Language.Give the Patient a Copy.Retain the Authorization.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the