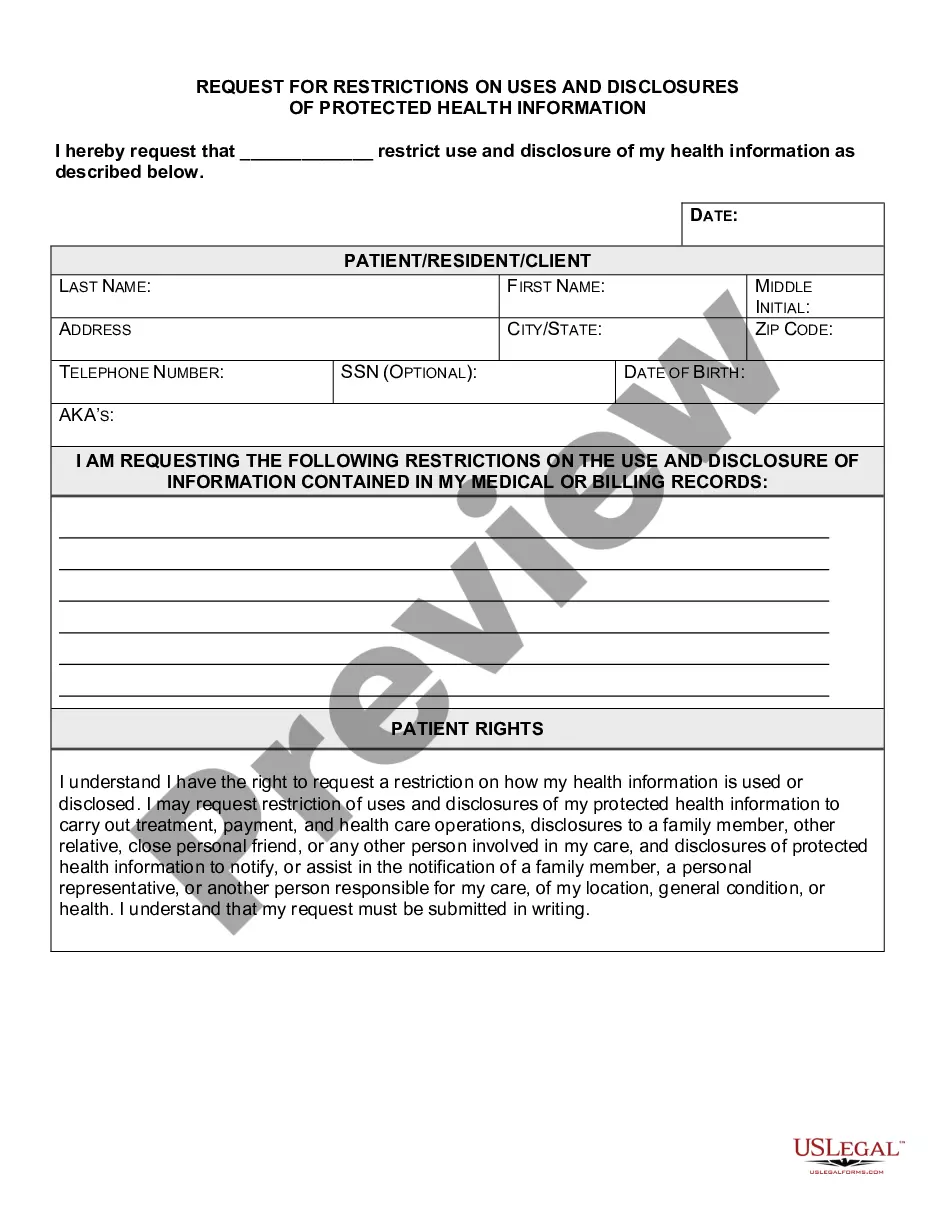
Idaho Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
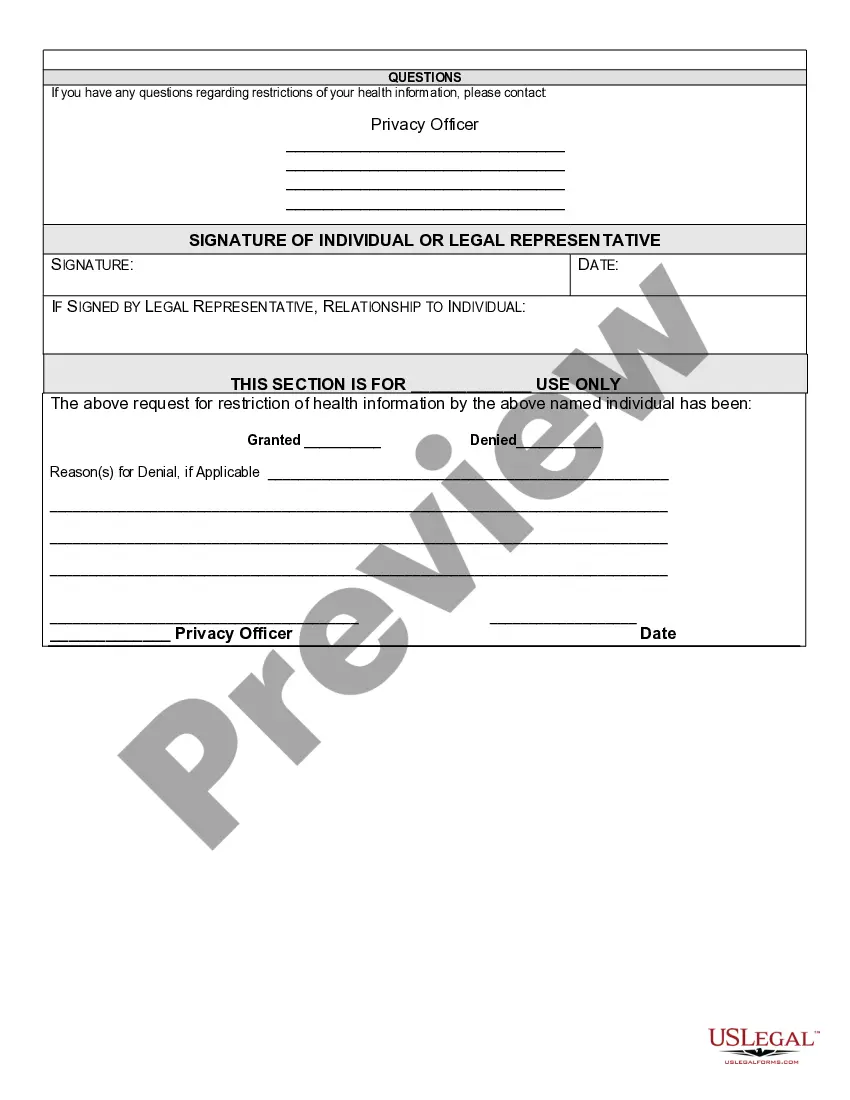
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
Are you in a situation where you need documentation for occasional business or personal activities almost every day? There are numerous legal document templates available on the web, but locating reliable versions can be challenging. US Legal Forms offers thousands of form templates, such as the Idaho Request for Restrictions on Uses and Disclosures of Protected Health Information, which are designed to comply with federal and state requirements.
If you are already familiar with the US Legal Forms website and have an account, simply Log In. After that, you can download the Idaho Request for Restrictions on Uses and Disclosures of Protected Health Information template.
If you do not have an account and wish to start using US Legal Forms, follow these instructions.
Access all the document templates you have purchased in the My documents menu. You can download an additional copy of Idaho Request for Restrictions on Uses and Disclosures of Protected Health Information at any time, if needed. Simply click on the desired form to download or print the document template.
Utilize US Legal Forms, one of the largest collections of legal forms, to save time and avoid mistakes. The service offers professionally created legal document templates that can be used for various purposes. Create an account on US Legal Forms and start making your life easier.
- Obtain the form you need and ensure it is for the correct area/region.
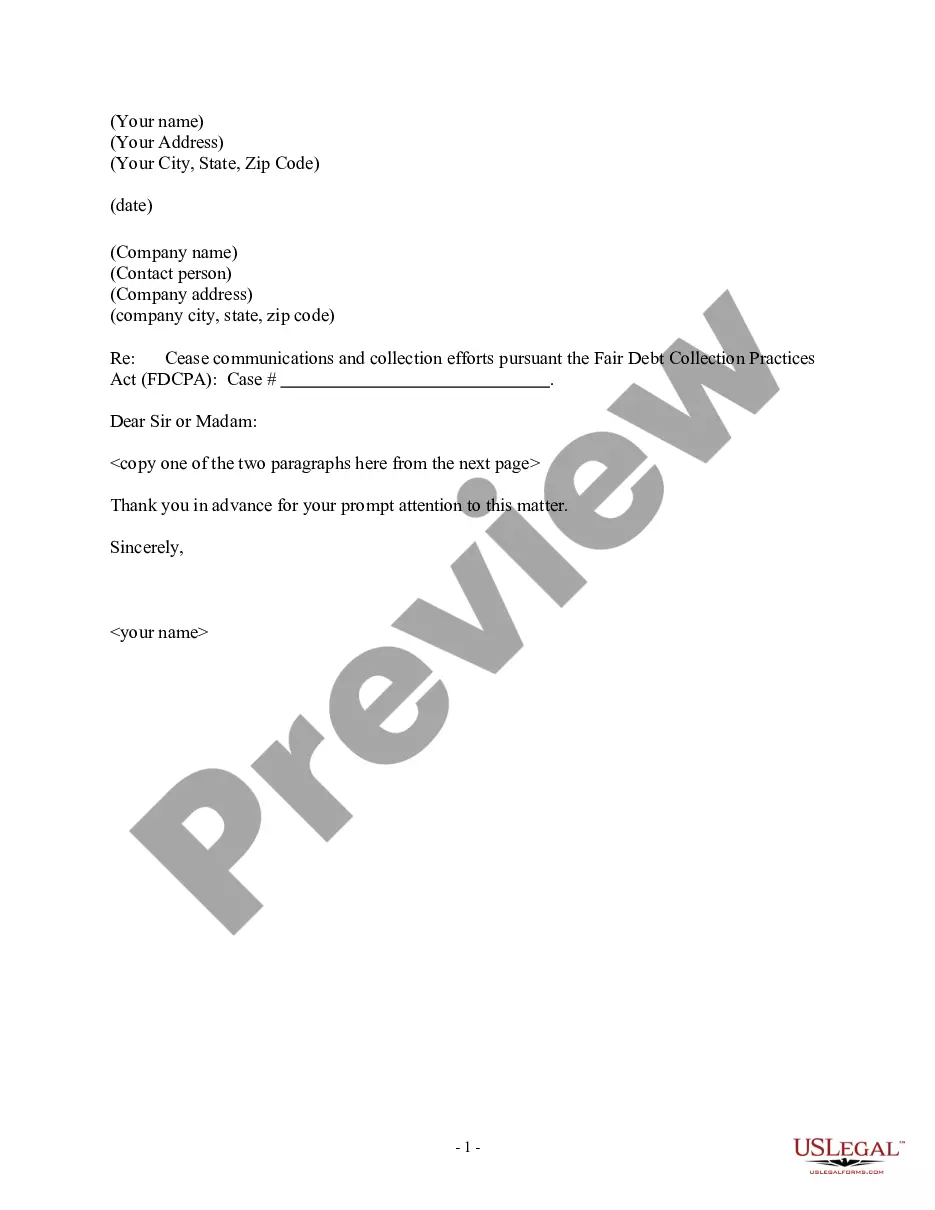
- Use the Preview button to review the form.
- Read the description to ensure you have selected the correct form.
- If the form is not what you are looking for, utilize the Search area to find the form that meets your needs.
- Once you have found the right form, click Buy now.
- Select the pricing plan you would like, provide the necessary information to create your account, and complete the transaction with your PayPal or Visa or Mastercard.
- Choose a convenient file format and download your copy.
Form popularity
FAQ
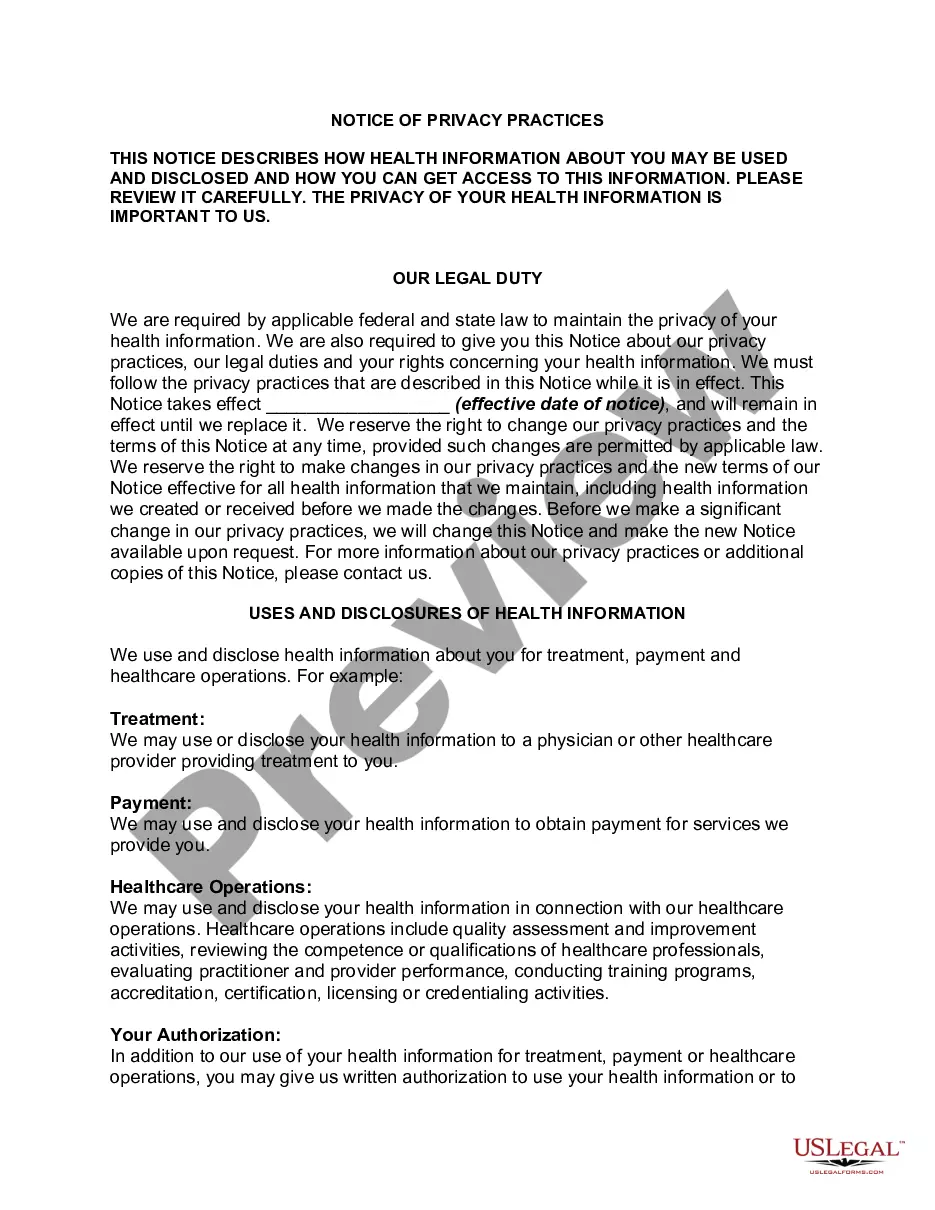
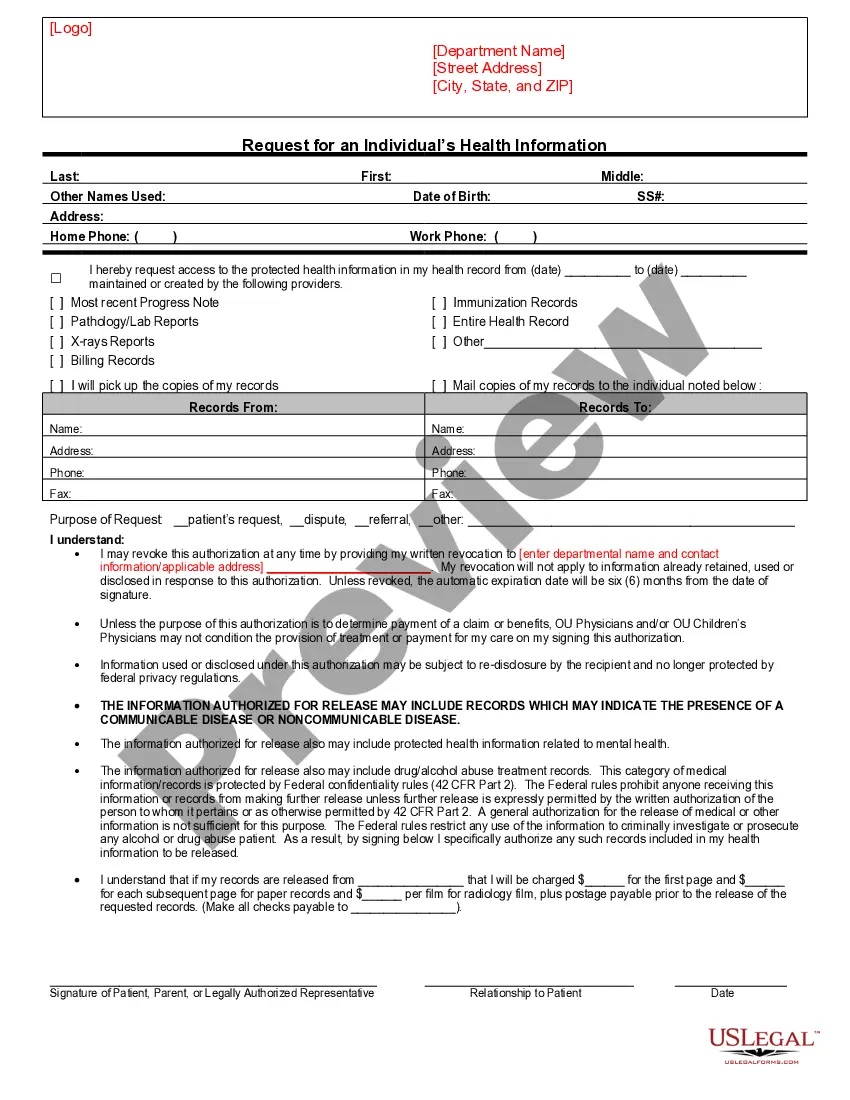
Unauthorized access, use, and disclosure of protected health information occur when someone gains access to personal health information without permission. This could involve a data breach or improper sharing of medical records. Such incidents can lead to serious privacy violations and can be subject to legal consequences. Understanding the Idaho Request for Restrictions on Uses and Disclosures of Protected Health Information is important to protect your data and rights.
Generally speaking, covered entities may disclose PHI to anyone a patient wants. They may also use or disclose PHI to notify a family member, personal representative, or someone responsible for the patient's care of the patient's location, general condition, or death.
You can share confidential information without consent if it is required by law, or directed by a court, or if the benefits to a child or young person that will arise from sharing the information outweigh both the public and the individual's interest in keeping the information confidential.
Regardless of the method by which de-identification is achieved, the Privacy Rule does not restrict the use or disclosure of de-identified health information, as it is no longer considered protected health information, according to HHS.
More generally, HIPAA allows the release of information without the patient's authorization when, in the medical care providers' best judgment, it is in the patient's interest. Despite this language, medical care providers are very reluctant to release information unless it is clearly allowed by HIPAA.
HIPAA Exceptions DefinedTo public health authorities to prevent or control disease, disability or injury. To foreign government agencies upon direction of a public health authority. To individuals who may be at risk of disease. To family or others caring for an individual, including notifying the public.
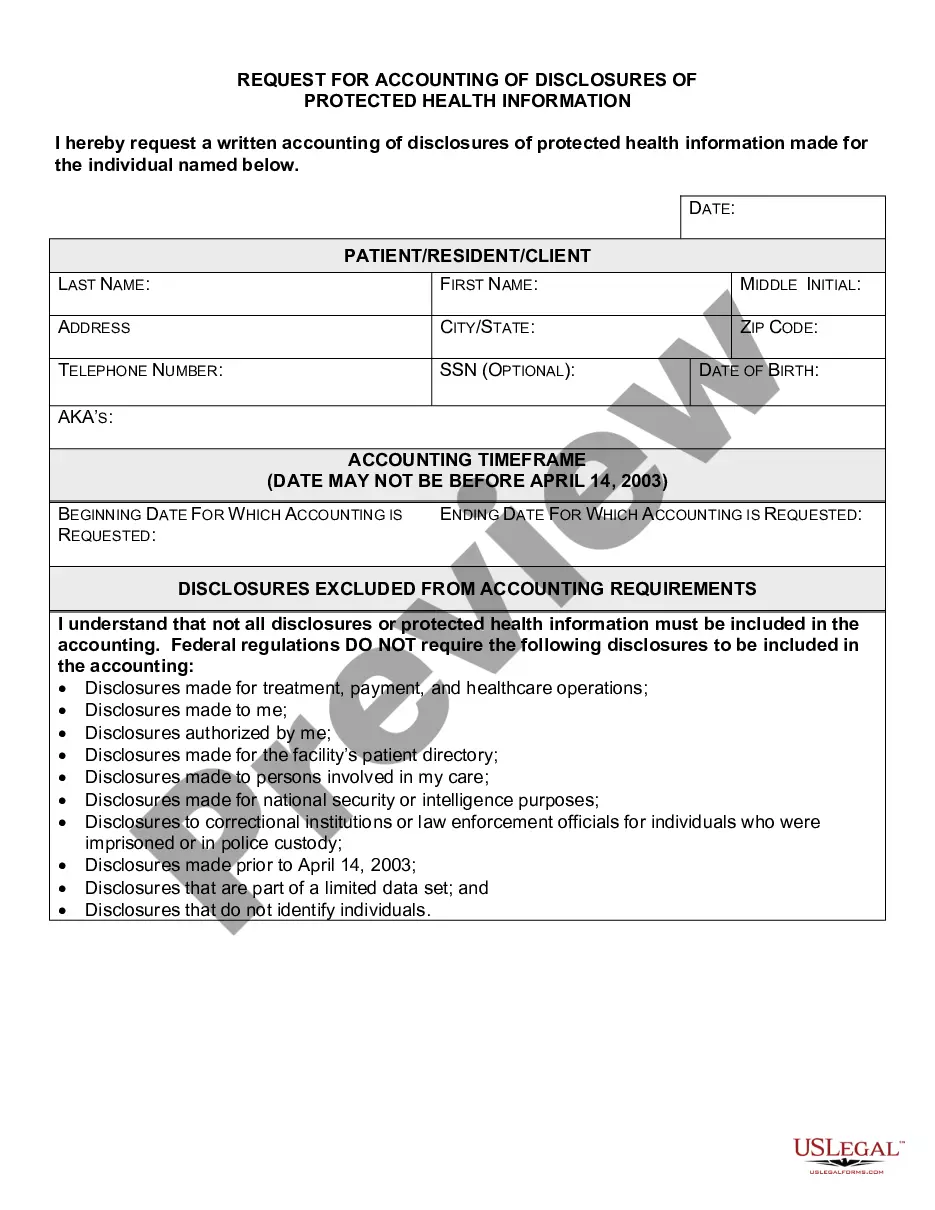
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.
A covered entity must agree to an individual's request to restrict disclosure to health plan if the individual or person on individual's behalf pays for the item or service out of pocket in full: For payment or healthcare operations. Unless required by law.