Florida Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
Are you presently in a role where you require documents for either business or personal activities almost every day.
There are numerous genuine document templates available online, but finding ones you can trust is challenging.
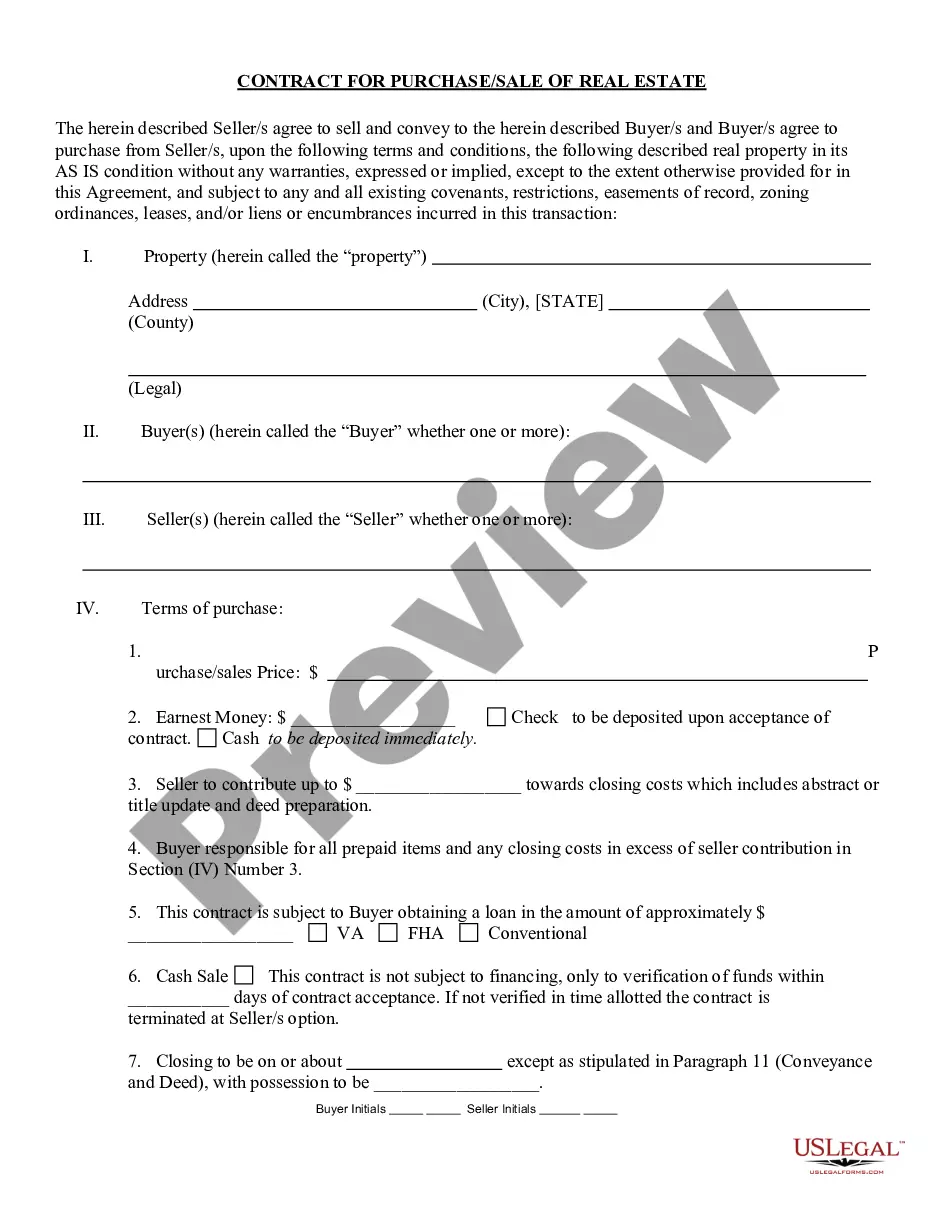
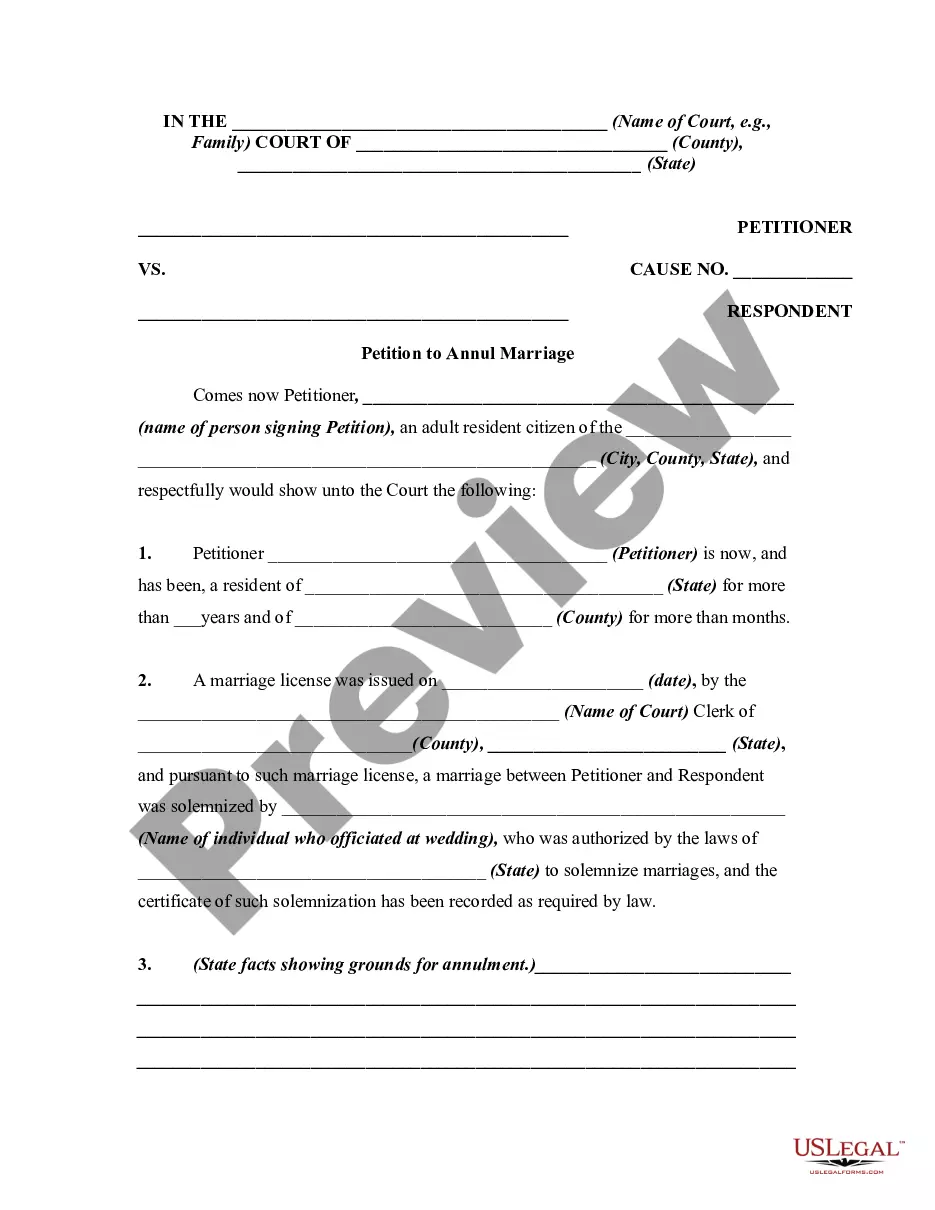
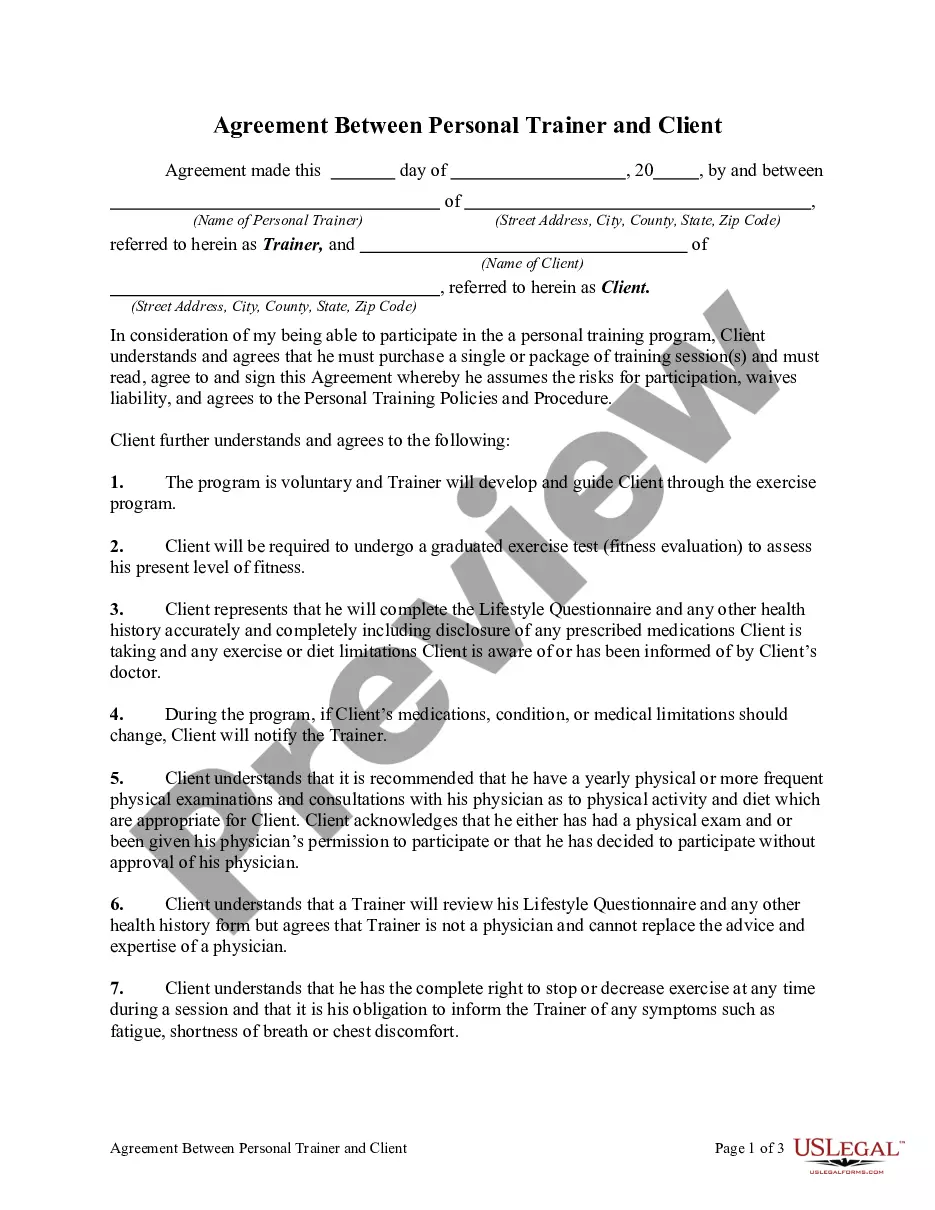
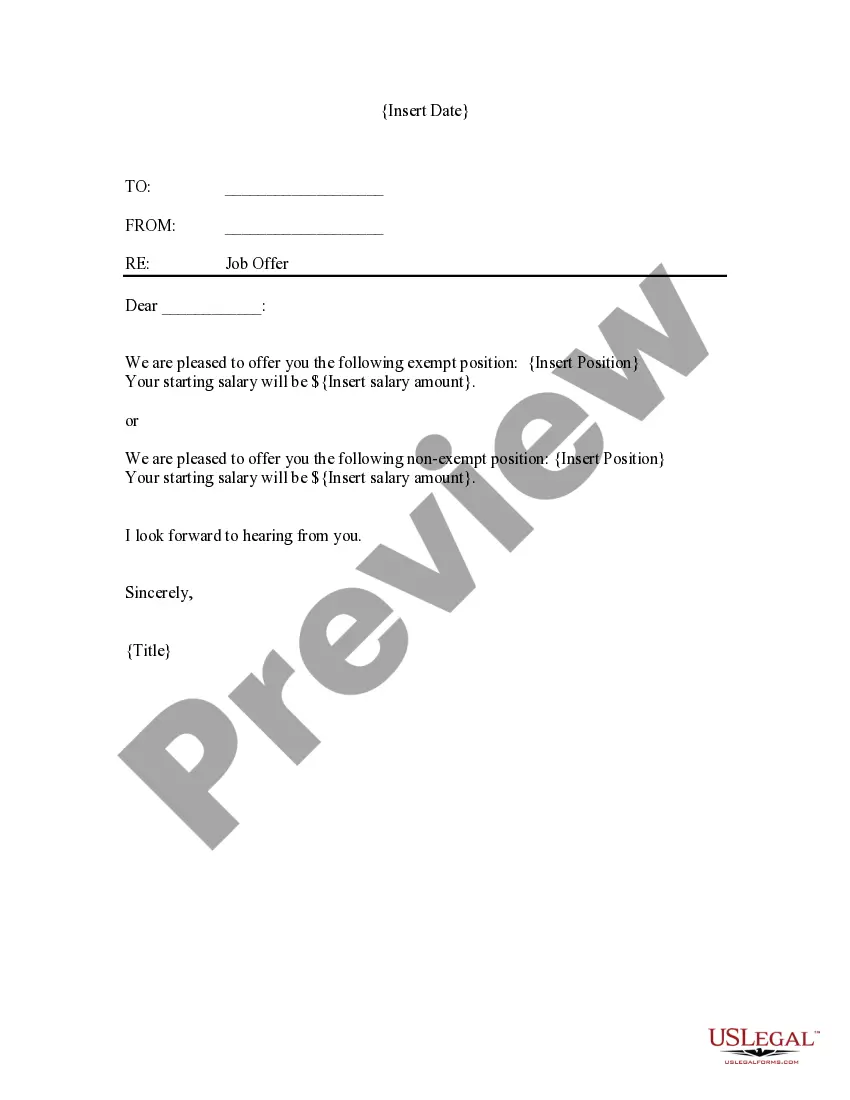
US Legal Forms offers a wide array of form templates, such as the Florida Sample COBRA Enrollment and/or Waiver Letter, which are designed to comply with state and federal regulations.
Once you locate the correct form, click Purchase now.
Choose the pricing plan you desire, fill in the necessary information to set up your payment method, and pay for the transaction using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Then, you can download the Florida Sample COBRA Enrollment and/or Waiver Letter template.
- If you do not have an account and wish to start using US Legal Forms, follow these instructions.
- Retrieve the form you need and ensure it is for the correct city/region.
- Utilize the Review button to examine the form.
- Check the description to ensure that you have selected the right form.
- If the form isn’t what you need, use the Search field to find the form that meets your requirements.
Form popularity
FAQ
To elect COBRA insurance in Florida, an individual must experience one of the following:Quit their job.Be fired unless it was due to gross misconduct.Have their hours reduced, and they no longer qualify for their employer's health plan because they are no longer considered full time.Retire.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive. You are now responsible for the entire insurance premium, whereas your previous employer subsidized a portion of that as a work benefit.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
To elect COBRA insurance in Florida, an individual must experience one of the following:Quit their job.Be fired unless it was due to gross misconduct.Have their hours reduced, and they no longer qualify for their employer's health plan because they are no longer considered full time.Retire.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a landmark federal law, passed in 1985, that provides for continuing group health insurance coverage for some employees and their families after a job loss or other qualifying event.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.