Florida Summary of Rights and Obligations under COBRA
Description
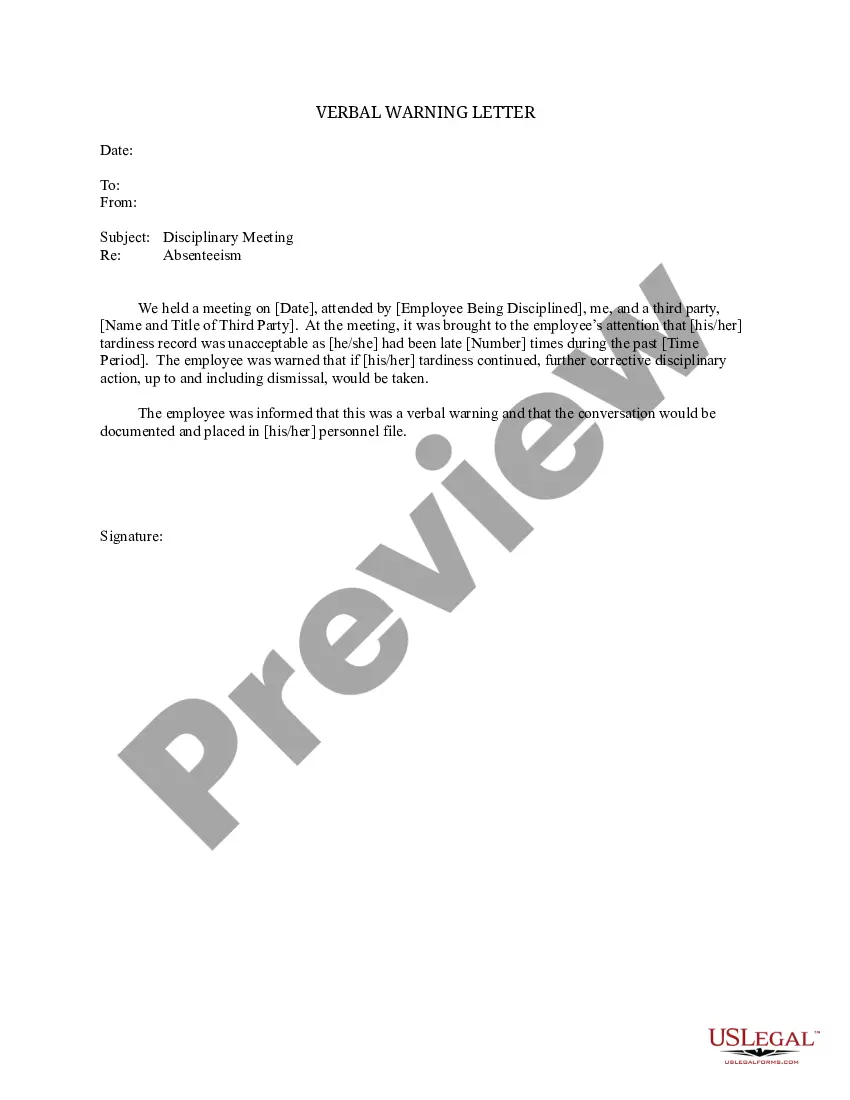
How to fill out Summary Of Rights And Obligations Under COBRA?
Finding the appropriate legal document template can be challenging.
Certainly, there is a multitude of designs available online, but how can you identify the legal form you require.
Utilize the US Legal Forms website. The platform offers thousands of templates, including the Florida Summary of Rights and Obligations under COBRA, which can be utilized for both business and personal purposes.
First, ensure you have selected the proper form for your city/region. You can view the form using the Preview button and read the form details to confirm it is suitable for you.
- All forms are verified by professionals and comply with federal and state regulations.
- If you are already a member, sign in to your account and click the Download button to obtain the Florida Summary of Rights and Obligations under COBRA.
- Use your account to browse the legal forms you have purchased previously.
- Visit the My documents section in your account to obtain another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple steps you can follow.
Form popularity
FAQ
COBRA. The Consolidated Omnibus Budget Reconciliation Act (COBRA) allows employees, retirees, and their families, to continue coverage of health, dental and vision benefits through their employer group plan for limited periods of time under certain circumstances, including: Voluntary or involuntary job loss.
To elect COBRA insurance in Florida, an individual must experience one of the following: Quit their job. Be fired unless it was due to gross misconduct. Have their hours reduced, and they no longer qualify for their employer's health plan because they are no longer considered full time.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive. You are now responsible for the entire insurance premium, whereas your previous employer subsidized a portion of that as a work benefit.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Under Florida COBRA insurance, employees can continue their healthcare coverage for a minimum of 18 months, while their spouses and children may receive coverage for up to three years.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.