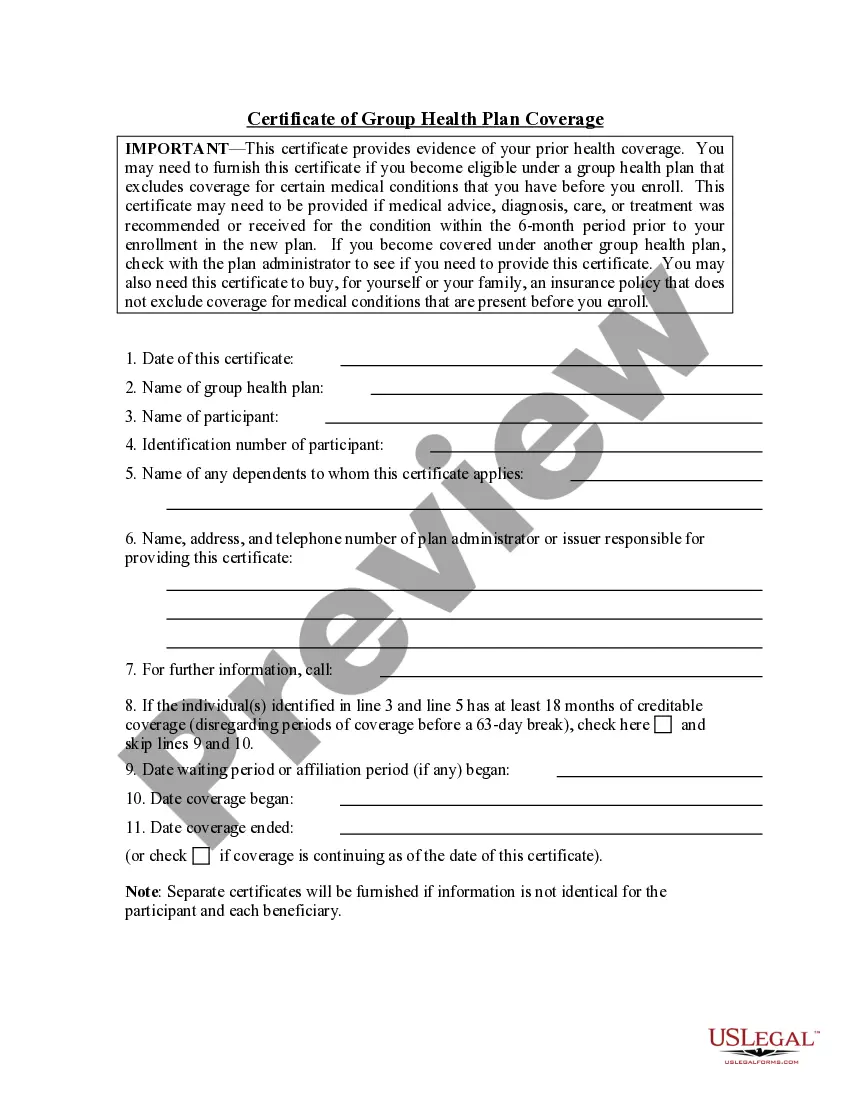
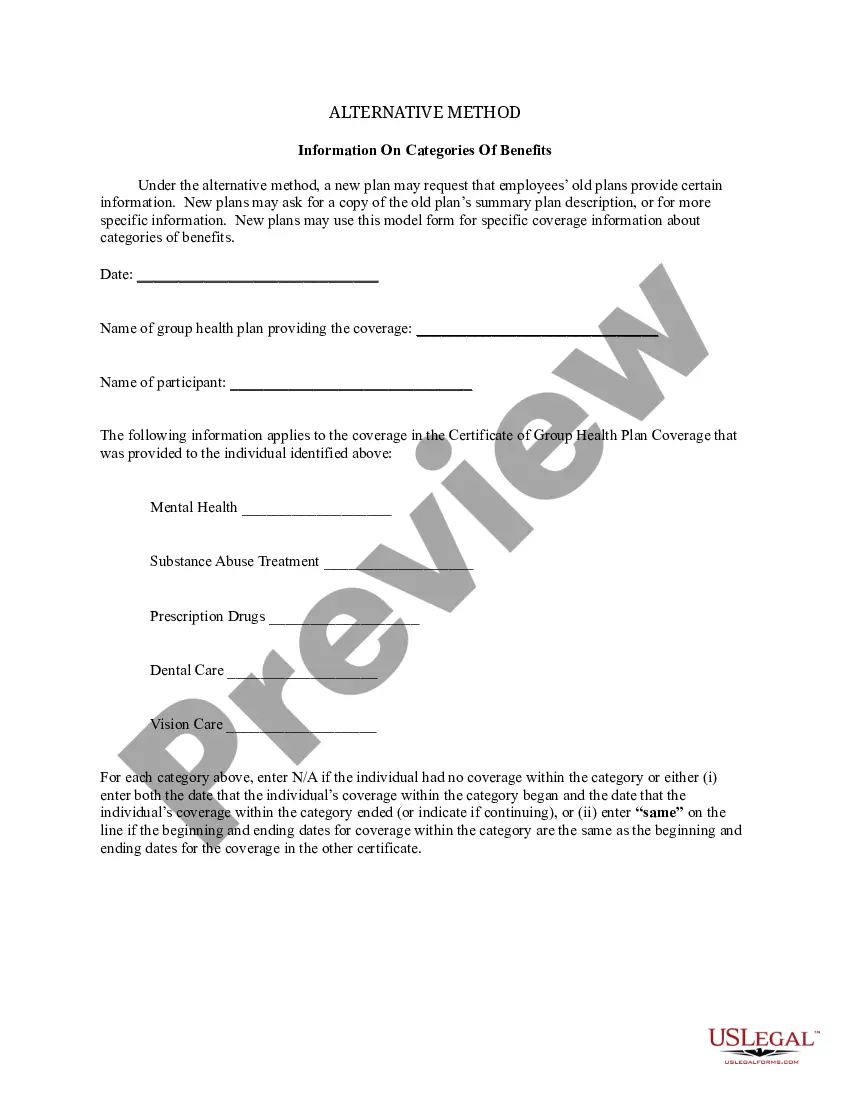
Connecticut Information for Alternative Method of Counting Creditable Coverage
Description
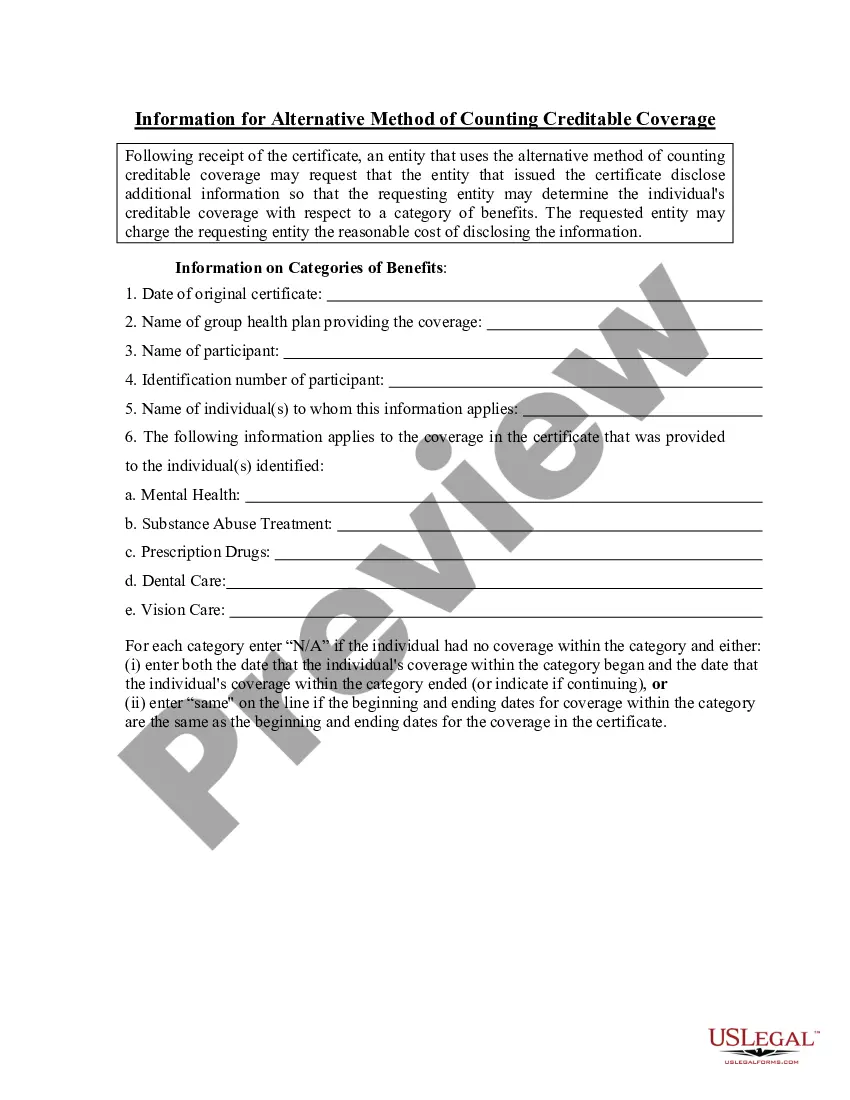
How to fill out Information For Alternative Method Of Counting Creditable Coverage?
Selecting the appropriate legal document template can be challenging.
Undoubtedly, there are numerous themes accessible online, but how will you find the legal format you require.
Utilize the US Legal Forms website. The service provides a vast array of templates, such as the Connecticut Information for Alternative Method of Counting Creditable Coverage, suitable for both business and personal purposes.
You can review the form using the Review button and examine the form details to confirm it is suitable for you.
- All of the forms are reviewed by experts and comply with federal and state regulations.
- If you are currently registered, Log In to your account and then click the Download button to acquire the Connecticut Information for Alternative Method of Counting Creditable Coverage.
- Use your account to search for the legal forms you have previously ordered.
- Proceed to the My documents tab of your account and retrieve another copy of the documents you need.
- If you are a new user of US Legal Forms, here are some simple guidelines for you to follow.
- First, ensure you have selected the correct form for your city/county.
Form popularity
FAQ
A certificate of Creditable Coverage (COCC) is a document provided by your previous insurance carrier that proves that your insurance has ended. This includes the name of the member to whom it applies as well as the coverage effective date and cancelation date.
A group health plan's prescription drug coverage is considered creditable if its actuarial value equals or exceeds the actuarial value of standard Medicare Part D prescription drug coverage, as demonstrated through the use of generally accepted actuarial principles and in accordance with CMS guidelines.
Notices of creditable/non-creditable coverage may be included in annual enrollment materials, sent in separate mailings or delivered electronically.
You should receive a notice from your employer or plan around September of each year, informing you if your drug coverage is creditable. If you have not received this notice, contact your human resources department, drug plan, or benefits manager.
The Notice of Creditable Coverage works as proof of your coverage when you first become eligible for Medicare. Those who have creditable coverage through an employer or union receive a Notice of Creditable Coverage in the mail each year. This notice informs you that your current coverage is creditable.
Non-creditable coverage: A health plan's prescription drug coverage is non-creditable when the amount the plan expects to pay, on average, for prescription drugs for individuals covered by the plan in the coming year is less than that which standard Medicare prescription drug coverage would be expected to pay.
Group health plan sponsors are required to disclose to CMS whether their prescription drug coverage is creditable or non-creditable. This disclosure is required regardless of whether the health plan's coverage is primary or secondary to Medicare.
The notices can also be sent electronically in some instances. As a general rule, a single disclosure notice may be provided to the covered Medicare beneficiary and all of his or her Medicare Part D-eligible dependents covered under the same plan.
Employers that offer prescription drug coverage must provide notices of "creditable" or "non-creditable" coverage to Medicare-eligible employees or covered dependents before each year's Medicare Part D annual enrollment period begins.