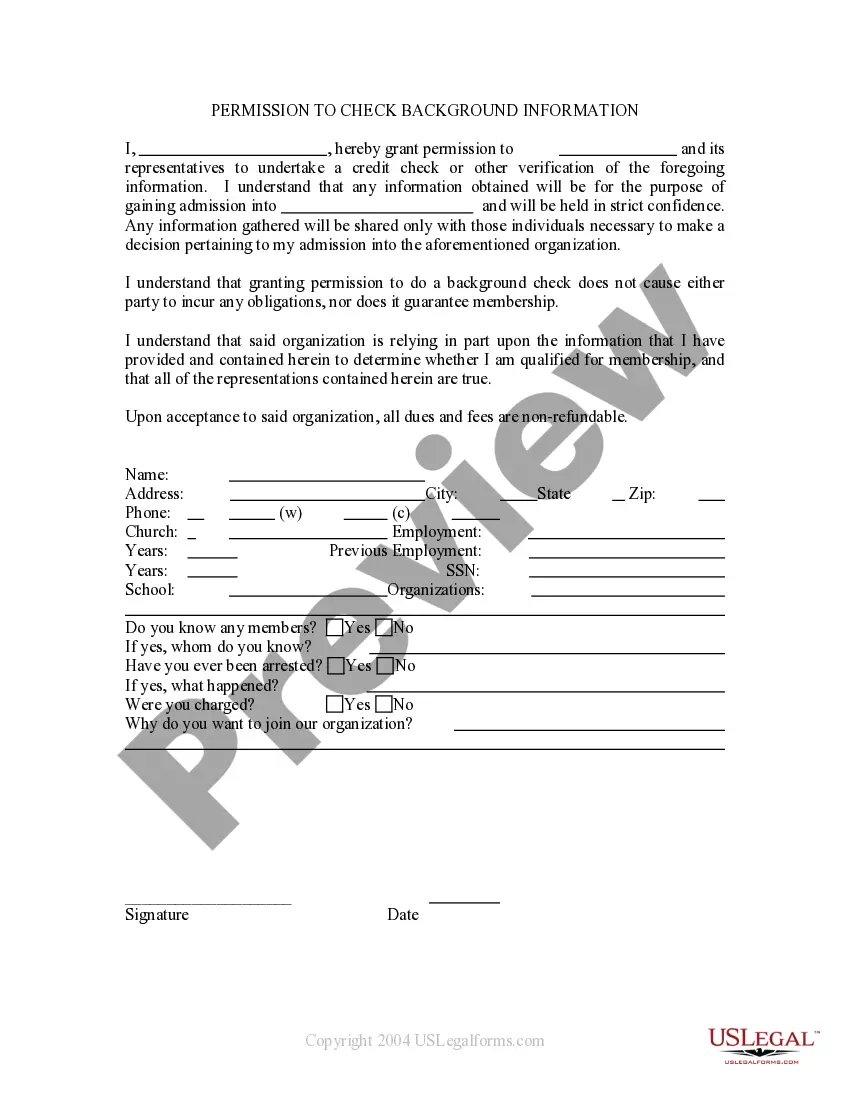
The Arizona COBRA Continuation Coverage Election Form is a crucial document that plays a significant role in ensuring individuals maintain their health insurance coverage after experiencing a qualifying event. COBRA, which stands for Consolidated Omnibus Budget Reconciliation Act, is a federal law that allows employees and their dependents to continue their health insurance coverage for a specified period when certain circumstances cause them to lose their job-based coverage. The Arizona COBRA Continuation Coverage Election Form is the standard form used to elect or decline COBRA coverage in Arizona. It can also be referred to as the COBRA Election Form or COBRA Enrollment Form. This form allows individuals to choose whether to continue their health insurance coverage under their former employer's group plan. The form typically contains a variety of relevant fields and sections, including personal information such as the individual's name, social security number, contact details, and the names of any dependents who were covered under the employer's plan. It also requires essential information regarding the qualifying event, such as the date coverage was lost and the reason for the loss. Additionally, the Arizona COBRA Continuation Coverage Election Form includes sections that outline the available coverage options, duration of coverage, and the associated costs. It is crucial to carefully review this information as it helps individuals make an informed decision regarding whether to elect COBRA coverage or seek alternative options. While there may not be different types of Arizona COBRA Continuation Coverage Election Forms, variations can occur depending on the employer or health insurance provider. This means that individuals may encounter customizations to the form. However, the core content and purpose of the form remain the same — allowing individuals to elect or decline COBRA continuation coverage and maintain essential health insurance benefits during times of transition or job loss. In conclusion, the Arizona COBRA Continuation Coverage Election Form is an essential document for individuals who have lost their job-based health insurance coverage. By accurately completing this form, individuals ensure the continuation of their health insurance benefits throughout the designated coverage period. It is recommended to thoroughly understand the form's content and consider seeking professional advice when making this important decision.
Arizona COBRA Continuation Coverage Election Form
Description
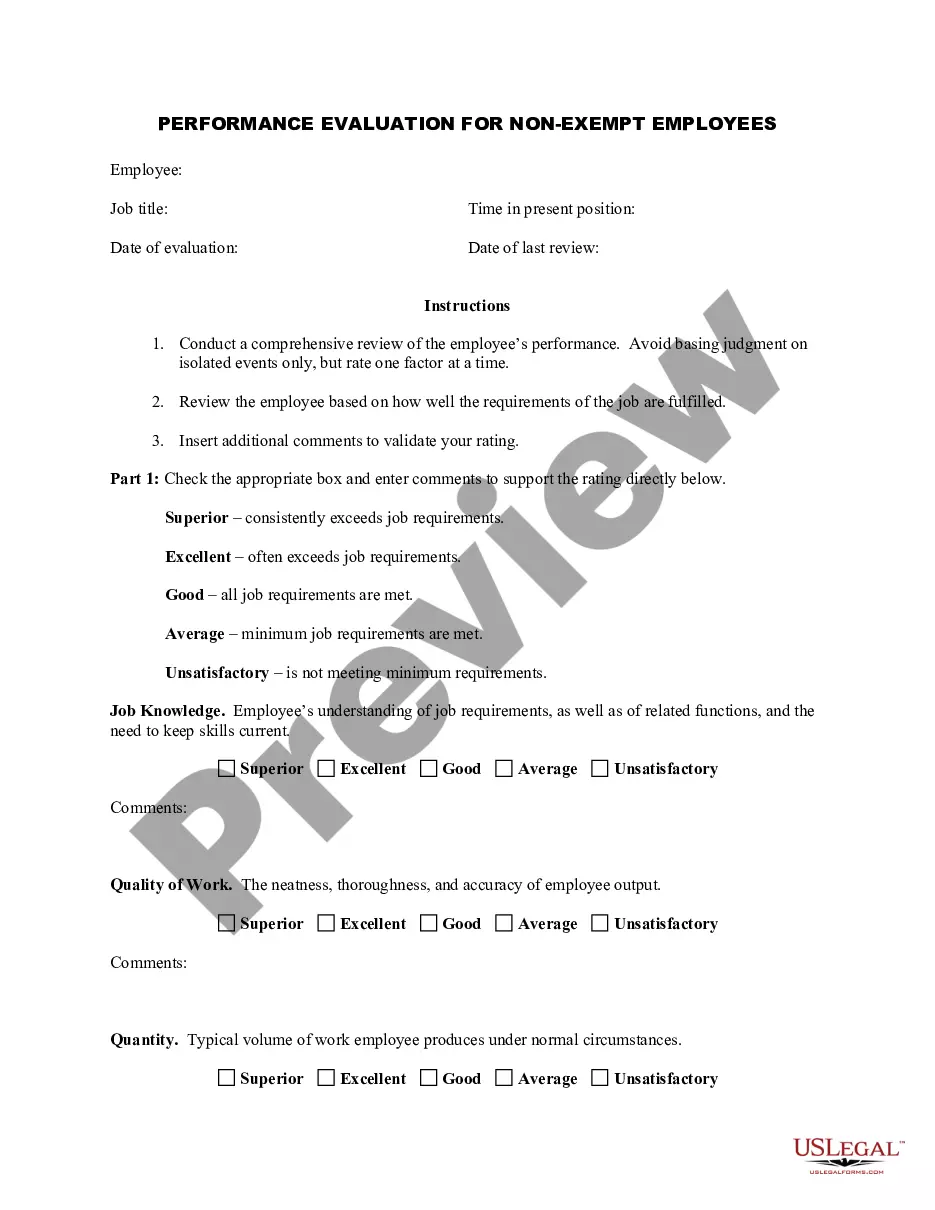
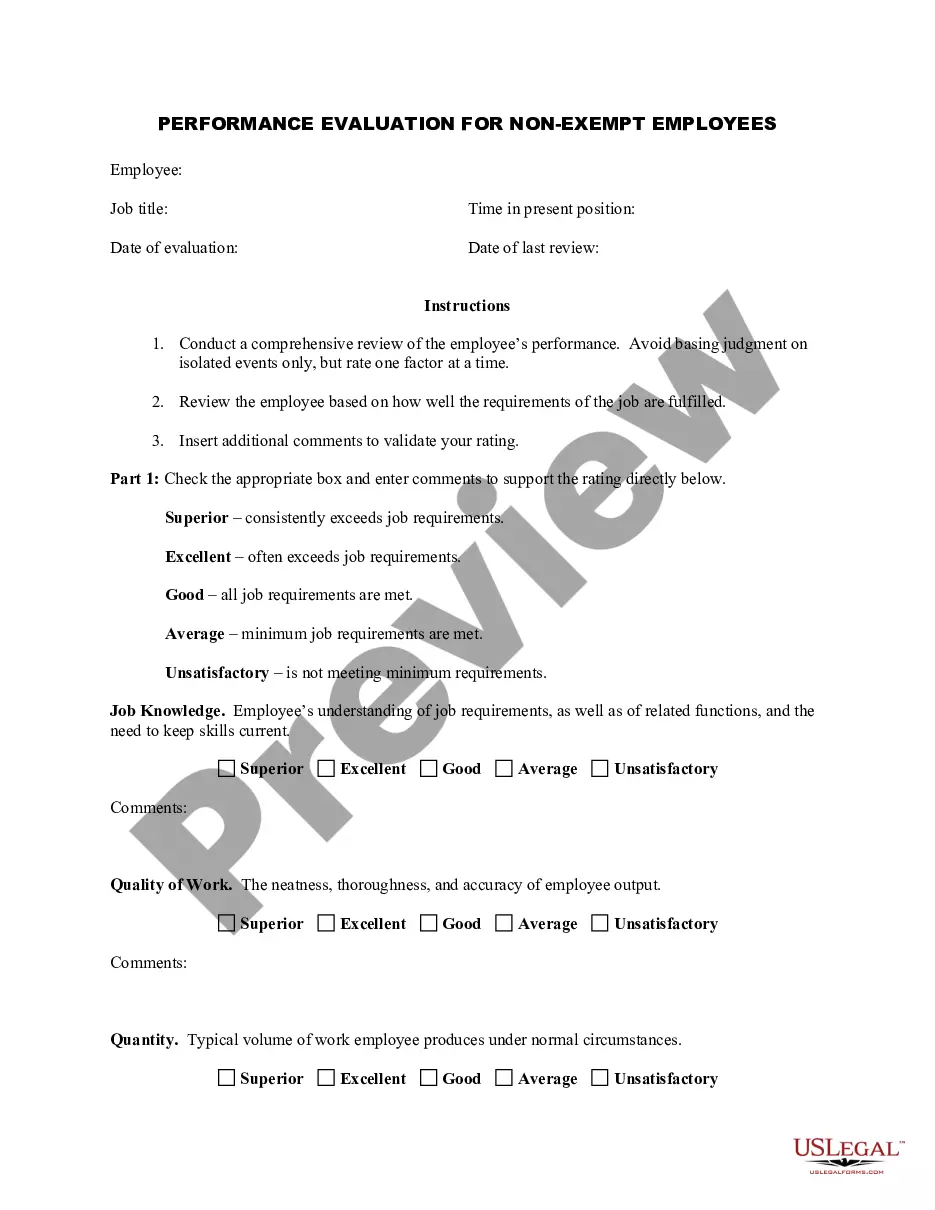
How to fill out Arizona COBRA Continuation Coverage Election Form?
Are you currently in the situation that you require files for sometimes business or individual functions virtually every day? There are plenty of legal record templates available on the net, but locating kinds you can depend on isn`t straightforward. US Legal Forms provides 1000s of type templates, just like the Arizona COBRA Continuation Coverage Election Form, that happen to be composed in order to meet state and federal specifications.
If you are currently familiar with US Legal Forms web site and also have a free account, just log in. Next, it is possible to download the Arizona COBRA Continuation Coverage Election Form template.
Should you not provide an account and would like to start using US Legal Forms, follow these steps:
- Get the type you need and make sure it is for that correct town/area.
- Use the Preview button to review the shape.
- Read the explanation to ensure that you have selected the appropriate type.
- In the event the type isn`t what you are looking for, make use of the Search area to find the type that meets your needs and specifications.
- If you discover the correct type, just click Get now.
- Select the rates program you need, submit the required details to make your bank account, and pay for the order using your PayPal or Visa or Mastercard.
- Select a convenient file structure and download your copy.
Discover all the record templates you possess purchased in the My Forms food selection. You can obtain a additional copy of Arizona COBRA Continuation Coverage Election Form whenever, if needed. Just select the needed type to download or print the record template.
Use US Legal Forms, probably the most comprehensive assortment of legal forms, in order to save time as well as prevent faults. The support provides appropriately produced legal record templates that can be used for an array of functions. Produce a free account on US Legal Forms and initiate generating your life easier.
Form popularity
FAQ
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Your COBRA coverage will begin at the full premium amount. Payment must be received within 45 days after the enrollment form has been received. COBRA will begin the day after active coverage ends. COBRA COVERAGE WILL NOT BEGIN UNTIL PAYMENT IS RECEIVED.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.