Alabama COBRA Continuation Waiver Letter
Description
How to fill out COBRA Continuation Waiver Letter?
Are you at the point where you require documentation for either commercial or personal purposes almost daily.
There are numerous legal document templates accessible online, but finding reliable forms can be challenging.
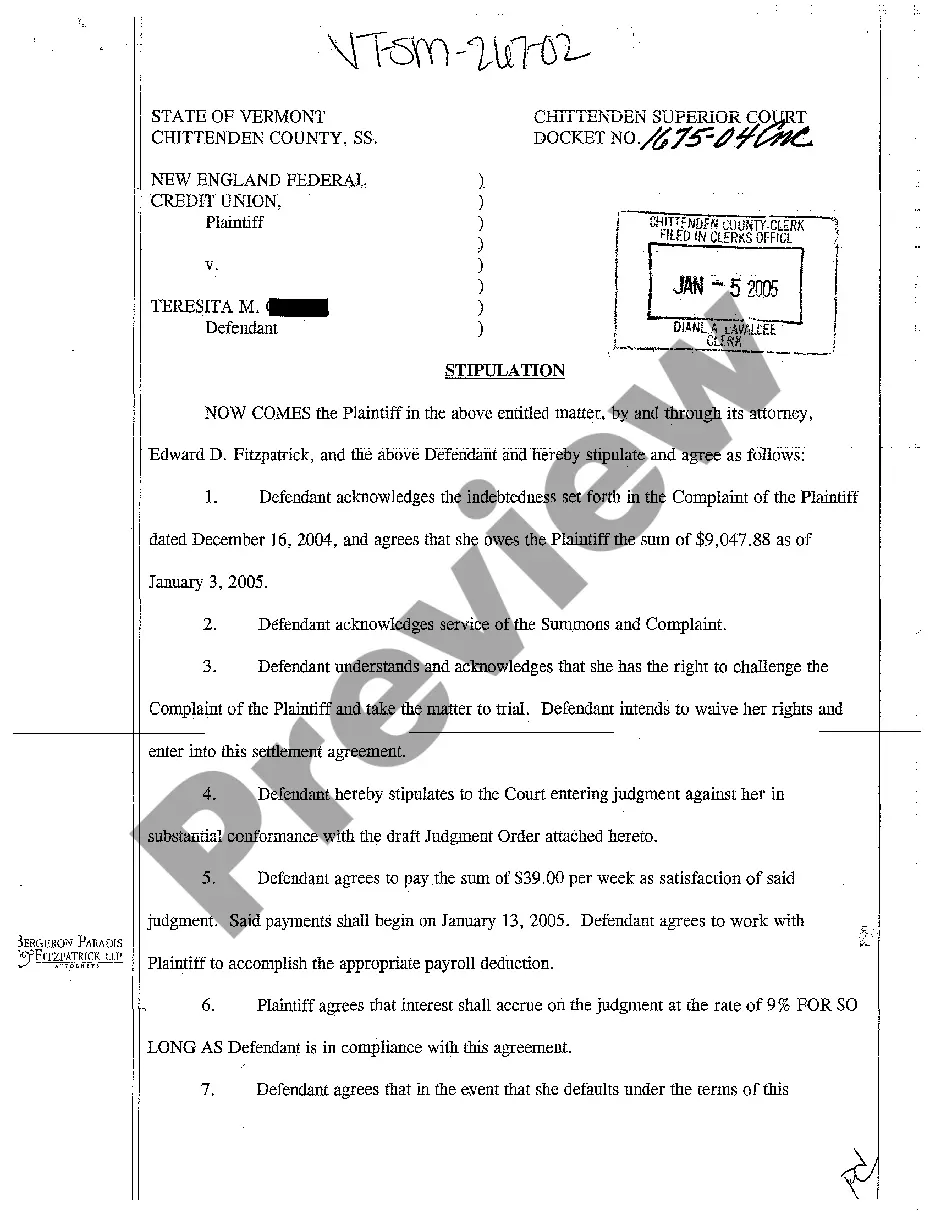
US Legal Forms provides an extensive collection of form templates, such as the Alabama COBRA Continuation Waiver Letter, designed to comply with state and federal regulations.
Once you find the appropriate form, click Purchase now.
Select the pricing plan you prefer, complete the required information to create your account, and pay for the order using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Alabama COBRA Continuation Waiver Letter template.
- If you do not have an account and want to start using US Legal Forms, follow these steps.
- Select the form you need and ensure it is for the correct area/region.
- Use the Preview button to review the form.
- Read the description to ensure you have chosen the right document.
- If the form is not what you're looking for, use the Search field to find the template that fits your needs and specifications.
Form popularity
FAQ
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.
Qualified unemployed individuals can qualify for free COBRA health insurance coverage under the latest relief bill. Unemployed Americans who lost their jobs in the last 18 months may qualify for free health insurance coverage through the Consolidated Omnibus Budget Reconciliation Act, commonly known as COBRA.
You can stop paying for your expensive premiums, or cancel COBRA continuation or coverage at any time, BUT you must remember that voluntarily quitting other health coverage or being terminated from a health plan for not paying premiums is NOT a qualifying life event.
If you want to avoid paying the COBRA cost, go with a short-term plan if you're waiting for approval on another health plan. Choose a Marketplace or independent plan for broader coverage. Choose a high-deductible plan to keep your costs low.
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
The COBRA subsidy has been extended until September 30, 2021. Currently this is the final date for subsidy assistance. There has currently been no word of extension beyond this date.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
The following do's and don'ts can help you get started to avoid common COBRA mistakes.DO count part-time employees to determine whether your plan is subject to COBRA.DO stay on top of required notices.DON'T overlook qualifying events.DON'T terminate COBRA coverage too early.DON'T forget about state law.
When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.