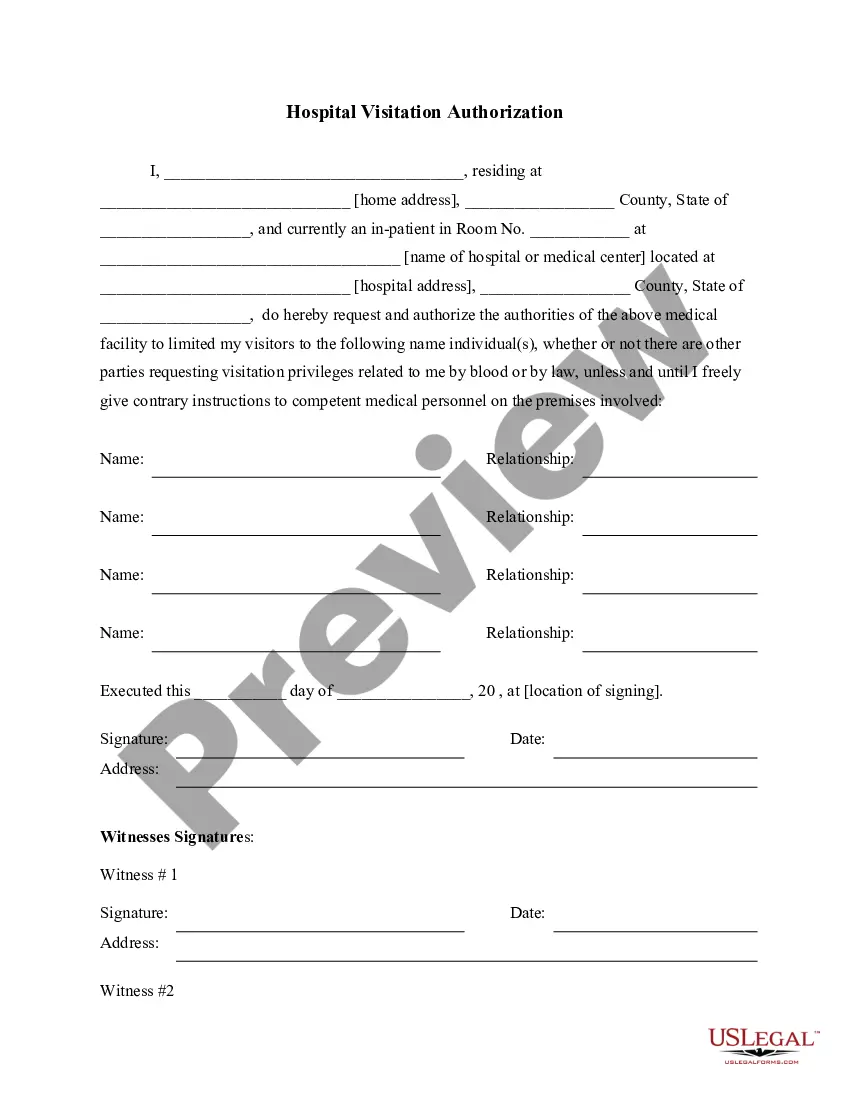
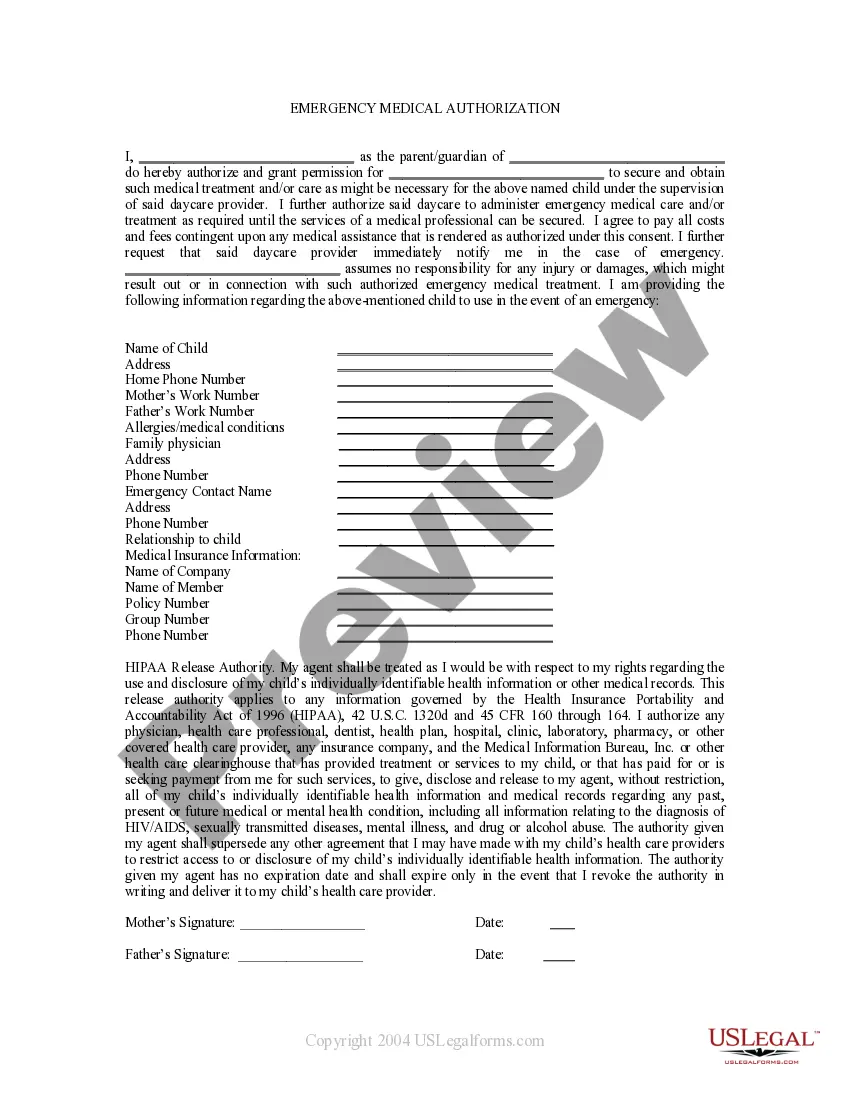
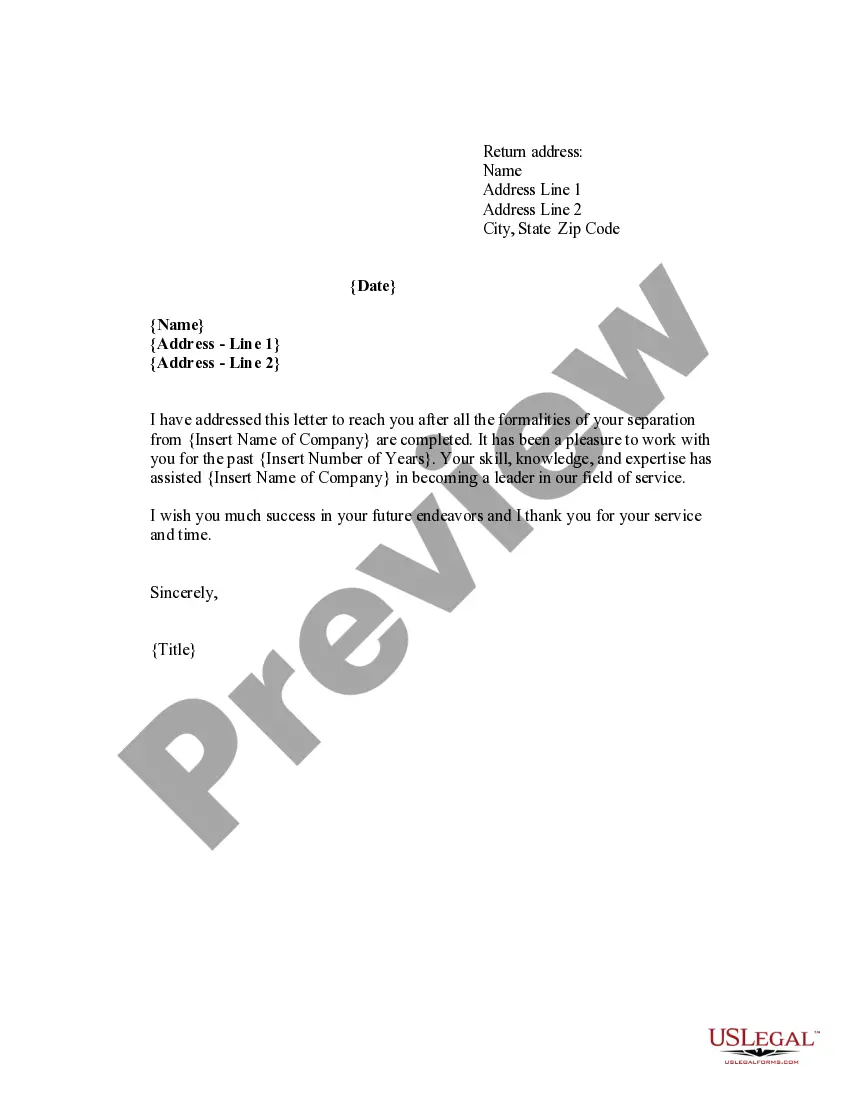
Authorization Visit Form With 2 Points
Description
How to fill out Hospital Authorization To Visit Form?
Legal document management can be overpowering, even for the most experienced specialists. When you are searching for a Authorization Visit Form With 2 Points and do not get the time to commit looking for the correct and updated version, the processes could be stress filled. A strong web form library might be a gamechanger for anyone who wants to manage these situations successfully. US Legal Forms is a market leader in web legal forms, with over 85,000 state-specific legal forms available to you anytime.
With US Legal Forms, you can:
- Gain access to state- or county-specific legal and business forms. US Legal Forms covers any needs you could have, from personal to enterprise papers, all in one location.
- Use advanced resources to finish and handle your Authorization Visit Form With 2 Points
- Gain access to a resource base of articles, guides and handbooks and materials relevant to your situation and requirements
Save time and effort looking for the papers you need, and use US Legal Forms’ advanced search and Review tool to get Authorization Visit Form With 2 Points and download it. For those who have a monthly subscription, log in to the US Legal Forms profile, search for the form, and download it. Review your My Forms tab to find out the papers you previously saved as well as to handle your folders as you can see fit.
If it is the first time with US Legal Forms, register a free account and have unlimited access to all benefits of the platform. Here are the steps to consider after accessing the form you want:
- Validate this is the correct form by previewing it and looking at its description.
- Ensure that the sample is accepted in your state or county.
- Select Buy Now once you are all set.
- Select a monthly subscription plan.
- Pick the format you want, and Download, complete, sign, print and deliver your papers.
Benefit from the US Legal Forms web library, backed with 25 years of expertise and trustworthiness. Change your daily papers managing into a smooth and intuitive process today.
Form popularity
FAQ
If your request for prior authorization has been denied, you have the right to know why. You can ask your healthcare provider's office, but you might get more detailed information by asking the medical management company that denied the request in the first place.
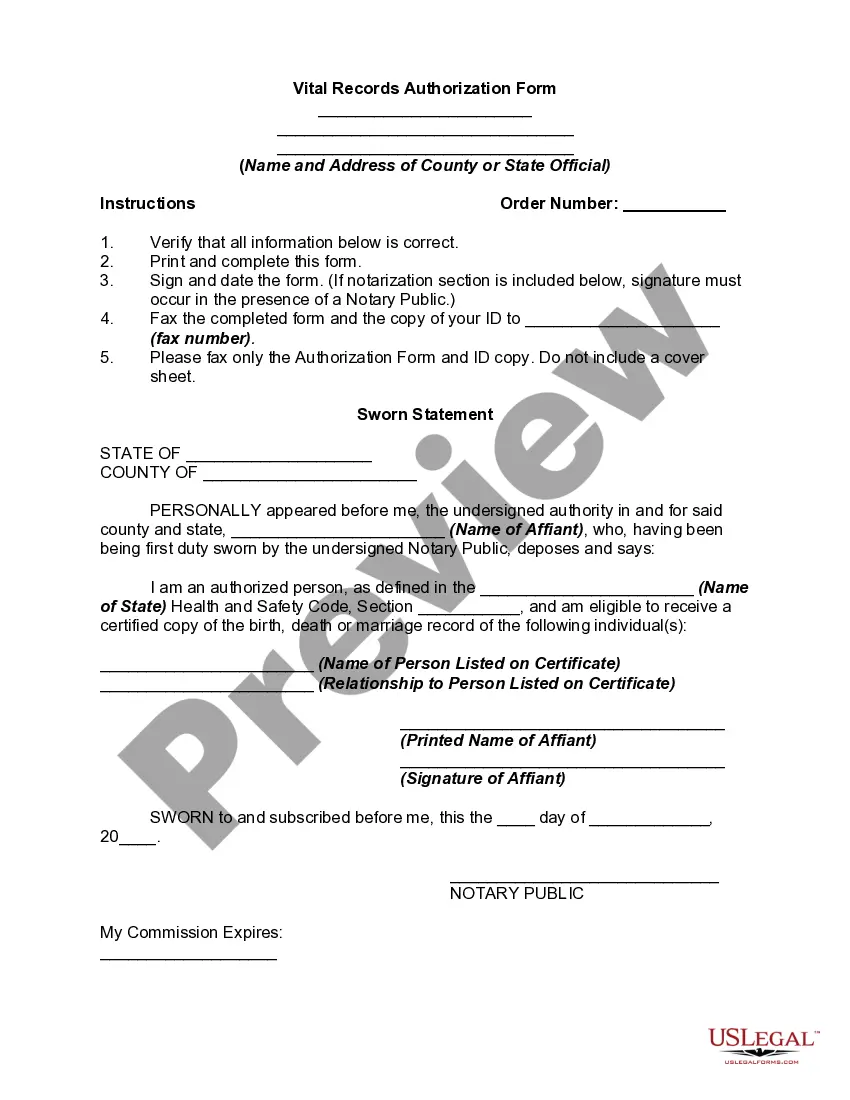
The Prior Authorization Process Flow The healthcare provider must check a health plan's policy or prescription to see if Prior Authorization is needed for the prescribed treatment. The healthcare professional must sign a Prior Authorization request form to verify the medical necessity claim.
If your prescription requires a prior authorization, the pharmacy will notify your healthcare provider. Your provider will give the necessary information to your insurance company. Your insurer will then decide whether or not to cover your medicine.
To the insurer: ? Patient name, date of birth, insurance policy number, and other relevant information. ? Physician and facility information (eg, name, provider ID number, and tax ID number) ? Relevant procedure and HCPCS codes for products/services to be provided/performed.
Tips to consider: Keep track of appeals and how long until an insurer must make a decision. Leverage a payer's peer-to-peer process. Speaking with the insurer's medical director or other physician available to speak with physicians about prior authorization issues can clear up problems much faster.