Appeal Form File For Aetna
Description
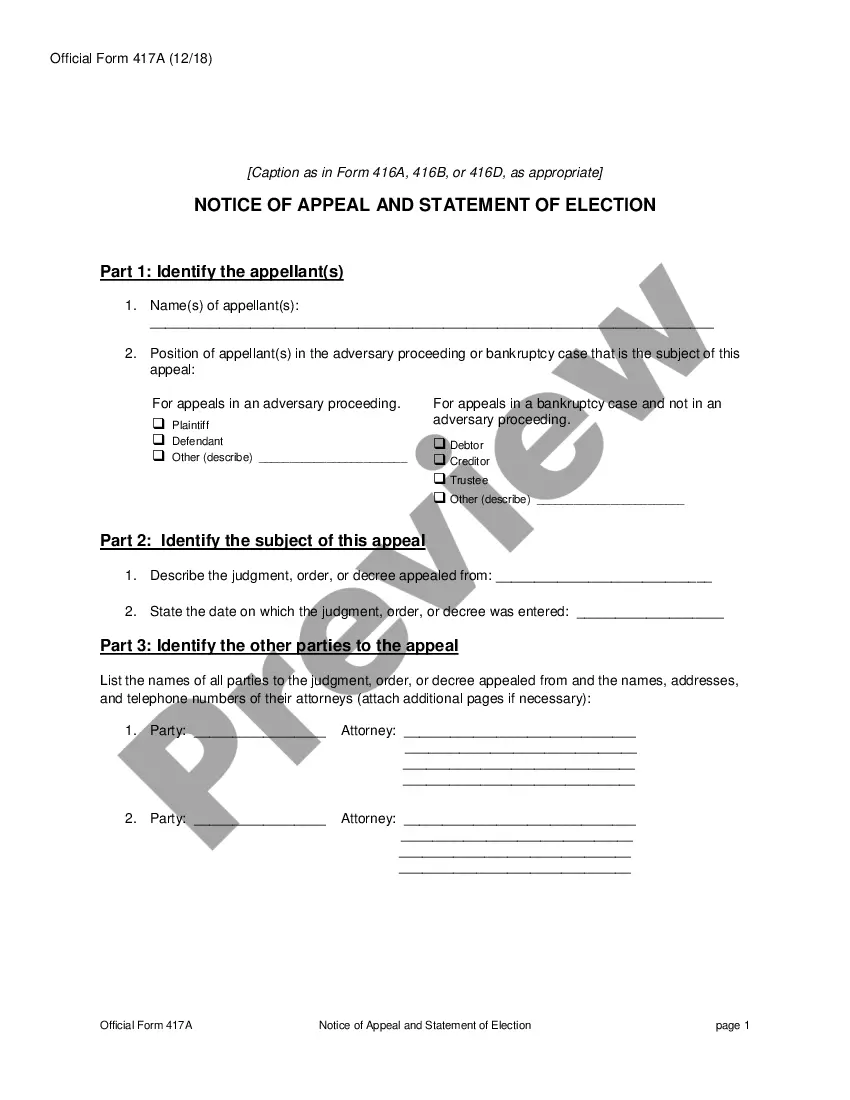
How to fill out Notice Of Appeal In A Criminal Case?
Legal document managing may be overpowering, even for knowledgeable experts. When you are interested in a Appeal Form File For Aetna and do not get the time to commit searching for the appropriate and up-to-date version, the operations might be demanding. A strong web form catalogue could be a gamechanger for everyone who wants to take care of these situations successfully. US Legal Forms is a market leader in online legal forms, with more than 85,000 state-specific legal forms accessible to you anytime.
With US Legal Forms, you are able to:
- Gain access to state- or county-specific legal and organization forms. US Legal Forms handles any needs you could have, from individual to business papers, all in one location.
- Employ innovative resources to finish and deal with your Appeal Form File For Aetna
- Gain access to a useful resource base of articles, tutorials and handbooks and resources highly relevant to your situation and requirements
Help save time and effort searching for the papers you need, and employ US Legal Forms’ advanced search and Preview feature to locate Appeal Form File For Aetna and download it. If you have a membership, log in to the US Legal Forms profile, look for the form, and download it. Take a look at My Forms tab to see the papers you previously saved and also to deal with your folders as you see fit.
If it is your first time with US Legal Forms, register a free account and get unlimited usage of all benefits of the library. Here are the steps for taking after accessing the form you want:
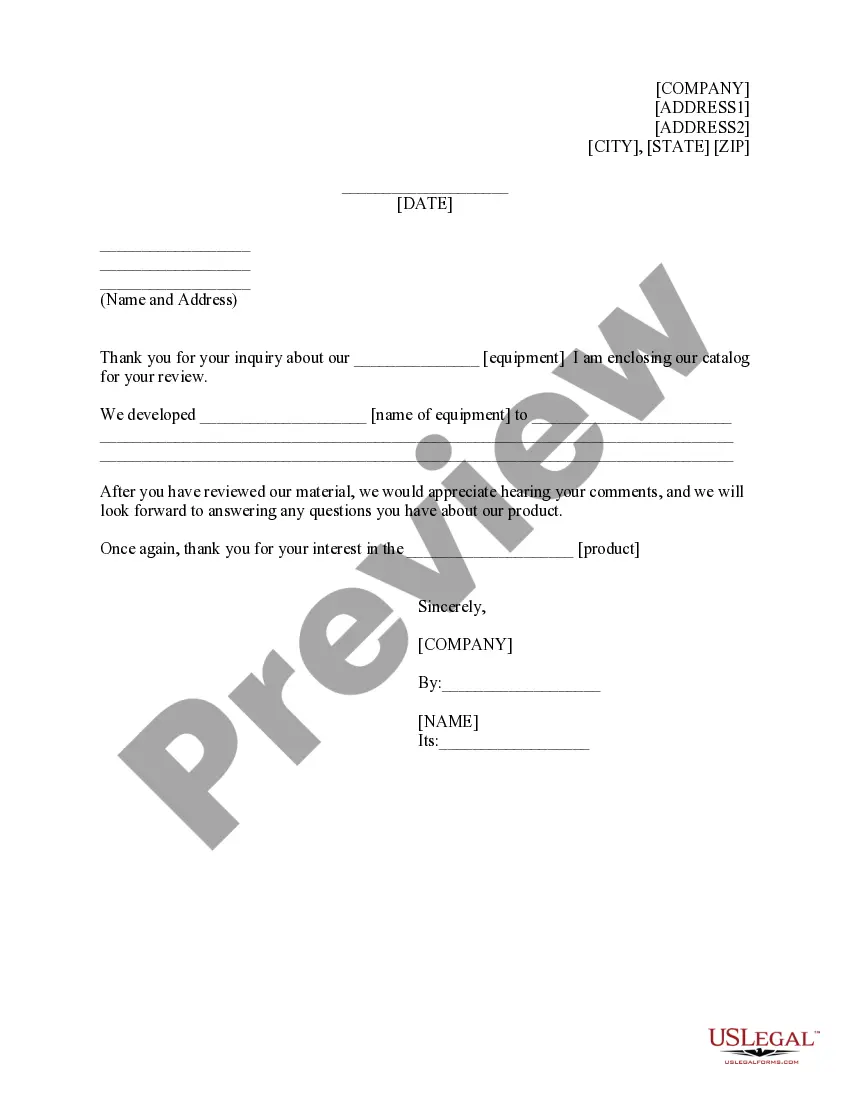
- Verify this is the right form by previewing it and reading through its information.
- Ensure that the sample is accepted in your state or county.
- Choose Buy Now once you are ready.
- Choose a monthly subscription plan.
- Find the format you want, and Download, complete, sign, print and send your papers.
Enjoy the US Legal Forms web catalogue, supported with 25 years of expertise and stability. Transform your day-to-day papers management in a easy and easy-to-use process today.
Form popularity
FAQ
If you receive a denial and are requesting an appeal, you'll ?request a medical appeal.? You can call us, fax or mail your information. Call: 1-800-245-1206 (TTY: 711), 7 days a week, 8 AM to 8 PM.
The Aetna Executive Team is rated a "D+" and led by CEO Mark Bertolini.
WOONSOCKET, R.I., April 17, 2023 ? CVS Health® (NYSE: CVS ) today announced that Brian Kane will join the company as Executive Vice President and President of Aetna®, effective September 1, 2023.
You can fax your complaint or appeal to 1-877-223-4580. You can also email us with your complaint or appeal.
TIMELY FILING APPEALS The standard timely filing period for Aetna Better Health of Texas is 95 days, measured from the claim date of service or the paid date of the primary carrier's EOP, whichever is later. Corrected claims must be received within 120 days of the first denial of the service.