Release Of Information Consent Form Psychology In California
Description
Form popularity
FAQ
Instructions for Developing an Informed Consent Document General Information. Describe the purpose(s) of this research study in lay terms. Purpose of the Study. Procedures. Risks. Benefits. Compensation, Costs and Reimbursement. Withdrawal or Termination from Study. Confidentiality.
Follow these steps to write an effective consent form. Step 1: Title and introduction. Step 2: Description of the activity. Step 3: Risks and benefits. Step 4: Confidentiality and data handling. Step 5: Voluntary participation and withdrawal. Step 6: Consent statement. Step 7: Signature and date. Step 8: Contact information.
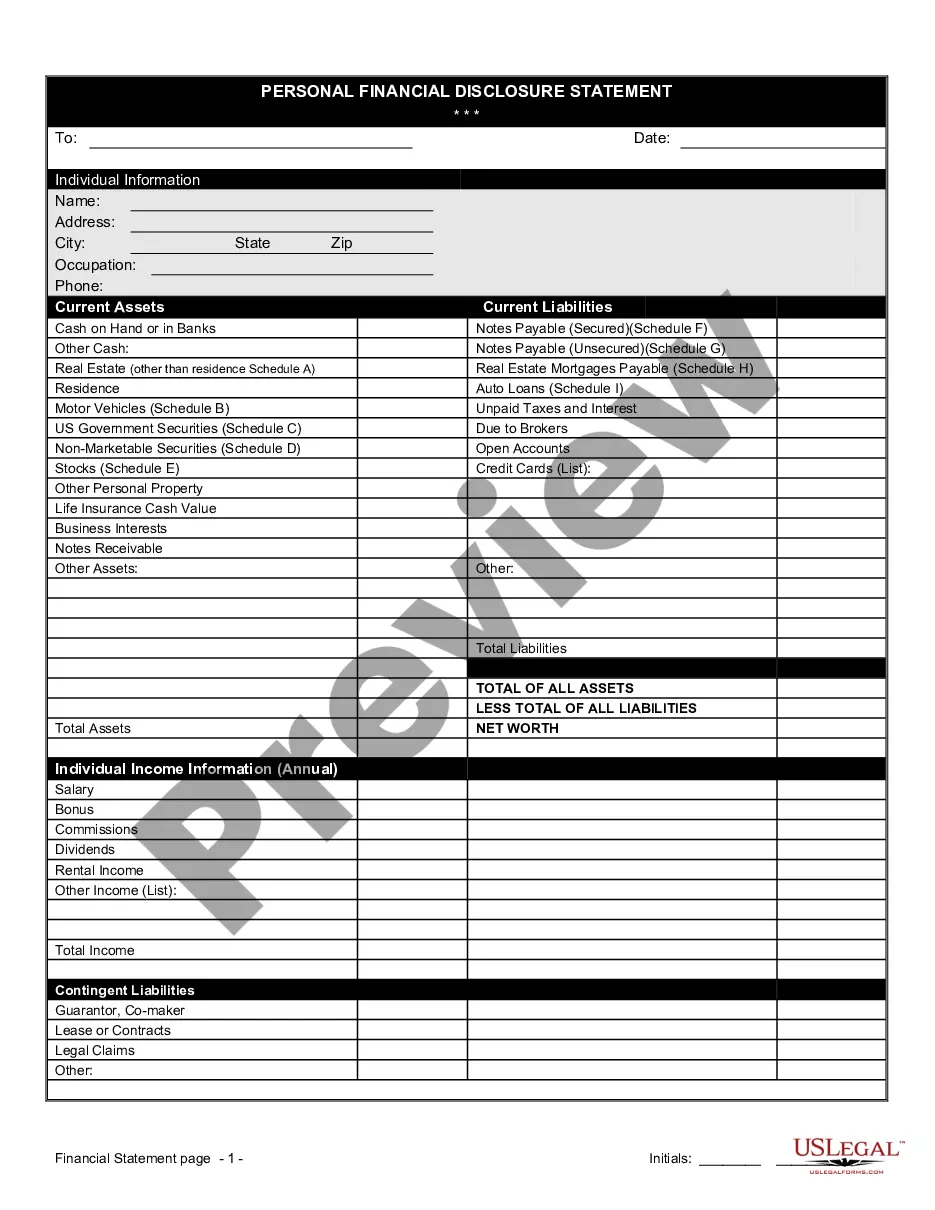
Basic Elements of Informed Consent Purpose of the Research. Description of the Research. Risks. Benefits. Alternatives to Participation.
You should focus on explaining why the question is important, summarizing the history of the question, and describing previous theories and data that are relevant to the study you will describe. Finally, you should present the hypothesis that you have tested (or will test) in your study.
It may only be met by the treating physician obtaining from his patient knowing authorization for carrying out the intended medical procedure. The physician is required to disclose whatever would be material to his patient's decision, including the nature and purpose of the procedure, and the risks and alternatives.
Please indicate with your signature on the space below that you understand your rights and agree to participate in the experiment. Your participation is solicited, yet strictly voluntary. All information will be kept confidential and your name will not be associated with any research findings.
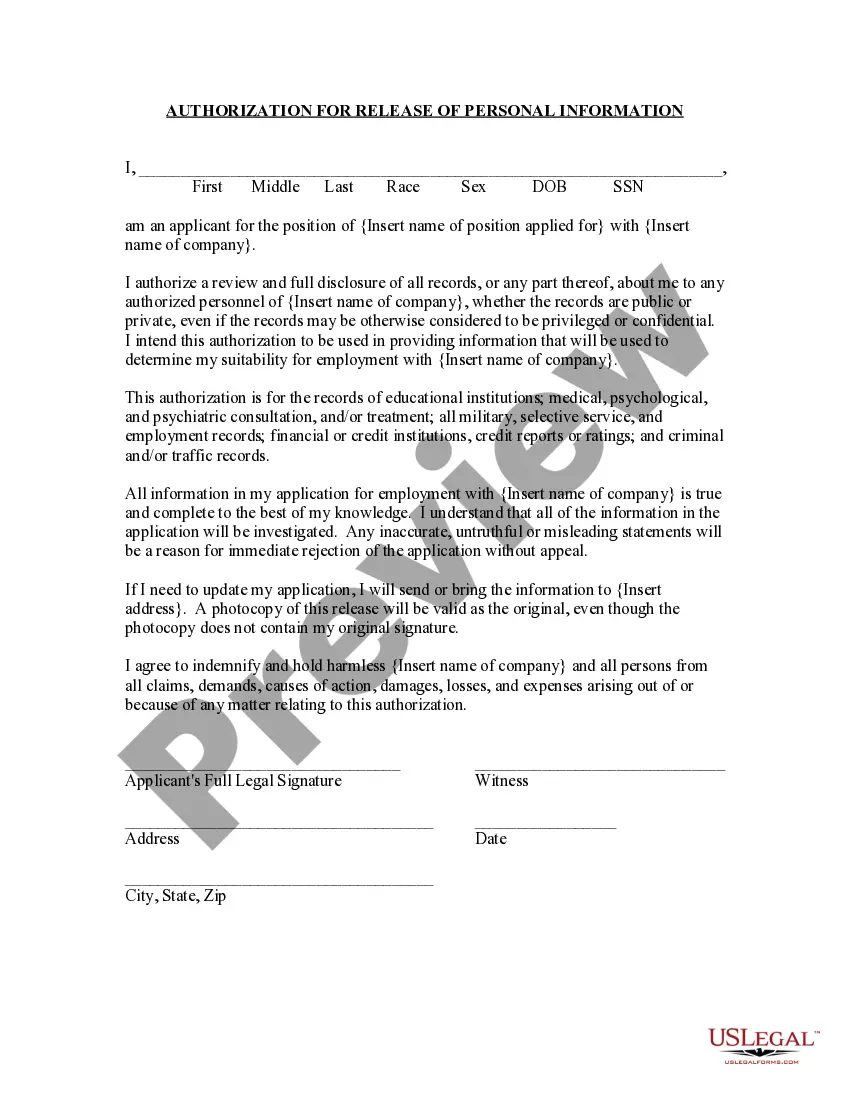
Authorization. A covered entity must obtain the individual's written authorization for any use or disclosure of protected health information that is not for treatment, payment or health care operations or otherwise permitted or required by the Privacy Rule.
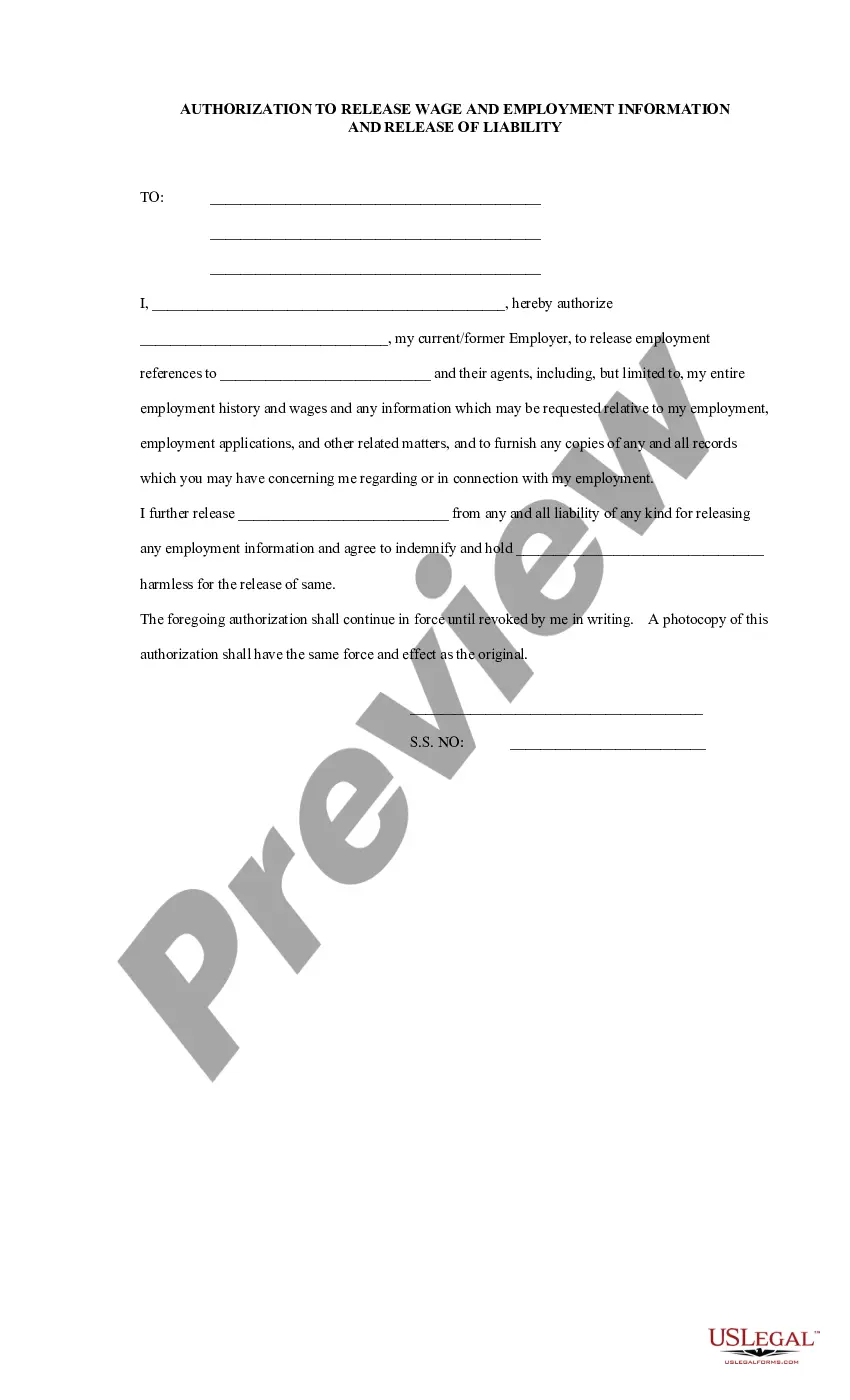
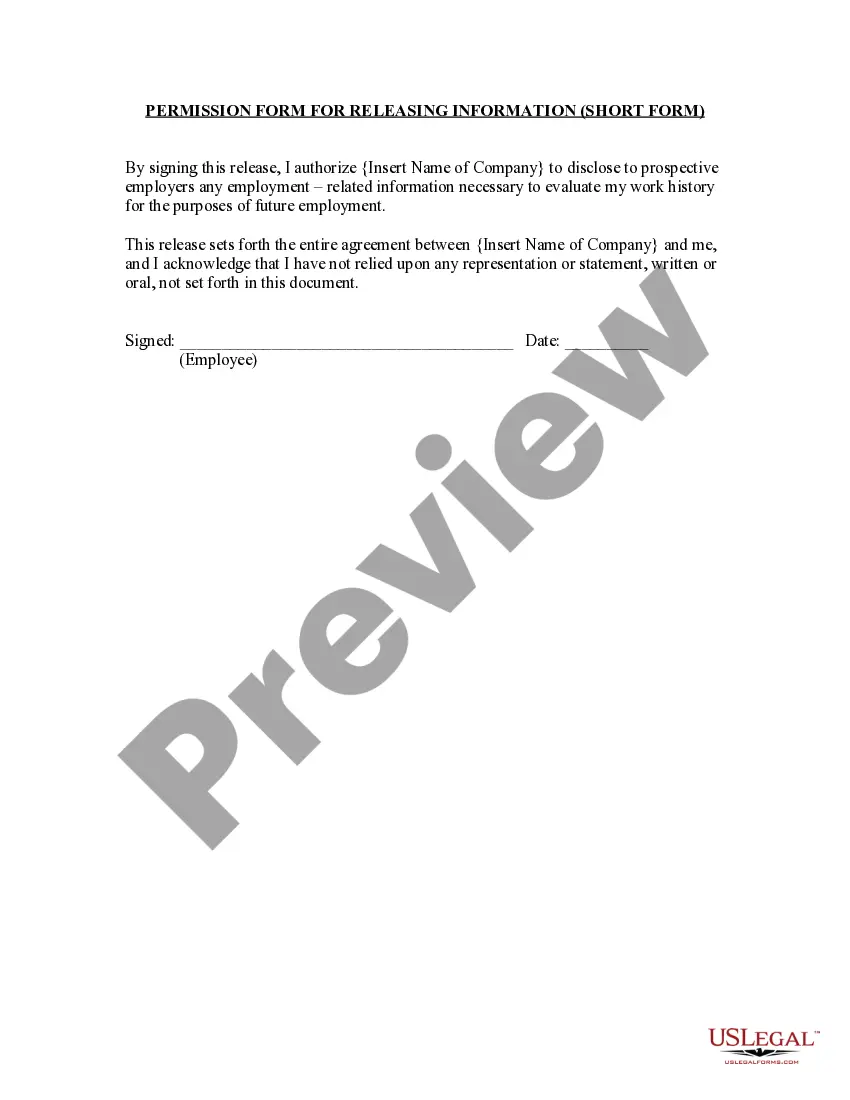
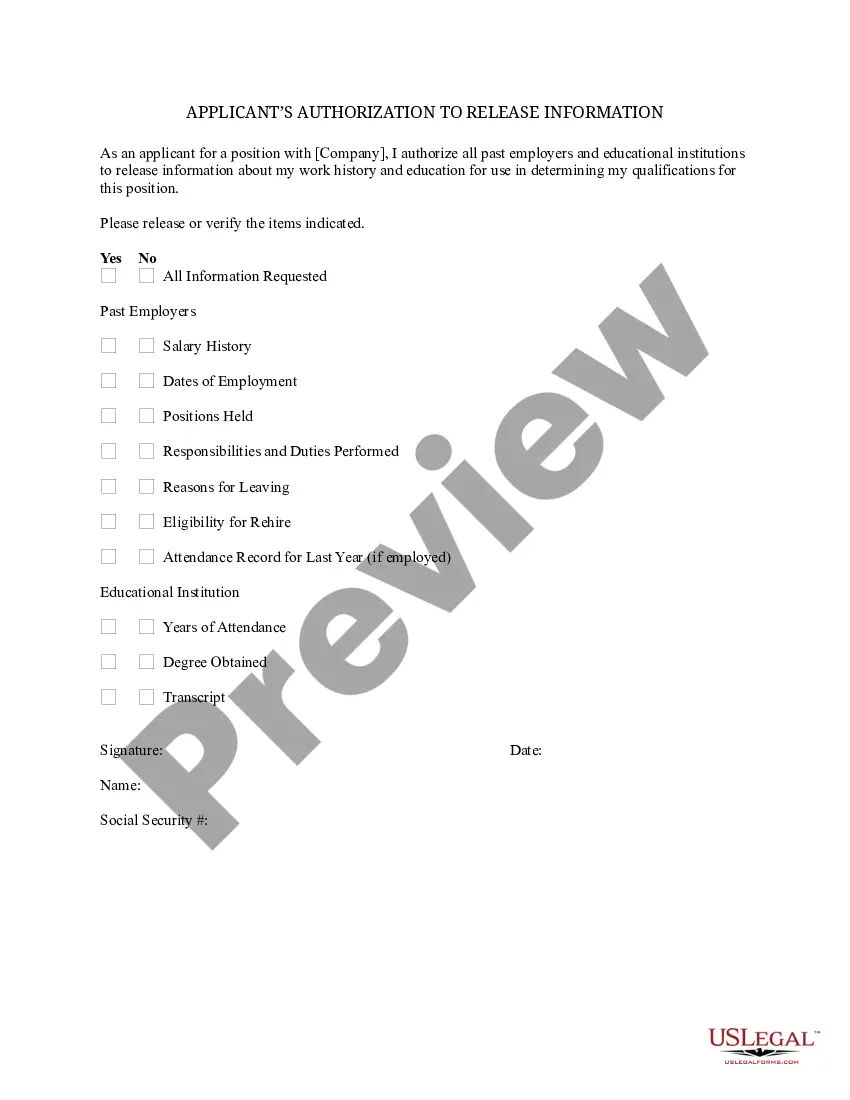
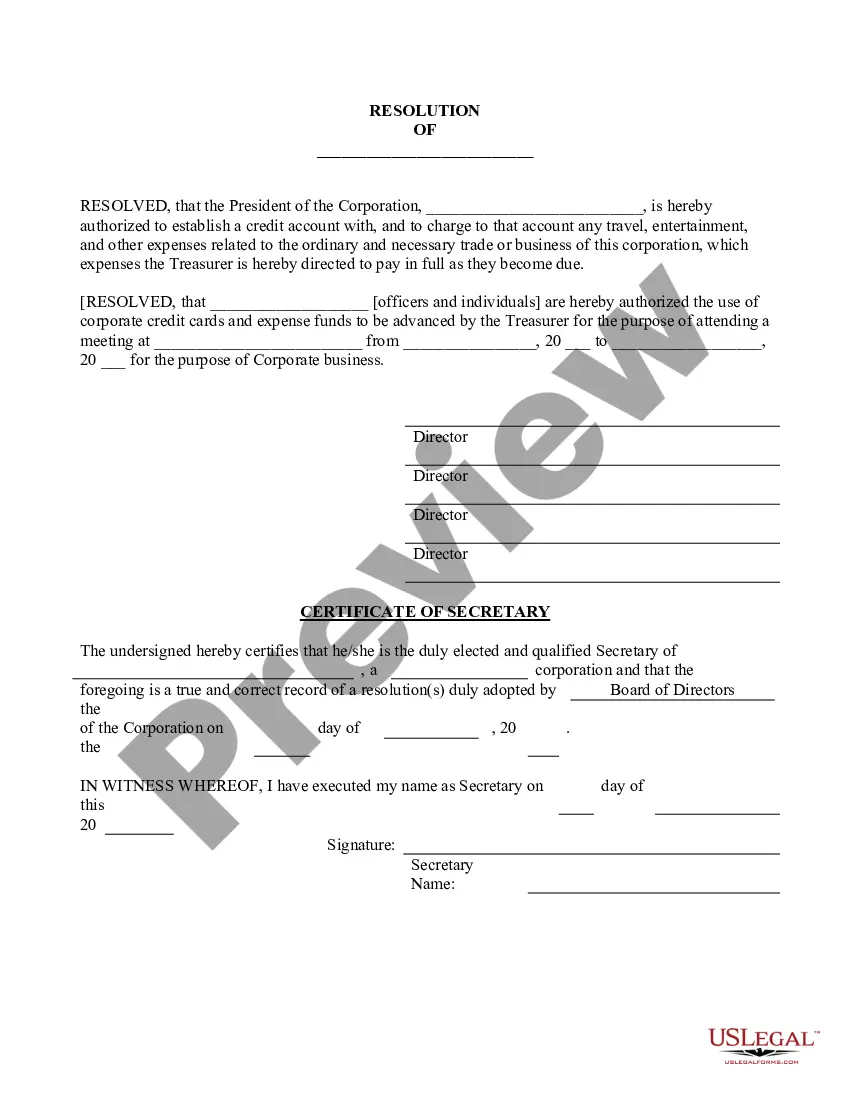
What is an Authorization Form? An authorization form is a document that is duly endorsed by an individual or organisation which grants permission to another individual or organisation to proceed with certain actions. It is often used to grant permission to carry out a specific action for a fixed period of time.
(a) Patients may authorize the release of their health care information by completing the CDCR 7385, Authorization for Release of Protected Health Information , to allow a family member or friend to request and receive an update when there is a significant change in the patient 's health care condition.
All health records of discharged patients shall be completed and filed within 30 days after discharge date and such records shall be kept for a minimum of 7 years, except for minors whose records shall be kept at least until 1 year after the minor has reached the age of 18 years, but in no case less than 7 years.