Service Agreement Provider Contract With United Healthcare In Wayne
Description
Form popularity
FAQ
Option 4: By fax Fill out a Decision Review Request: Board Appeal (Notice of Disagreement) (VA Form 10182). Fax your form and any supporting documents to 844-678-8979 .
What are the timely filing requirements? Timely filing requirements are generally 90 days from the date of service. Non-network provider and secondary claims filing limit is 6 months from date of discharge or date of service.
Timeframes for reconsiderations and appeals Dispute levelReconsideration Contacts Call: Use phone numbers above. Write: Medicare Contracted Appeals use: Medicare Provider Appeals PO Box 14835 Lexington, KY 40512 Fax: 860-900-7995 Dispute level Appeals: Medicare Non-Contracted Providers13 more rows
Yes. To streamline the credentialing and contracting process, UnitedHealthcare may also mail a contract to you within 5 business days of a request for credentialing. If my credentialing isn't approved, what happens?
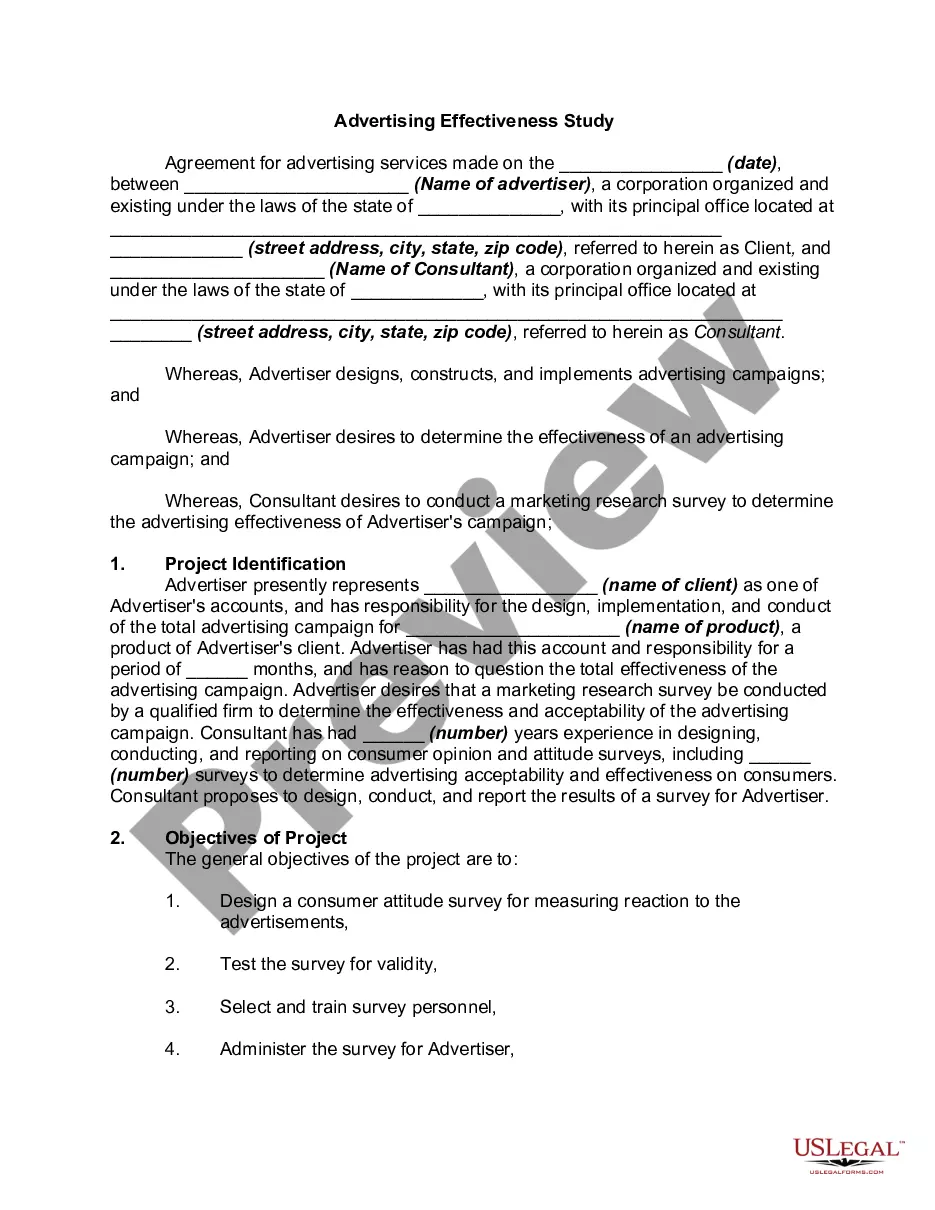
A management services agreement (MSA) is a contract that facilitates the business relationship between two business entities, most often a non-physician-owned business entity and a physician-owned medical practice.
Obtain the provider termination form: Contact United Healthcare directly or go to their website to download the provider termination form. You may need to log in to your provider account to access the form. 2. Read the instructions: Familiarize yourself with the instructions provided on the form.