Here Denied Claim For Primary Eob In Travis
Description
Form popularity
FAQ
Abbreviation for end of business: the end of the working day or the business day: by EOB Could you let me have your projections by EOB Friday? Synonyms. COB.
Explanation of Benefits (EOB) Lookup.
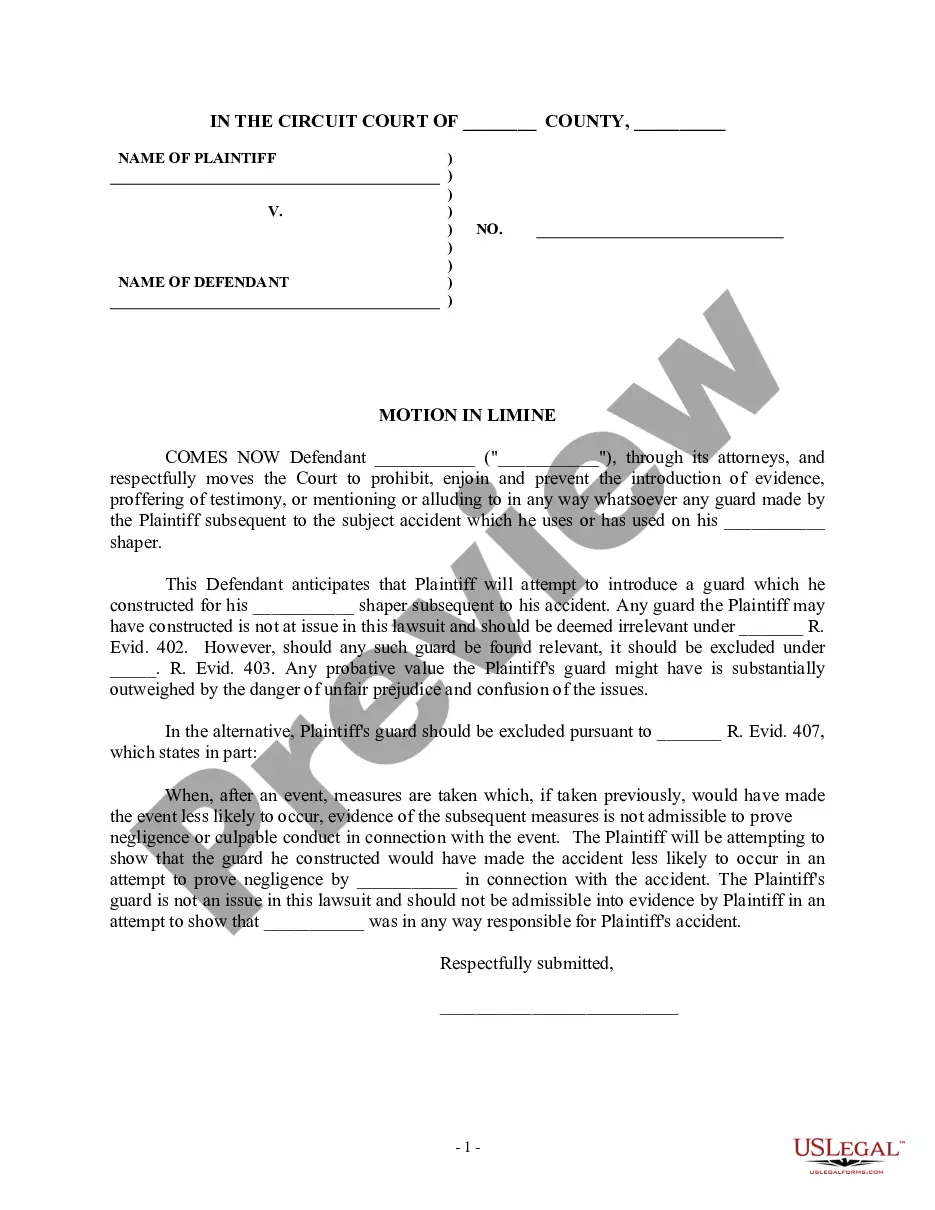
If the notification is not clear, call the carrier for more information. In addition to eliciting a stated reason for denying a claim, you may find out that the claim was adjudicated incorrectly because of an administrative error on the part of the payer.
You can ask your doctor to resubmit the claim and correct the error. If your claim was denied for another reason, let your doctor know that you're appealing a claim. You can ask your doctor to write a letter explaining that the service was medically necessary, or provide other supporting documents.
If an insurance company denies a request or claim for medical treatment, insureds have the right to appeal to the company and also to then ask the Department of Insurance to review the denial. These actions often succeed in obtaining needed medical treatment, so a denial by an insurer is not the final word.
Abbreviation for end of business: the end of the working day or the business day: by EOB Could you let me have your projections by EOB Friday?
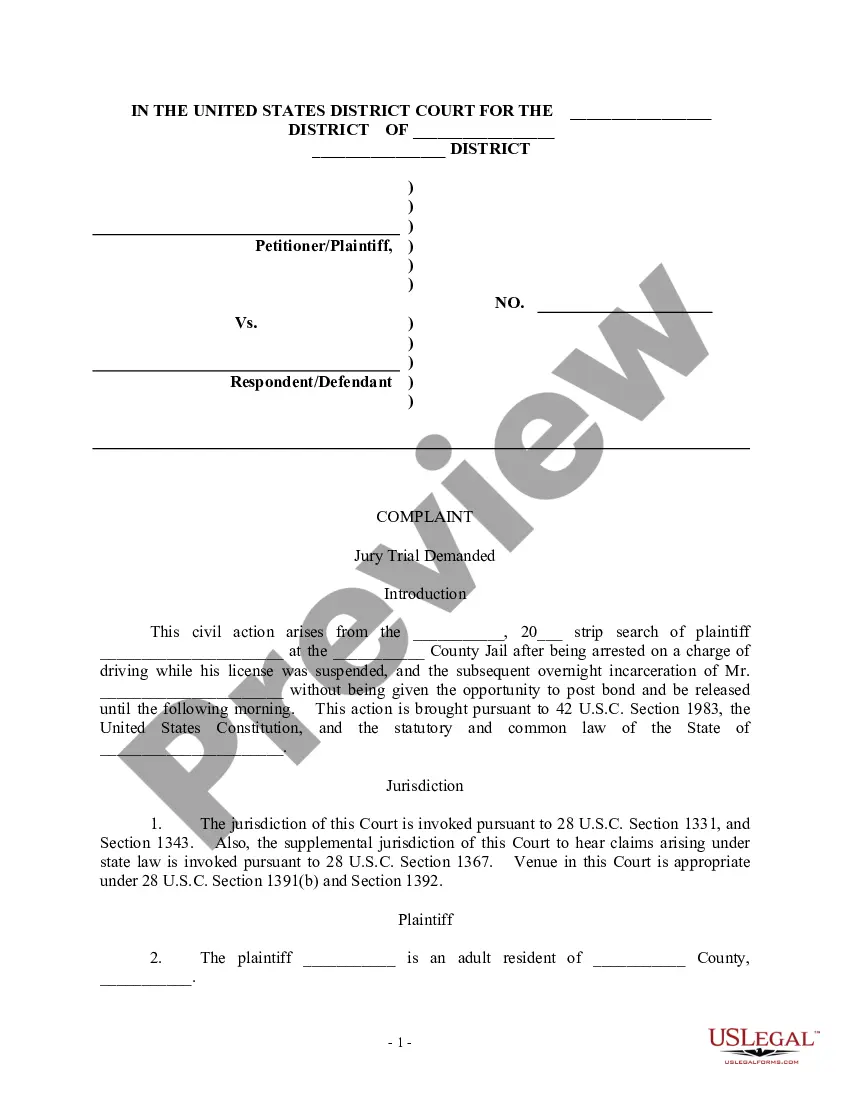
Each time your insurer pays for a service you use, they send you an Explanation of Benefits (EOB). The EOB is your insurance company's written explanation for that claim, showing the name of the provider that covered the service and date(s) of service.
You can start the appeal process by calling your insurance provider. Ask for more details about the denial and review your appeal options. Your insurance agent can walk you through the appeals process to help get you started.
Claim Denials are claims that have been received and processed by the insurance carrier and have been deemed unpayable for a variety of reasons. These claim denials typically contain an error that was flagged after processing.
EOB stands for “end of business,” a phrase that has the same meaning as “close of business.” In other words, the time when a company closes its doors at the end of the day.