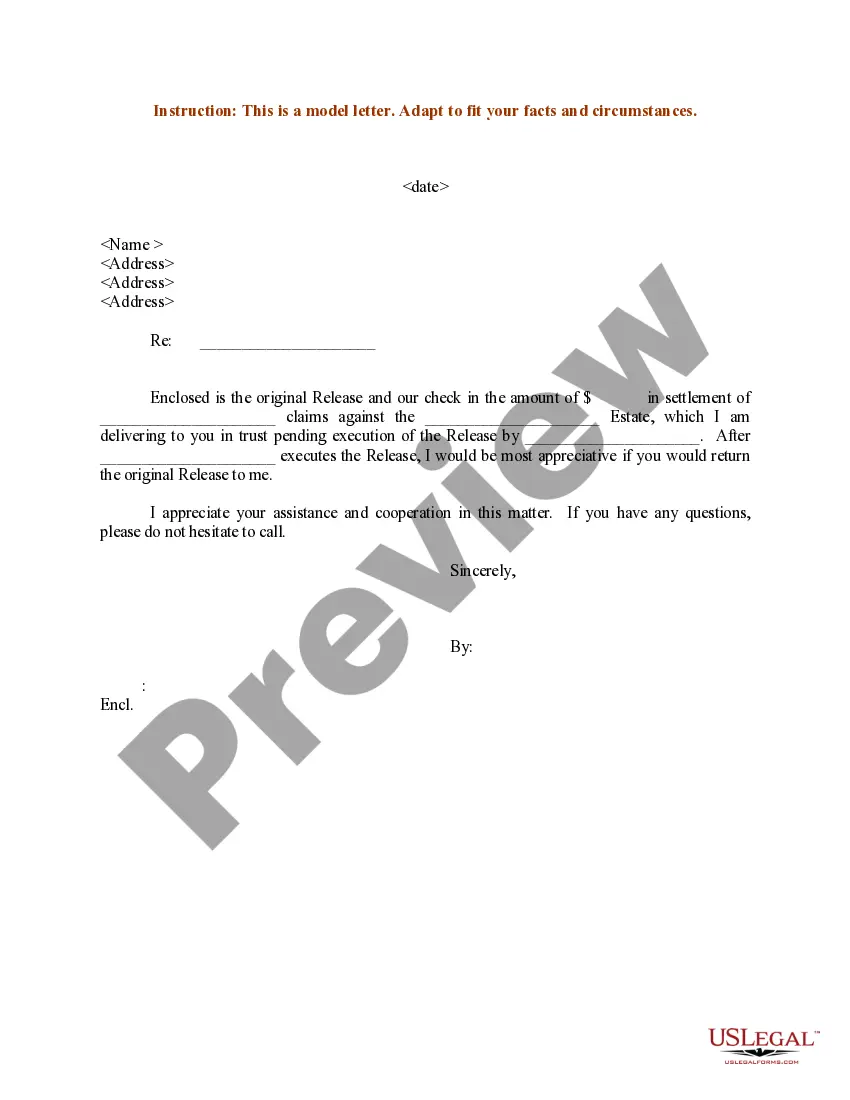
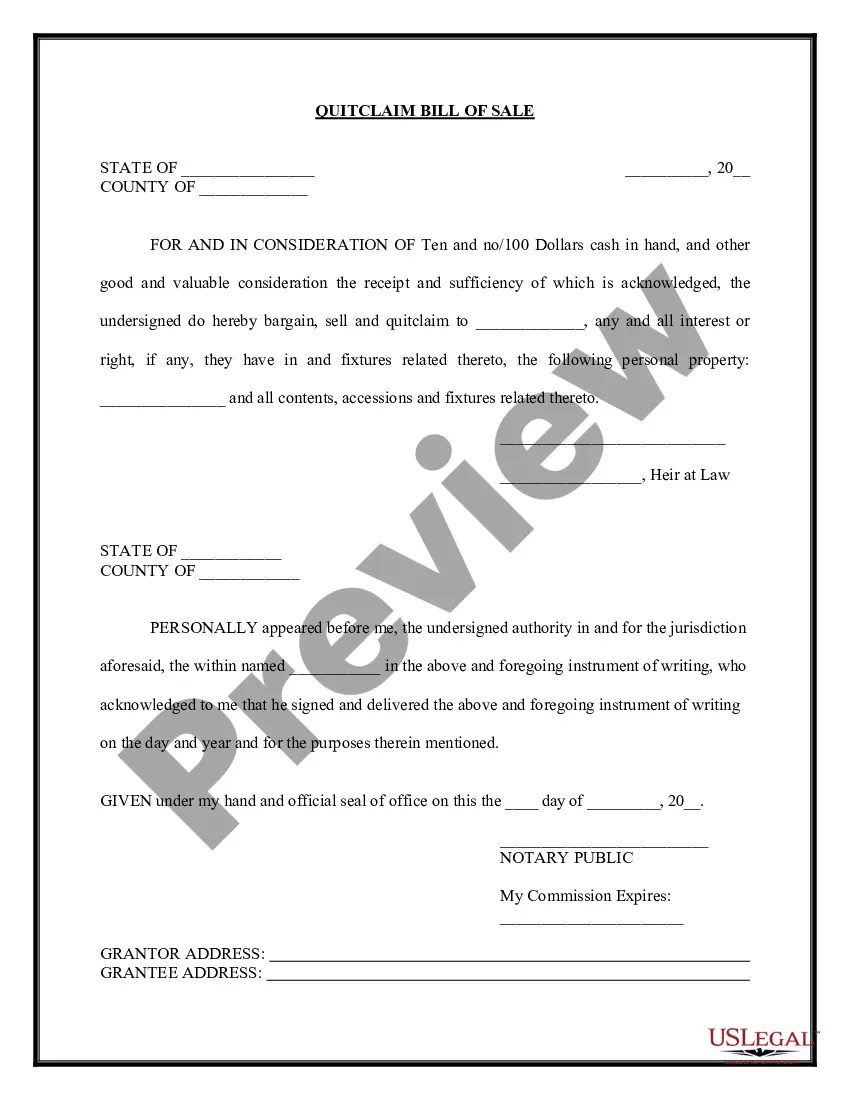
The parties may agree to a different performance. This is called an accord. When the accord is performed, this is called an accord and satisfaction. The original obligation is discharged. In order for there to be an accord and satisfaction, there must be a bona fide dispute; an agreement to settle the dispute; and the performance of the agreement. An example would be settlement of a lawsuit for breach of contract. The parties might settle for less than the amount called for under the contract.
Anthem Claim Dispute Form With Claim Number In Travis
Description
Form popularity
FAQ
Effective Date: January 1, 2024 Plan NameSingle (1)Two-Party (2) Anthem Blue Cross Del Norte EPO $1,240.19 $2,480.37 Anthem Blue Cross Select HMO $944.08 $1,888.16 Anthem Blue Cross Traditional HMO $1,221.90 $2,443.80 Blue Shield Access+ EPO $910.34 $1,820.6815 more rows •
For help, call us at the number listed on your ID card or 1-866-346-7198.
Customer Care Centers Call 888-831-2246 Option 4 and ask to speak with Dr.
With the PPO, you can use any of the BCBS providers in all 50 states. They may not be directly contracted with the BS of CA, but as long as they participate with the BCBS in the state you see a provider in, they will file claims with that plan. Benefits would be covered at the in-network rates given that's the case.
When complete, please mail to: Attn: Grievance and Appeals Department, Anthem Blue Cross, P.O. Box 60007, Los Angeles, CA 90060-0007. For claim disputes, please use the Provider Dispute Resolution form. This information is part of the permanent record. Write clearly and legibly.
Anthem follows the standard of: • 90 days for participating providers and facilities.
Anthem Blue Cross is the trade name of In California: Blue Cross of California, Anthem Blue Cross Partnership Plan, Anthem BC Health Insurance Company and Anthem Blue Cross Life and Health Insurance Company are independent licensees of the Blue Cross Association.
To use the Appeals application, the Availity administrator must assign the Claim Status role for the user. The Disputes and Appeals functionality will support Appeals, Reconsiderations and Rework requests for providers. The Disputes and Appeals functionality is accessible from the Claim Status transaction.
Common Reasons Anthem Gives for Insurance Denials Reasons for Anthem insurance claims denials include: The filing deadline has expired. The insured mad a late payment to COBRA. The medical device or treatment sought is not medically necessary.