Anthem Claim Dispute Form With Provider In Santa Clara
Description
Form popularity
FAQ
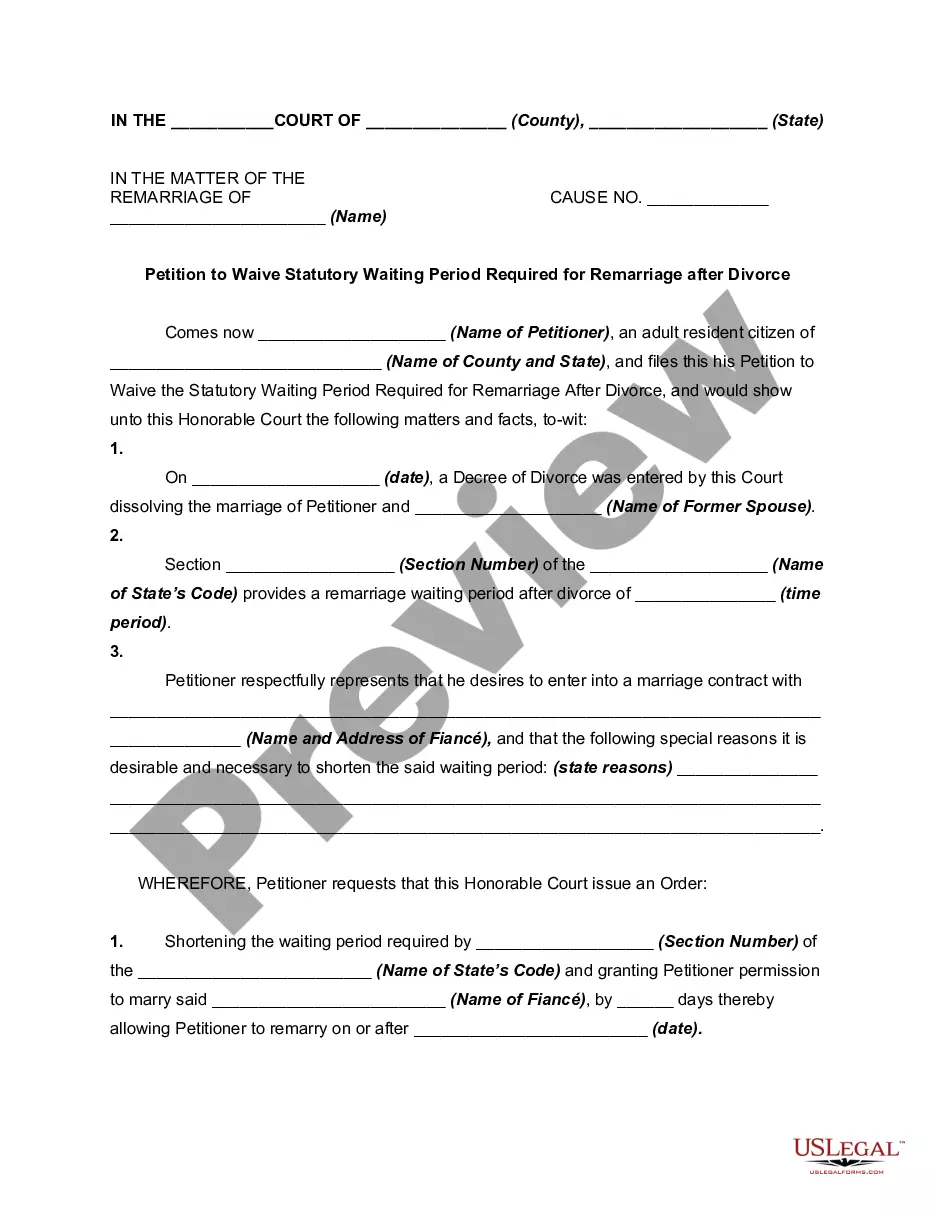
Provider Dispute Resolution Review Process Provider submits written dispute to Anthem Blue Cross at P.O. Box 60007, Los Angeles, CA 90060-0007.
If a dispute involves a lack of a decision, it must be submitted within 365 days, or the time specified in the provider's contract, whichever is greater, after the time for contesting or denying a claim has expired.
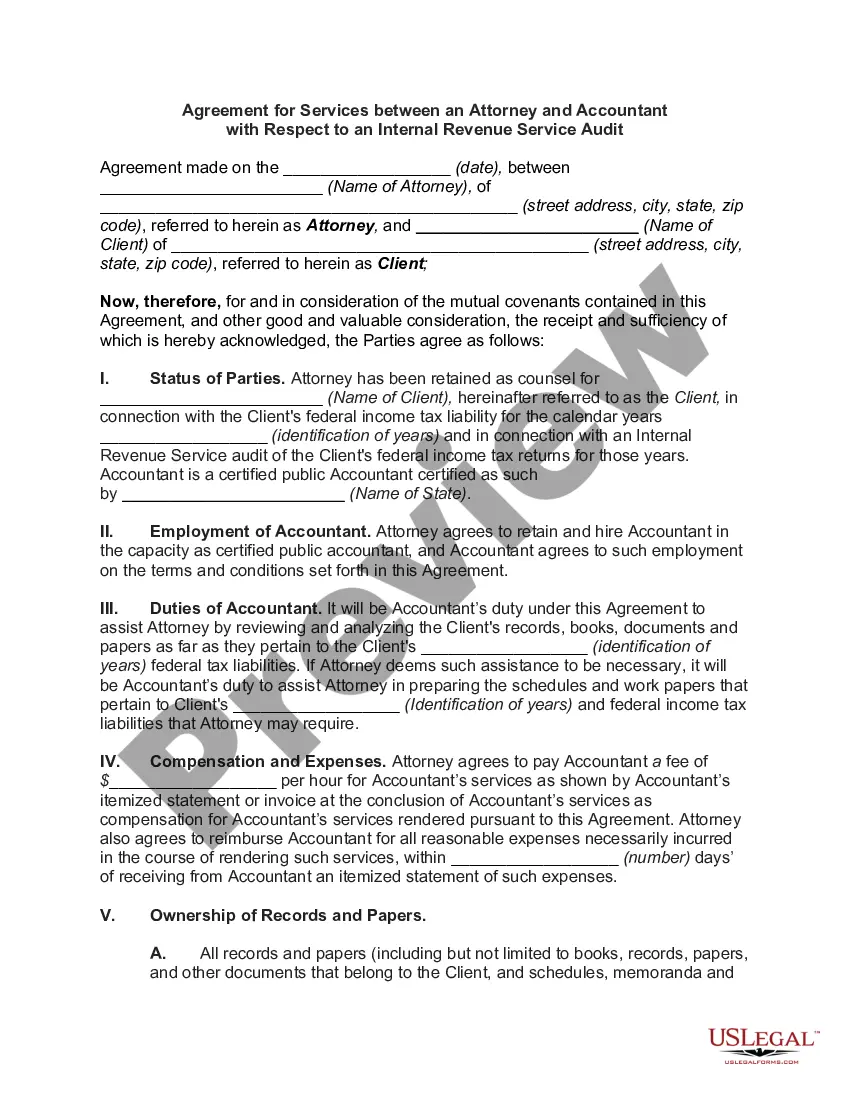
In 2019, Anthem's denial rate was 35%. The average rate of denials in the industry currently hovers around 17%. Anthem has been repeatedly fined millions of dollars for reneging on their financial responsibility to patients and providers in variously creative ways, with denials figuring largely in this pattern.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
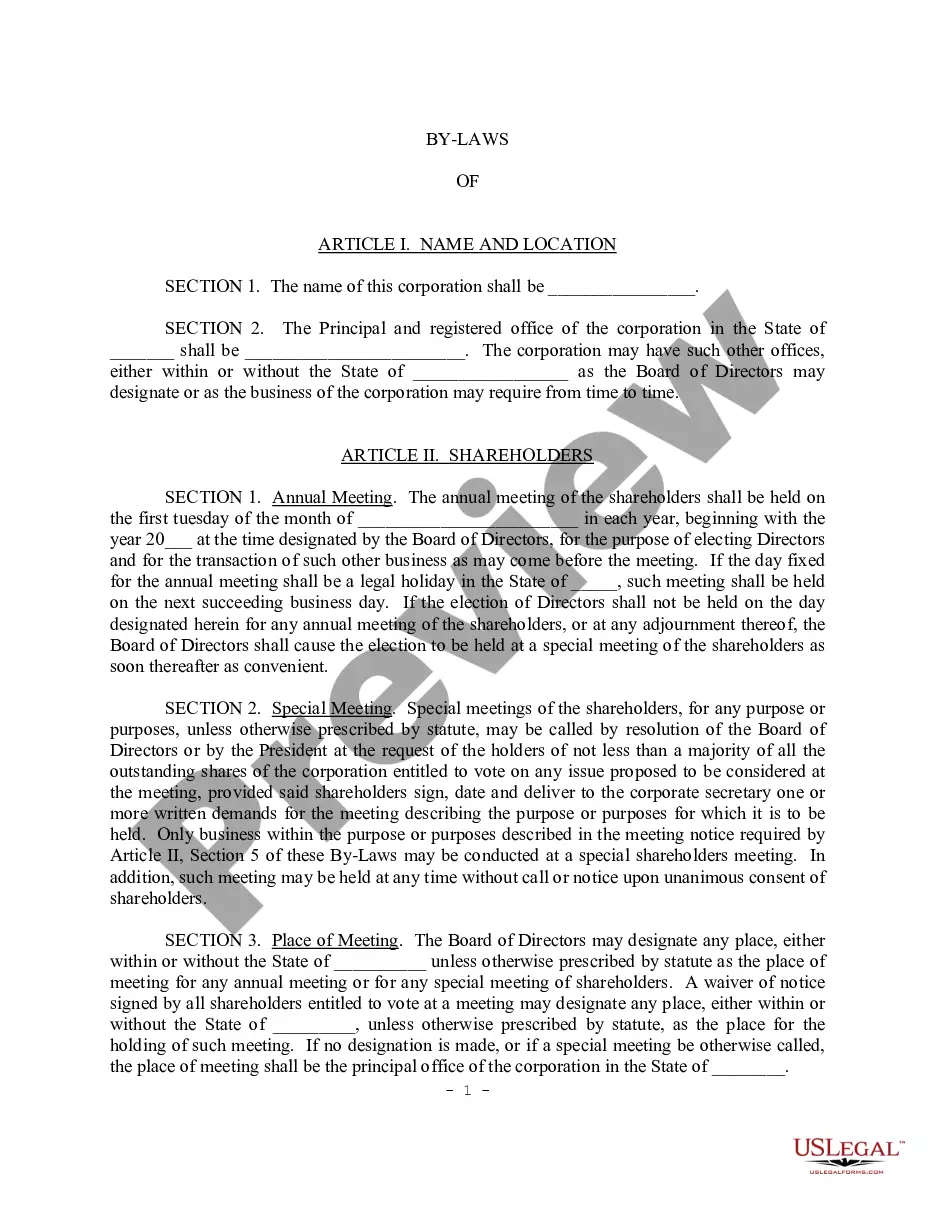
Anthem Blue Cross is the trade name of Blue Cross of California. Anthem Blue Cross and Blue Cross of California Partnership Plan, Inc. are independent licensees of the Blue Cross Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc.
How to Appeal a Claim Step 1: Contact Us. Call the Member Services phone number on your member ID card. Step 2: Submit A Written Appeal. CareFirst BlueChoice must receive your written appeal within 180 days of the date of notification of the denial of benefits or services. Step 3: Appeal Decisions.
You have the right to voice your dissatisfaction with any aspect of Anthem' services for investigation and resolution by: Writing your grievance. Completing the online GRIEVANCE FORM. Calling our Customer Care Center at 800-407-4627 (TTY 711) Monday to Friday, 7 a.m. to 7 p.m. Pacific time.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.
Blue Shield sold Care1st Arizona to WellCare in 2017. Care1st California was renamed Blue Shield of California Promise Health Plan in 2019.
With the PPO, you can use any of the BCBS providers in all 50 states. They may not be directly contracted with the BS of CA, but as long as they participate with the BCBS in the state you see a provider in, they will file claims with that plan. Benefits would be covered at the in-network rates given that's the case.