Denied Claim Agreement For Medicare In Ohio
Description
Form popularity
FAQ
To submit this form, choose your preferred method: online at fepblue/mra, via fax at 877-353-9236, or by mailing it to P.O. Box 14053, Lexington, KY 40512. Ensure that you include all required documents that verify your Medicare Part B premium payment.
What is the best way to win a Medicare appeal? Make sure all notices from Medicare or the Medicare Advantage plan are fully read and understood. Include a letter from the beneficiary's doctor in support of the appeal. Make sure to meet appeal deadlines. Keep a copy of all documents sent and received during the process.
Timeframes for reconsiderations and appeals Dispute levelReconsideration Contacts Call: Use phone numbers above. Write: Medicare Contracted Appeals use: Medicare Provider Appeals PO Box 14835 Lexington, KY 40512 Fax: 860-900-7995 Dispute level Appeals: Medicare Non-Contracted Providers13 more rows
1. Fill out a “Medicare Reconsideration Request” form (CMS Form number 20033), which is included with the “Medicare Redetermination Notice.” You can also get a copy by visiting CMS/cmsforms/downloads/cms20033.pdf, or calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
1-800-MEDICARE (1-800-633-4227) For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.
One redetermination form can be submitted for multiple claims only for denials by the Unified Program Integrity Contractor or Medical Review probe reviews. Fax request to 1-888-541-3829.
Call us at 1-800-MEDICARE (1-800-633-4227).
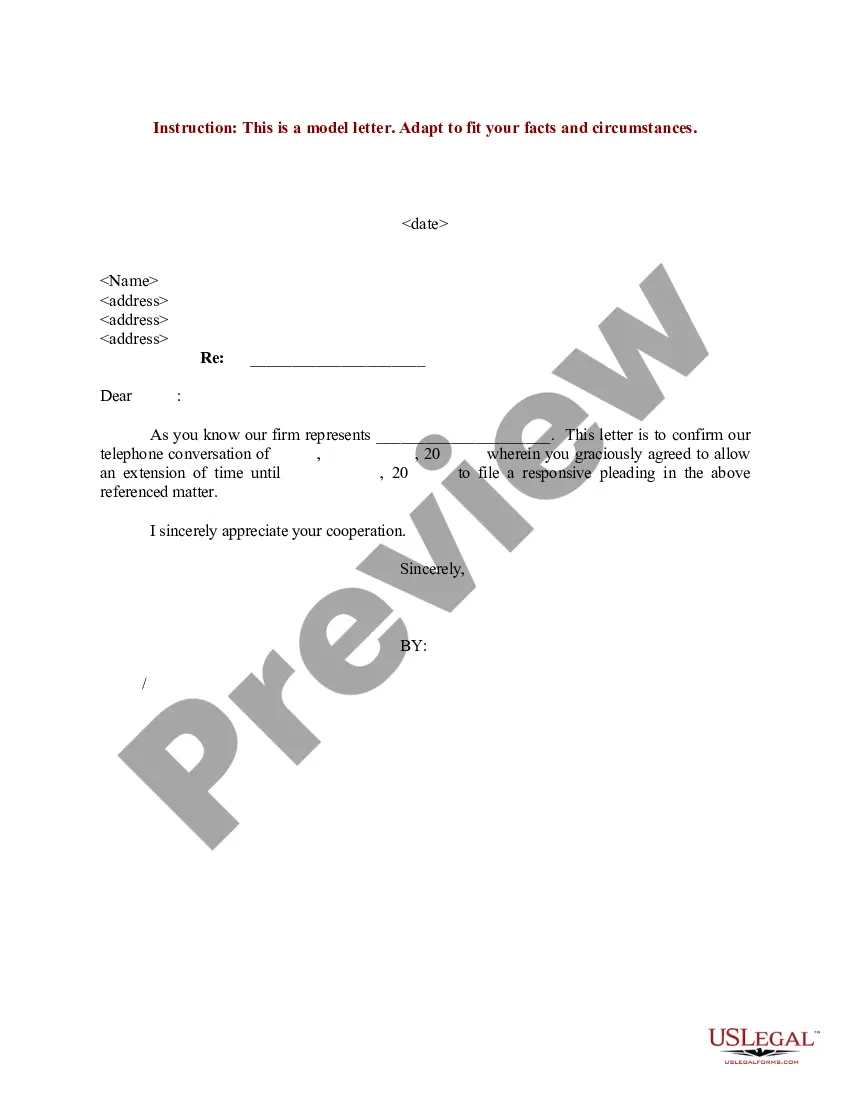
Any letter written to appeal a denial should include a response to the specific reasons given for the denial. Before writing a letter you must request the reasons for denial in writing, if you have not already received this and also request copies of any plan guidelines that were used in support of the denial.
To ask for a hearing, call or write your local agency or write to the Ohio Department of Job and Family Services, Bureau of State Hearings, PO Box 182825, Columbus, Ohio 43218-2825. If you receive a notice denying, reducing or stopping your assistance or services, you will receive a state hearing request form.