Anthem Claim Dispute Form With 2 Points In New York
Description
Form popularity
FAQ
Services provided by Anthem HealthChoice HMO, Inc., and/or Anthem HealthChoice Assurance, Inc., Independent licensees of the Blue Cross Blue Shield Association, an association of independent Blue Cross and Blue Shield plans, serving residents and businesses in the 28 eastern and southeastern counties of New York State.
Yes. We will retain the Blue Cross and Blue Shield and Blue Cross in our name. Anthem Blue Cross and Blue Shield and Anthem Blue Cross are our local health insurance companies in our 14 Blue-licensed markets and will continue to be our local health plan brands in those states, which now includes New York.
Insurance: Anthem BCBS (formerly known as Empire Blue Cross Blue Shield BCBS) - NYC Health + Hospitals.
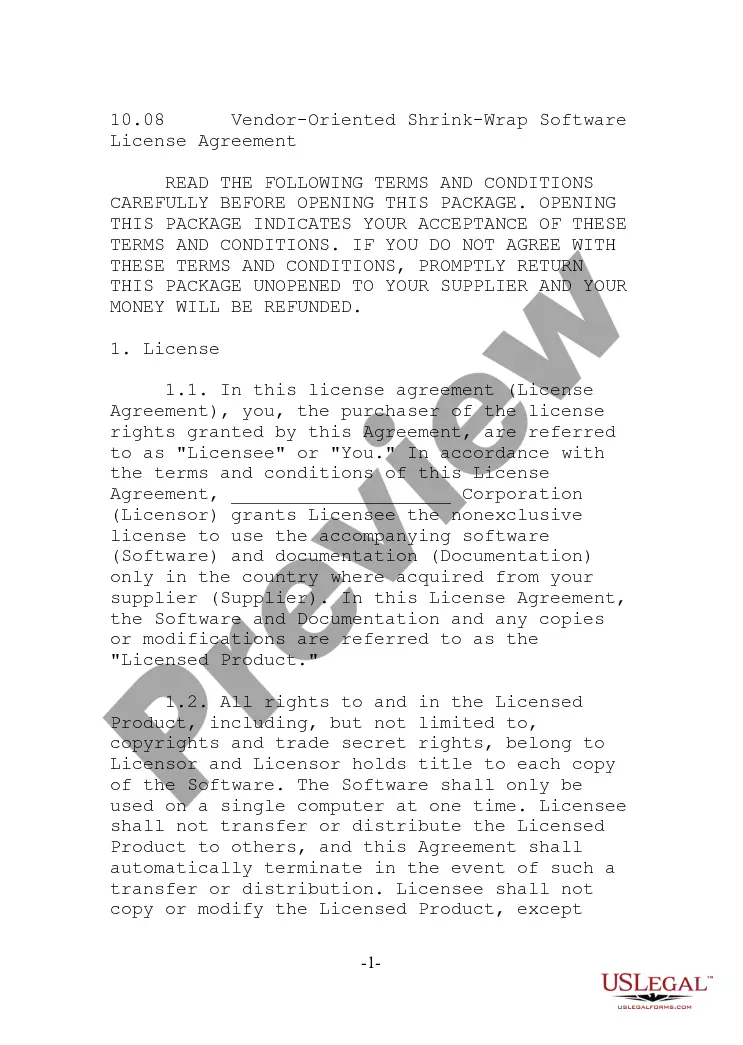
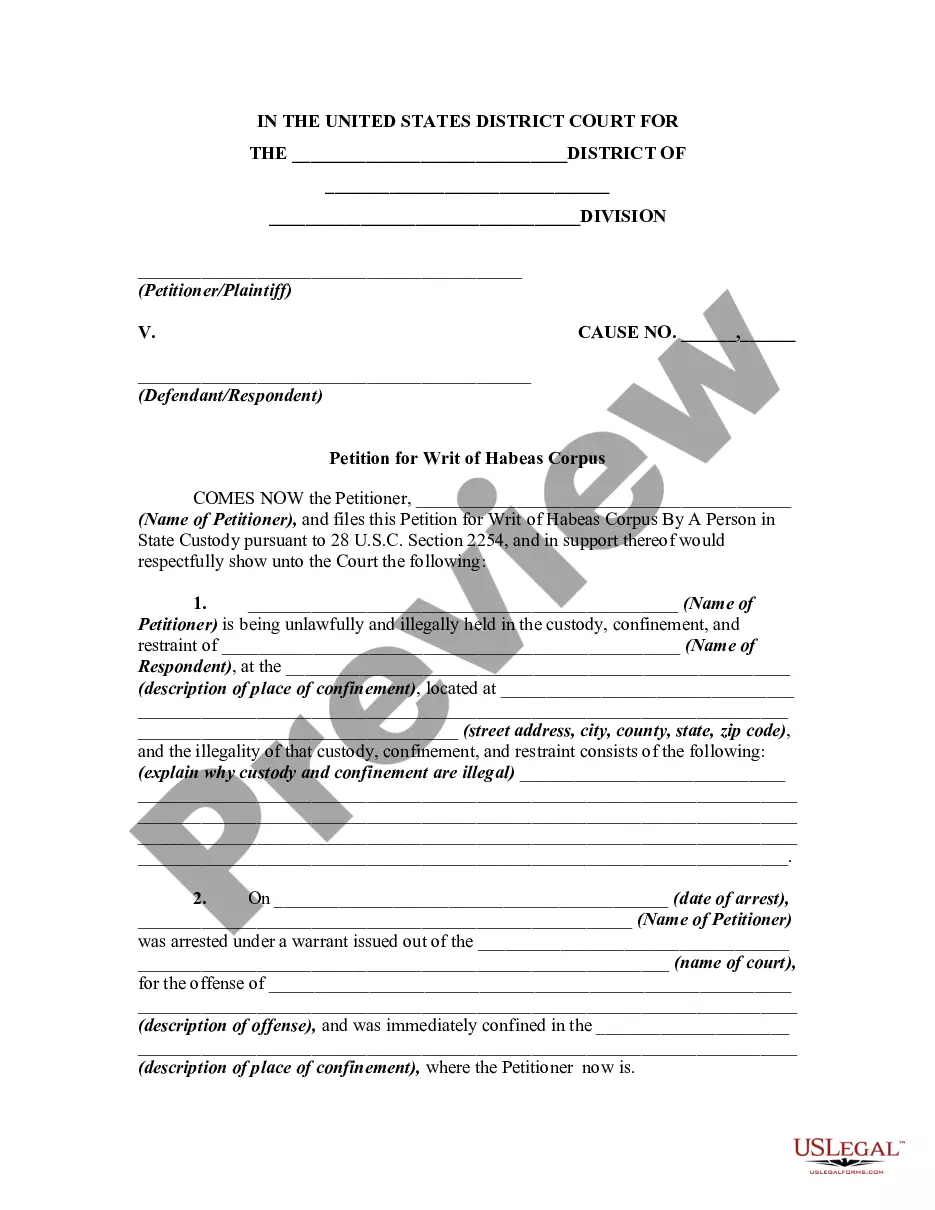
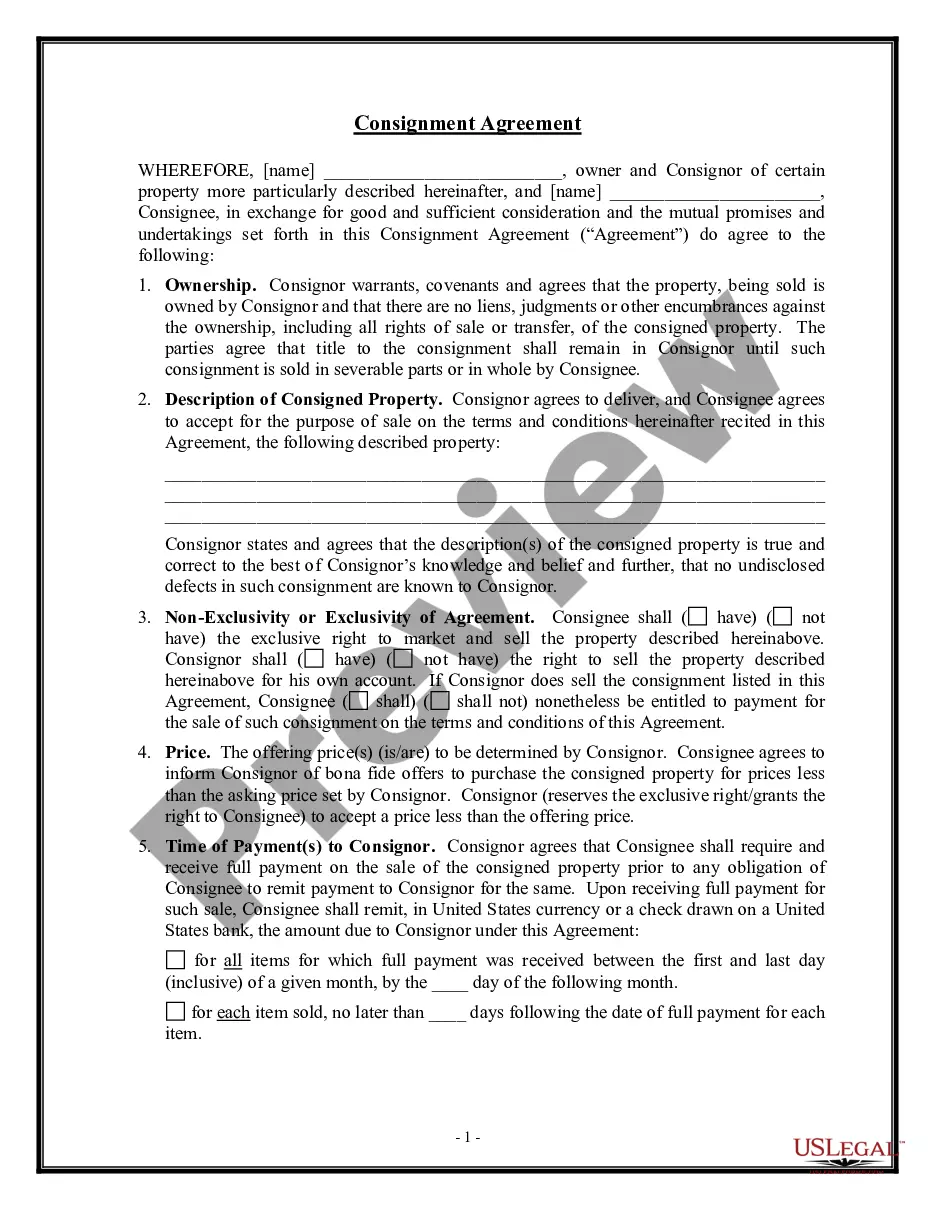
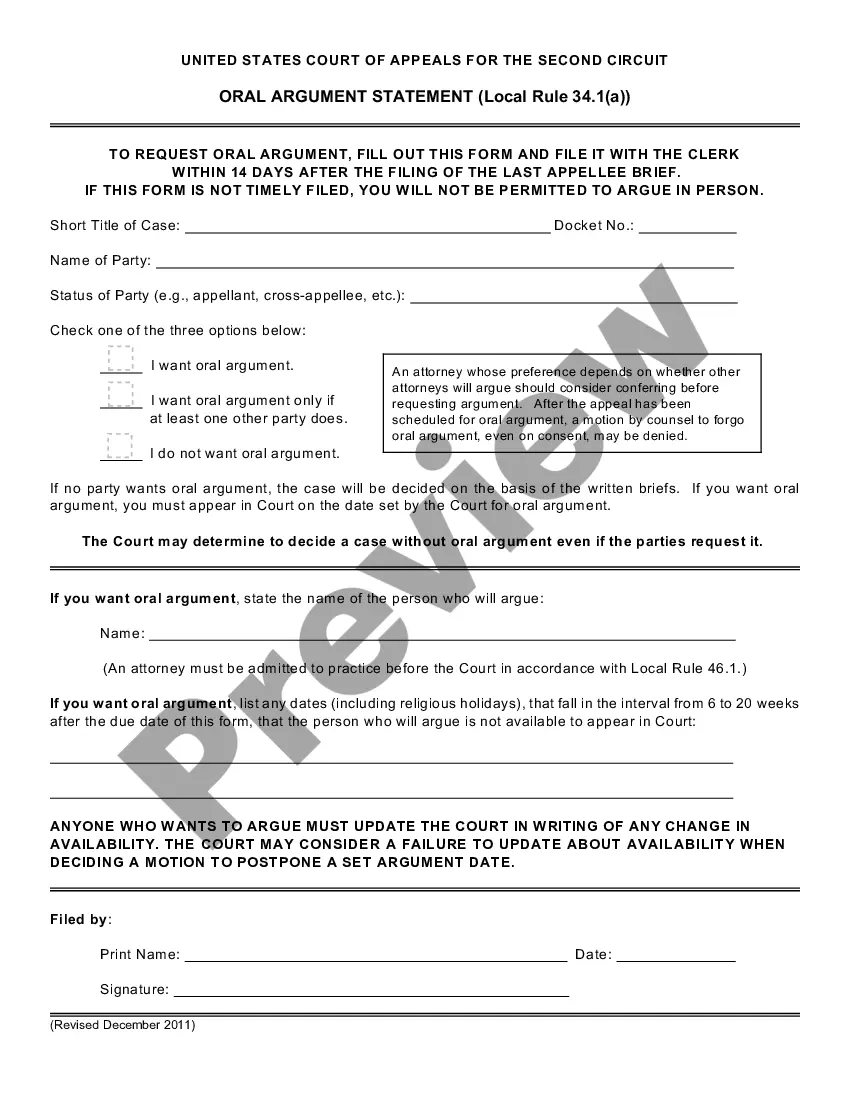
A request for review must be made within 180 days after the claim payment date or the date of the notification of denial of benefits. You may submit an appeal by phone or in writing. You should state the reason why you believe the claim determination or precertification improperly reduced or denied your benefits.
How do I dispute a claim? Empire BlueCross BlueShield HealthPlus New York Claims, P.O. Box 61010 Virginia Beach, VA 23466-1010.
Insurance: Anthem BCBS (formerly known as Empire Blue Cross Blue Shield BCBS) - NYC Health + Hospitals.
Find Your Local BCBS Company On their website, you'll be able to look up your health plan, review a claim and more. Enter the first three letters of the Identification Number from your member ID card. If you receive insurance through an employer, please enter the ZIP Code.
BCBS is a federation of 36 independent health insurance companies, each serving specific states or regions. While BCBS-affiliated insurers offer health plans nationwide, the details of coverage, including plan types, premiums, and benefits, can differ by state due to local regulations and market conditions.
Level 1 Appeal – call or write to Anthem to appeal the coverage decision Level 2 Appeal - conducted by an Independent Review Entity . This organization decides whether the decision we made should be changed.
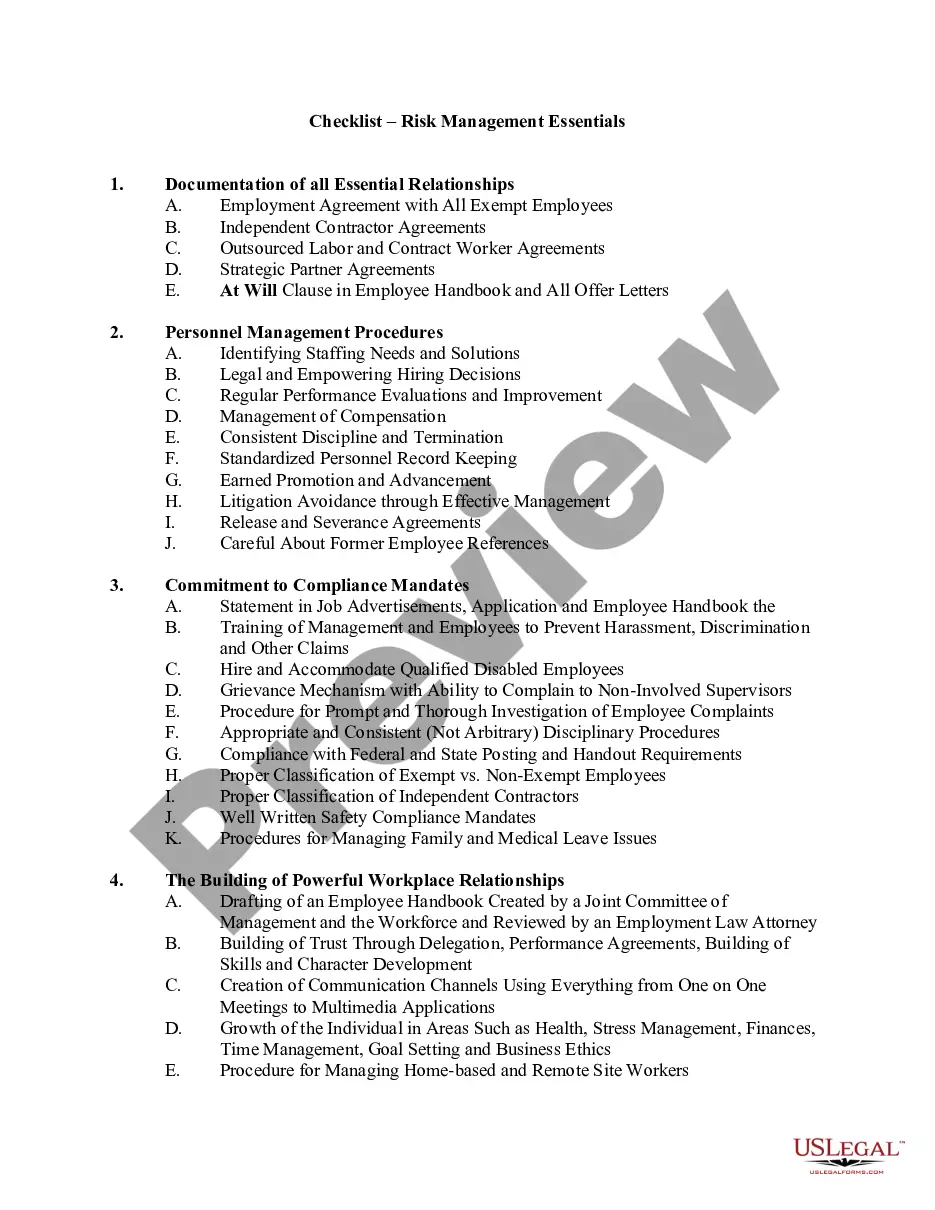
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.