Anthem Claim Dispute Form With Email In Montgomery
Description
Form popularity
FAQ
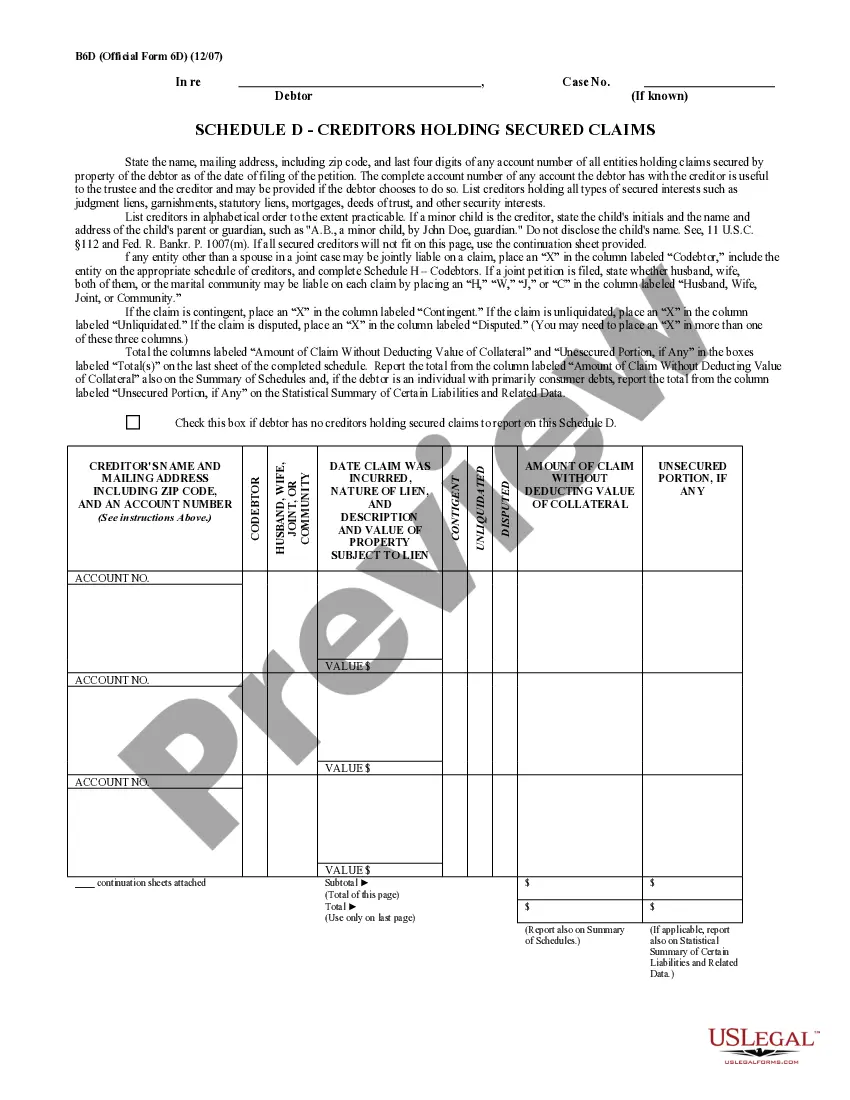
180-day timely filing limit.
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.
-Timely filing is within 180 days of the date of service or per the terms of the provider agreement. Out-of-state and emergency transportation providers have 365 days from the last date of service.
How to Find Timely Filing Limits With Insurance Insurance CompanyTimely Filing Limit (From the date of service) Anthem BCBS Ohio, Kentucky, Indiana, Wisconsin 90 Days Wellmark BCBS Iowa and South Dakota 180 Days BCBS Alabama 2 Years BCBS Arkansas 180 Days28 more rows
Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
Anthem will consider reimbursement for the initial claim, when received and accepted within timely filing requirements, in compliance with federal, and/or state mandates. Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
Please fax to 1-855-516-1083. You may ask us to rush your appeal if your health needs it. We'll let you know we got your appeal within 24 hours from the time we received it.
1) Sign on using your own login and password. 2) Once in Availity, select the State you're contracted in from the top task bar. 3) Choose Claims and Payments from the task bar and then Claims and Encounters. 4) Select Professional Claim for 1500 claim submission and choose the appropriate Payer.
To use the Appeals application, the Availity administrator must assign the Claim Status role for the user. The Disputes and Appeals functionality will support Appeals, Reconsiderations and Rework requests for providers. The Disputes and Appeals functionality is accessible from the Claim Status transaction.