Erisa Law Explained In Houston
Description
Form popularity
FAQ
ERISA requirements apply to all employer-based health plans, whether fully insured through a third party or self-funded. But, governmental plans offered by local, state, or federal governments are generally excepted from ERISA requirements.
Employers offering an employee welfare benefit plan, such as health insurance or a retirement plan, are subject to the provisions of the the Employee Retirement Income Security Act (ERISA). ERISA is a federal law that covers administrative aspects of employee benefit and retirement plans.
ERISA governs the claim only if ERISA covers the plan involved in the claim. ERISA applies to most employee benefit plans, including employee health and retirement plans. ERISA does not cover certain plans, such as government plans and church plans.
An ERISA lawsuit offers individuals the opportunity to recover various types of damages, including medical bills, lost wages, and pension benefits.
An ERISA claim refers to a legal action taken under the Employee Retirement Income Security Act (ERISA) of 1974. This law protects employees' rights to their benefits, such as retirement and health plans, ensuring fair treatment by employers.
An ERISA fidelity bond is a type of insurance that protects the plan against losses caused by acts of fraud or dishonesty. Fraud or dishonesty includes, but is not limited to, larceny, theft, embezzlement, forgery, misappropriation, wrongful abstraction, wrongful conversion, willful misapplication, and other acts.
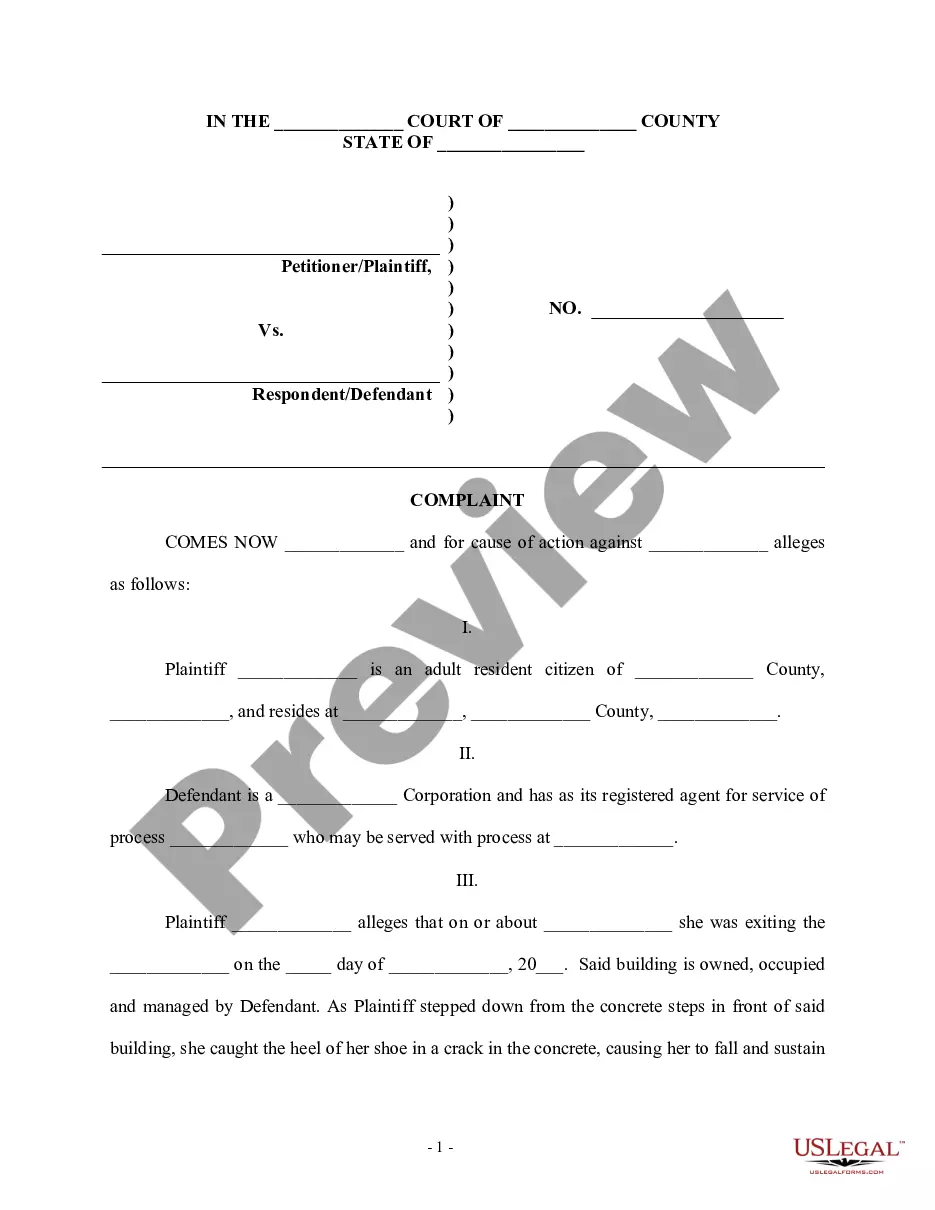
Types of ERISA Claims Consider the following examples, which is not exhaustive: An employee who has a long-term disability plan that provides benefits if she is totally disabled. After suffering a serious fall at work, the employee struggles with a traumatic brain injury and other impairments.
ERISA requires plans to provide participants with plan information including important information about plan features and funding; sets minimum standards for participation, vesting, benefit accrual and funding; provides fiduciary responsibilities for those who manage and control plan assets; requires plans to ...
The plan document should contain: Name of the plan administrator. Designation of any named fiduciaries other than the plan administrator under the claims procedure for deciding benefit appeals. A description of the benefits provided. The standard of review for benefit decisions.
ERISA prohibits certain transactions between an employee benefit plan and "parties in interest," which include the employer and others who may be in a position to exercise improper influence over the plan, and such transactions may trigger civil monetary penalties under Title I of ERISA.