Tranfer Conveys Death With Dignity
Description
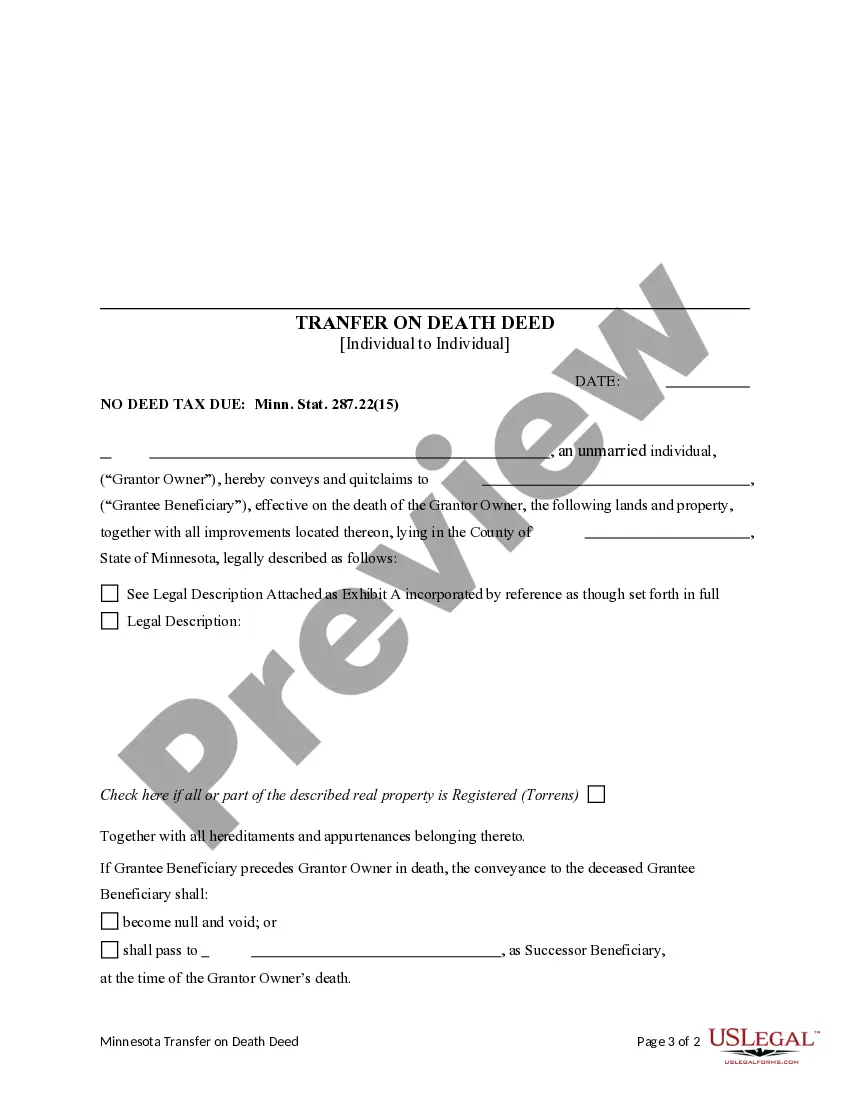
How to fill out Minnesota Transfer On Death Deed - Individual To Individual?
The Transfer Communicates Death With Honor you observe on this webpage is a reusable official template created by experienced attorneys in accordance with federal and local laws.
For over 25 years, US Legal Forms has supplied individuals, businesses, and legal practitioners with more than 85,000 validated, state-specific documents for any commercial and personal circumstance. It’s the fastest, most direct and most dependable method to acquire the paperwork you require, as the service ensures the utmost level of data protection and anti-virus security.
Subscribe to US Legal Forms to have authenticated legal templates for all of life’s circumstances readily available.
- Search for the document you require and review it.
- Browse through the file you searched and preview it or examine the form description to confirm it meets your needs. If it doesn’t, utilize the search bar to locate the suitable one. Click Buy Now once you have found the template you need.
- Choose and Log In.
- Select the pricing plan that fits you and create an account. Use PayPal or a credit card for a swift payment. If you already possess an account, Log In and verify your subscription to proceed.
- Retrieve the editable template.
- Select the format you prefer for your Transfer Communicates Death With Honor (PDF, DOCX, RTF) and download the example onto your device.
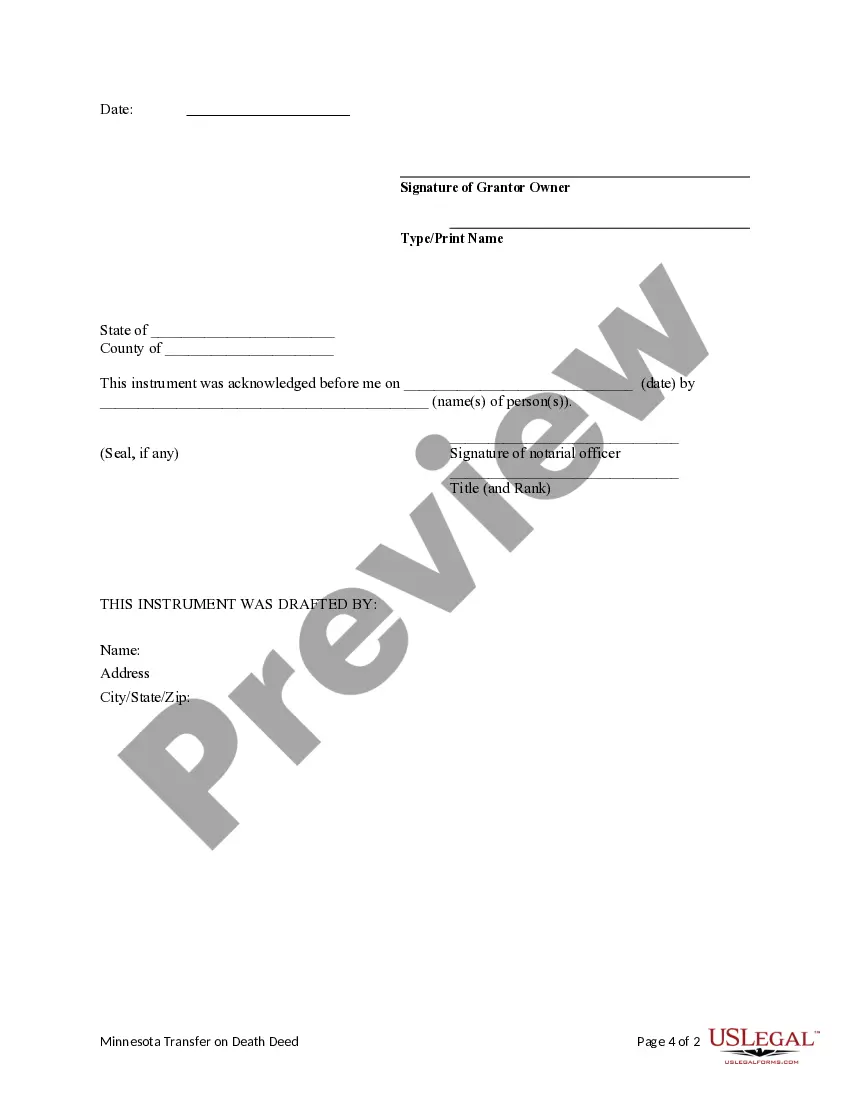
- Fill out and sign the document.
- Print the template to complete it manually. Alternatively, employ an online versatile PDF editor to swiftly and accurately fill out and sign your form with a valid signature.
- Download your documents again.
- Utilize the same form again whenever needed. Access the My documents tab in your profile to redownload any previously downloaded forms.
Form popularity
FAQ
Oregon has not eliminated the residency requirement for accessing medically assisted deaths; it remains a state-specific provision. Residents must establish their status to secure the legal protections and processes available for death with dignity. Understanding how transfer conveys death with dignity within Oregon's framework is essential for those considering this option.
These laws are commonly referred to as aid-in-dying laws, voluntary-assisted dying laws, and physician-assisted dying laws. In a nutshell, death with dignity laws allow mentally competent people with a confirmed terminal illness to request and receive a prescription for a lethal medication that will hasten their death.
Passive euthanasia: intentionally letting a patient die by withholding artificial life support such as a ventilator or feeding tube. Some ethicists distinguish between withholding life support and withdrawing life support (the patient is on life support but then removed from it).
To requesta prescription for lethal medications, the DWDA requires that a patient must be: ? an adult (18 years of age or older), ? a resident of Oregon, ? capable (defined as able to make and communicate health care decisions), and ? diagnosed with a terminal illness that will lead to death within six months.
There is only one death with dignity. Comprehensive symptom control, optimal quality of life, ability to engage in enjoyable activities, capacity and desire for independent functioning. Palliative care teams should be involved to provide holistic care for the patient.
If present during medical aid in dying, the nurse promotes patient dignity as well as provides for symptom relief, comfort, and emotional support to the patient and family. The nurse must maintain patient confidentiality and privacy in the aid in dying process.