Florida Blue Appeal Process
Description
How to fill out Florida Writ Of Certiorari And Appeal Of License Suspension?
Obtaining a reliable resource to access the latest and suitable legal documents is a significant part of navigating bureaucratic processes.
Identifying the appropriate legal document necessitates accuracy and careful consideration, which is why it's essential to source samples of the Florida Blue Appeal Process exclusively from credible providers, such as US Legal Forms. An incorrect template can squander your time and hinder your progress.
After obtaining the form on your device, you may edit it with the editor or print it out to fill it out by hand. Eliminate the stress associated with your legal documentation. Browse through the extensive US Legal Forms catalog to find legal templates, assess their relevance to your situation, and download them instantly.
- Utilize the library navigation or the search function to find your document.
- Review the description of the form to confirm that it meets the requirements of your region and state.
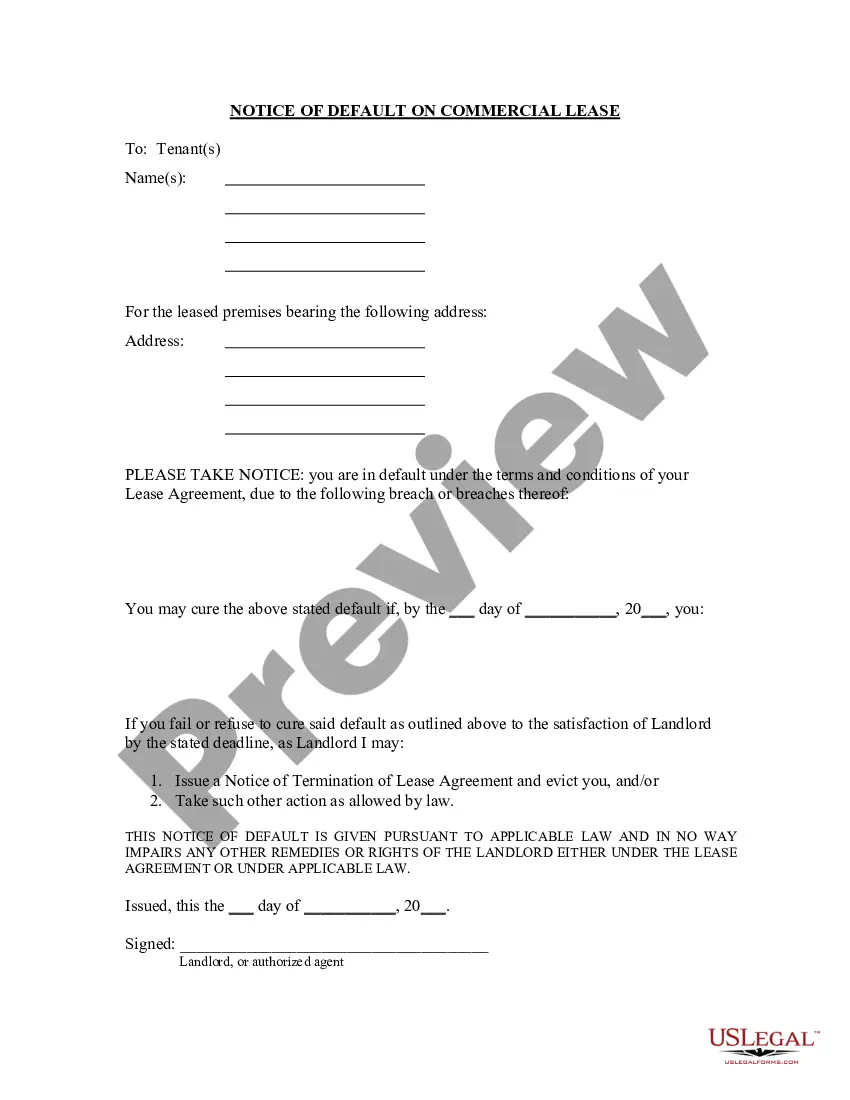
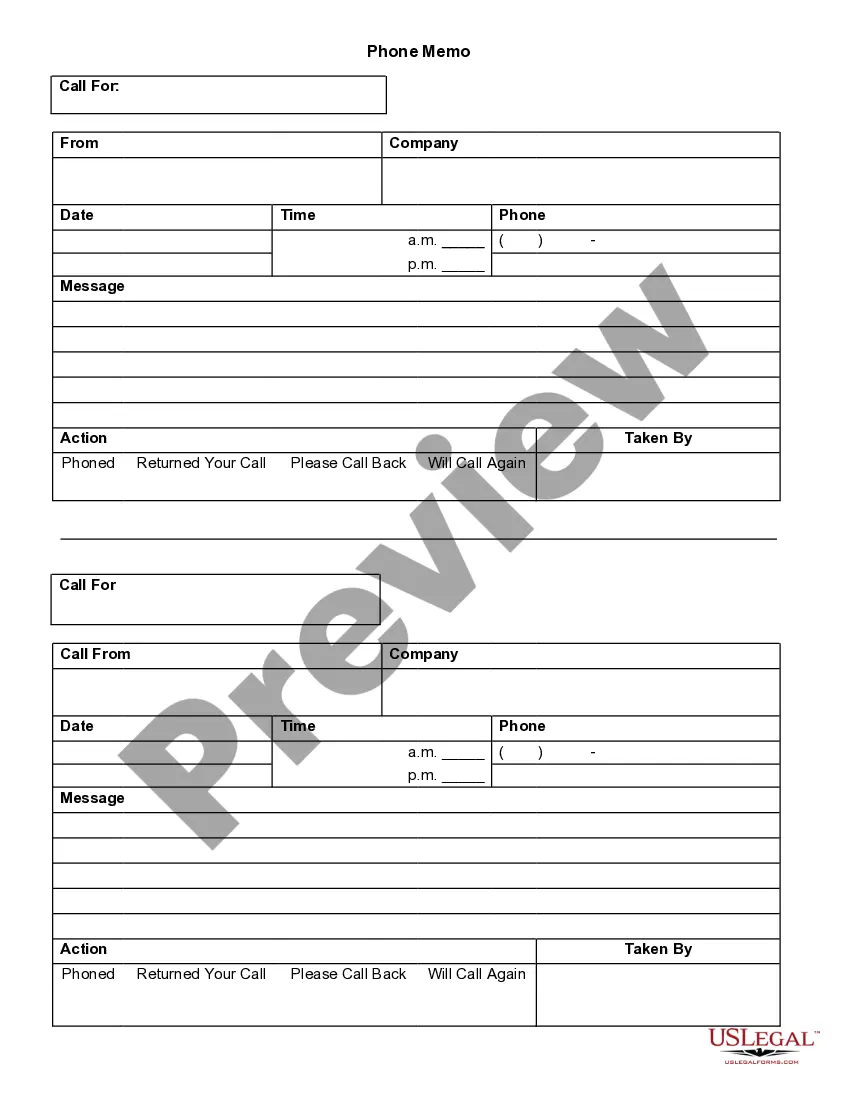
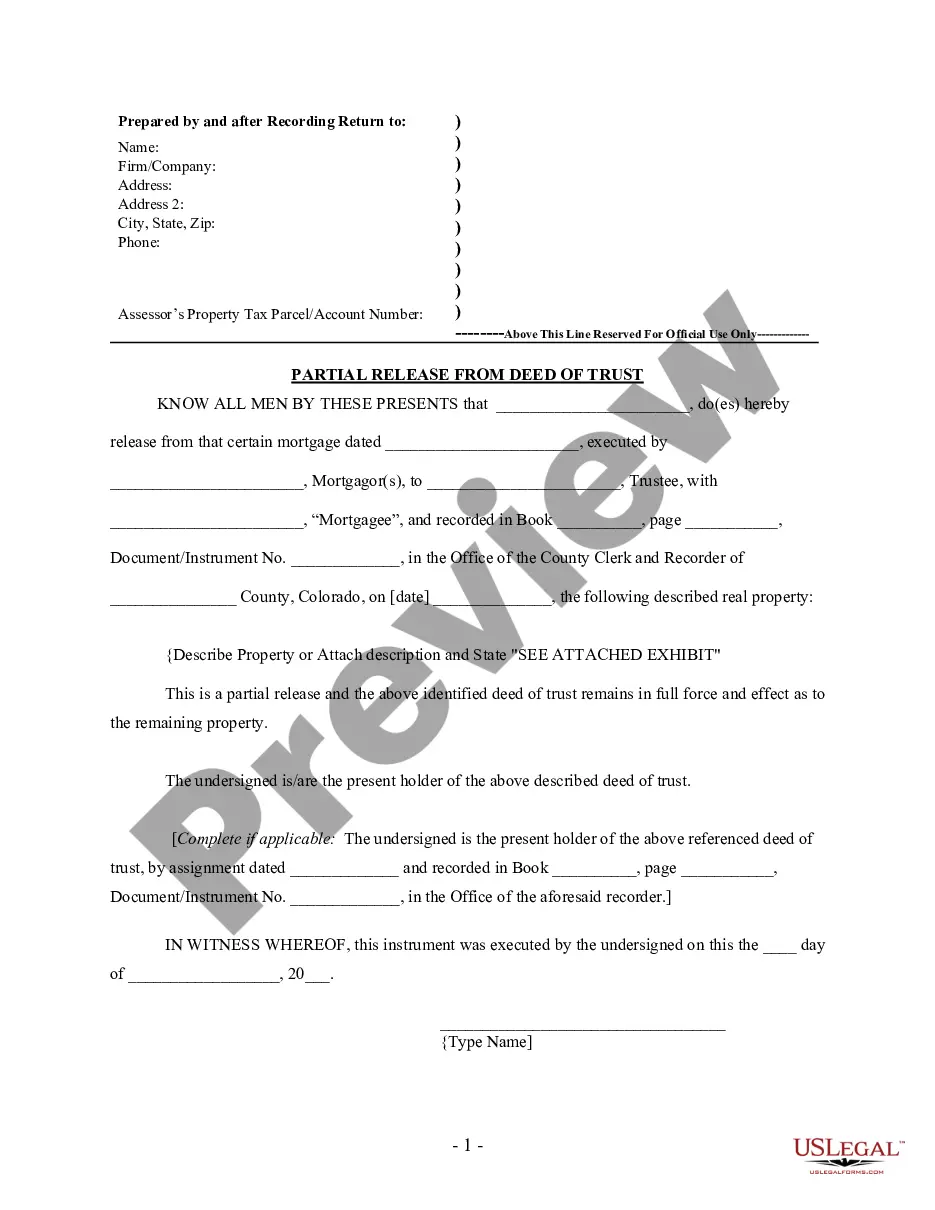
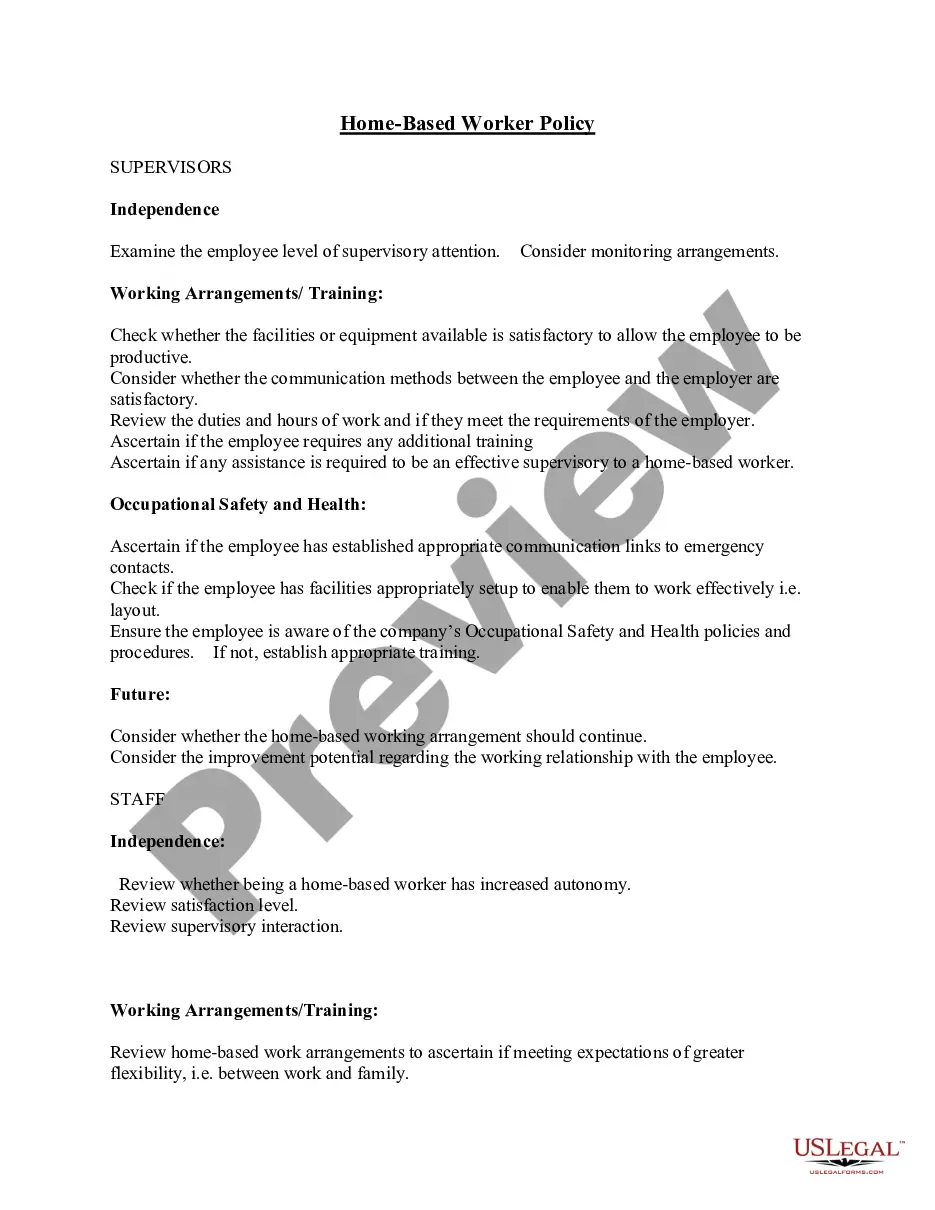
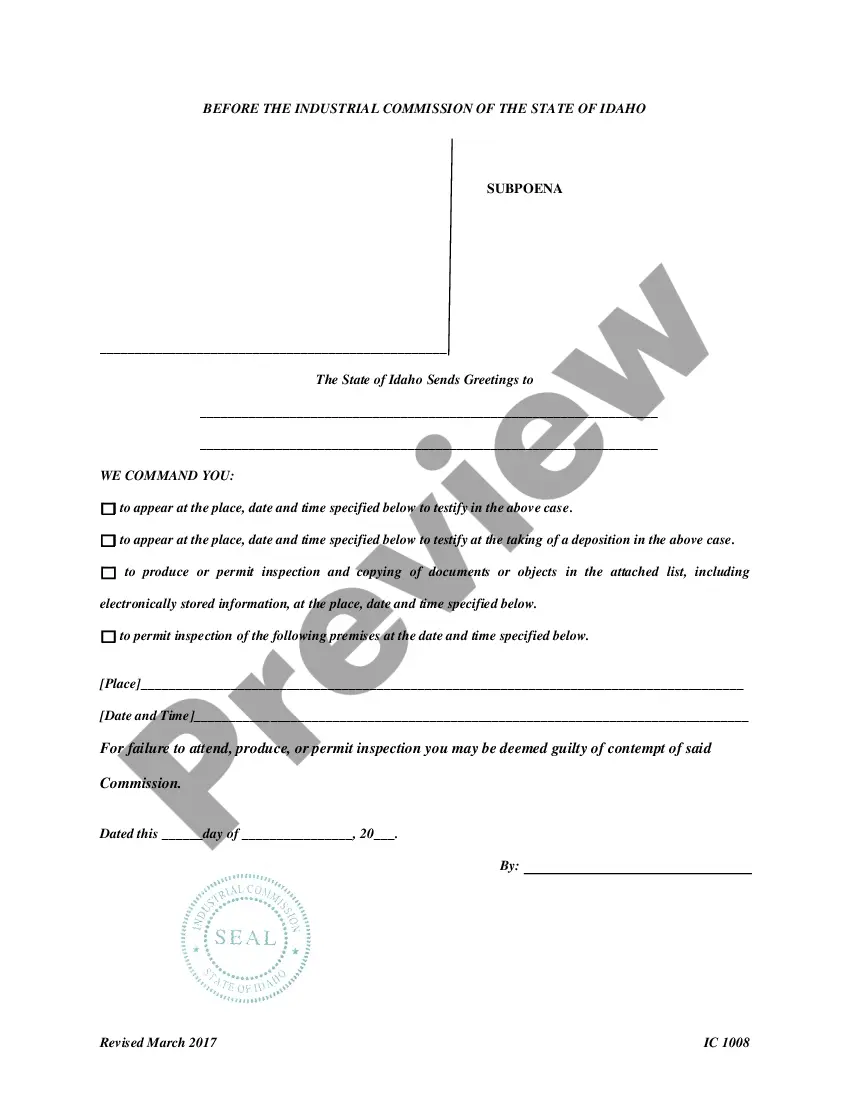
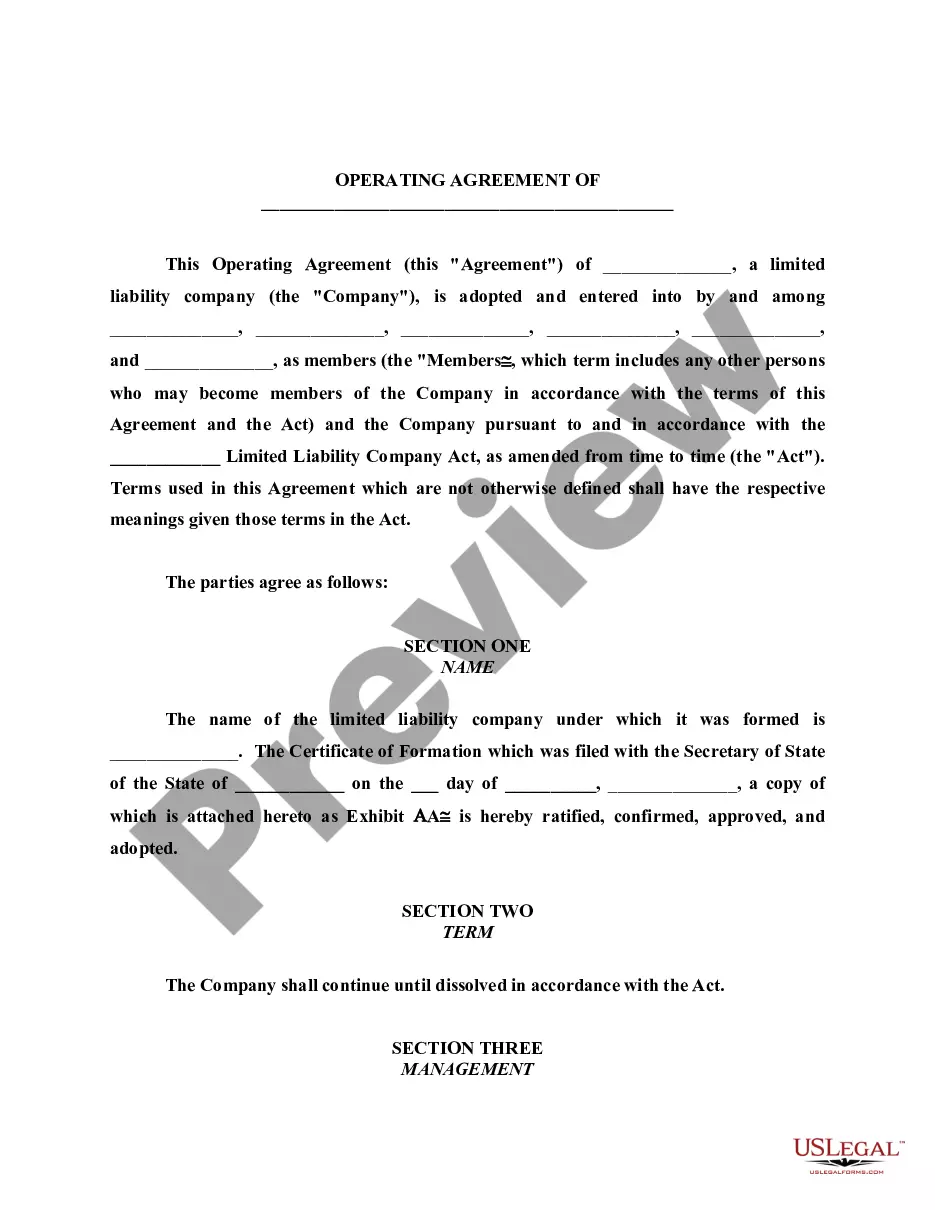
- Access the form preview, if available, to ensure the template is indeed what you need.
- Return to the search to find the appropriate template if the Florida Blue Appeal Process does not fulfill your needs.
- Once you are certain about the document’s applicability, download it.
- If you are a registered user, click Log in to verify your identity and access your chosen templates in My documents.
- If you haven’t created an account yet, click Buy now to acquire the form.
- Select the pricing plan that suits your needs.
- Proceed to the registration to finalize your purchase.
- Complete your order by selecting a payment option (credit card or PayPal).
- Choose the document format for downloading the Florida Blue Appeal Process.
Form popularity
FAQ
This External Review Form must be filed with Florida Blue's Member Appeals Department within four (4) months after receipt of your final adverse benefit determination regarding coverage of a health care service or treatment.
Select Claims from the left-hand navigation menu. Select Appeal Claim from the left-hand navigation menu, and then Go to Availity. If you are navigating to the claims submission tool from .Availity.com: Click on Log in and enter your Availity ID and password.
This External Review Form must be filed with Florida Blue's Member Appeals Department within four (4) months after receipt of your final adverse benefit determination regarding coverage of a health care service or treatment.
If you have questions about accessing the Electronic Appeal tool please call 1-800-Availity or 1-800-282-4548.
You must file your internal appeal within 180 days (6 months) of receiving notice that your claim was denied.