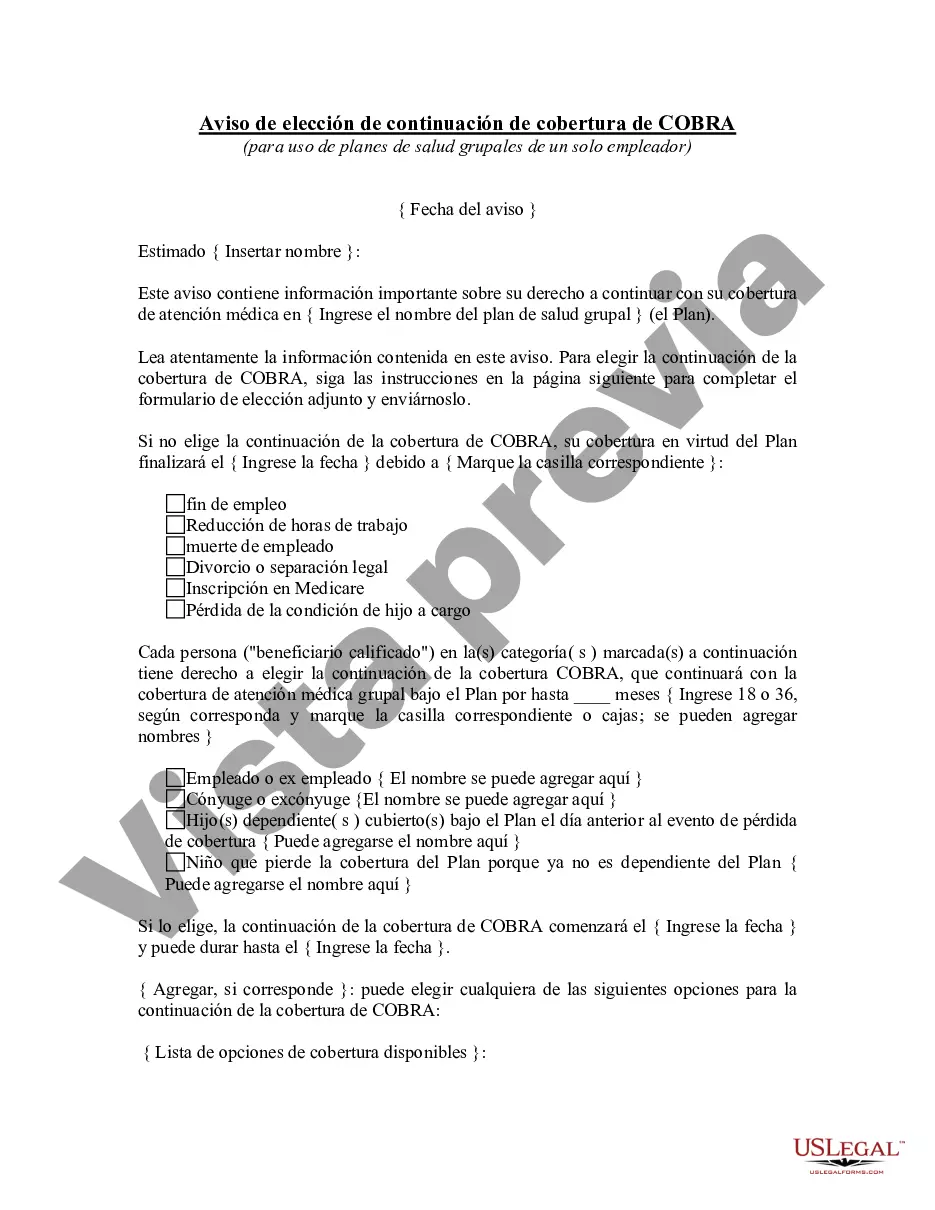
Mesa Arizona Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
State:
Multi-State
City:
Mesa
Control #:
US-323EM
Format:
Word
Instant download
Description
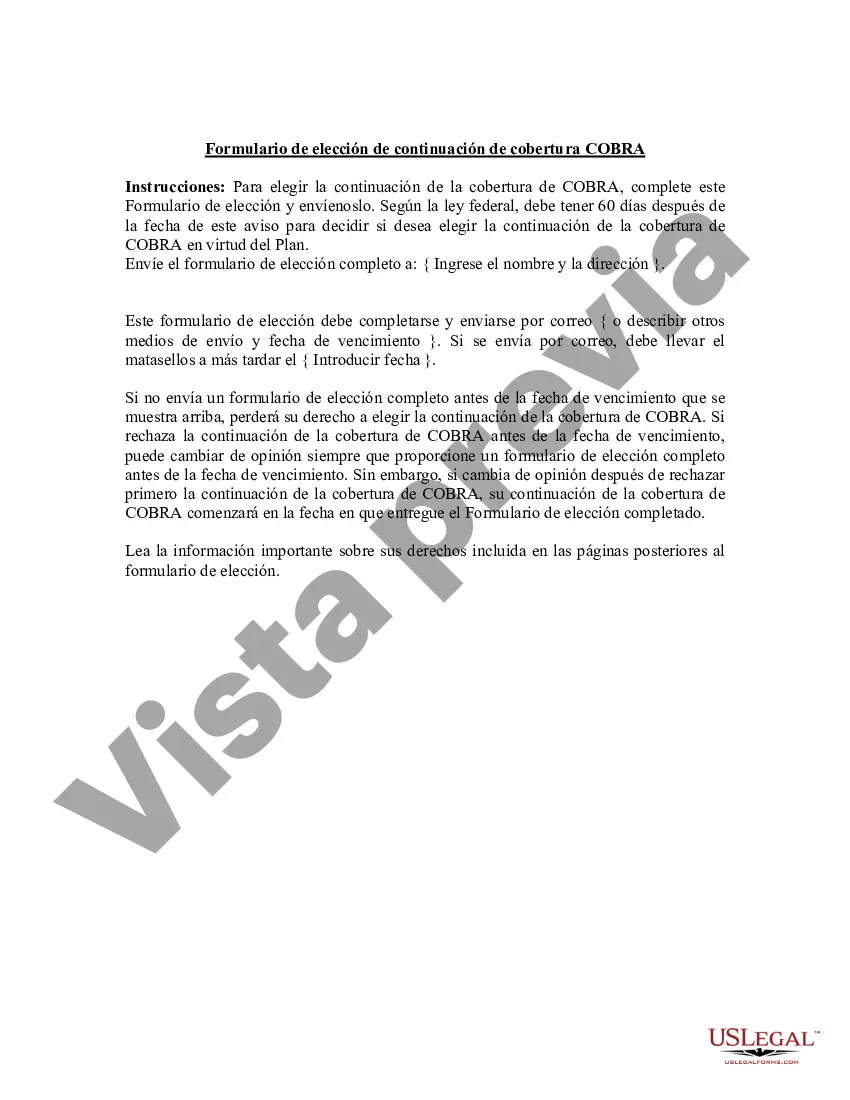
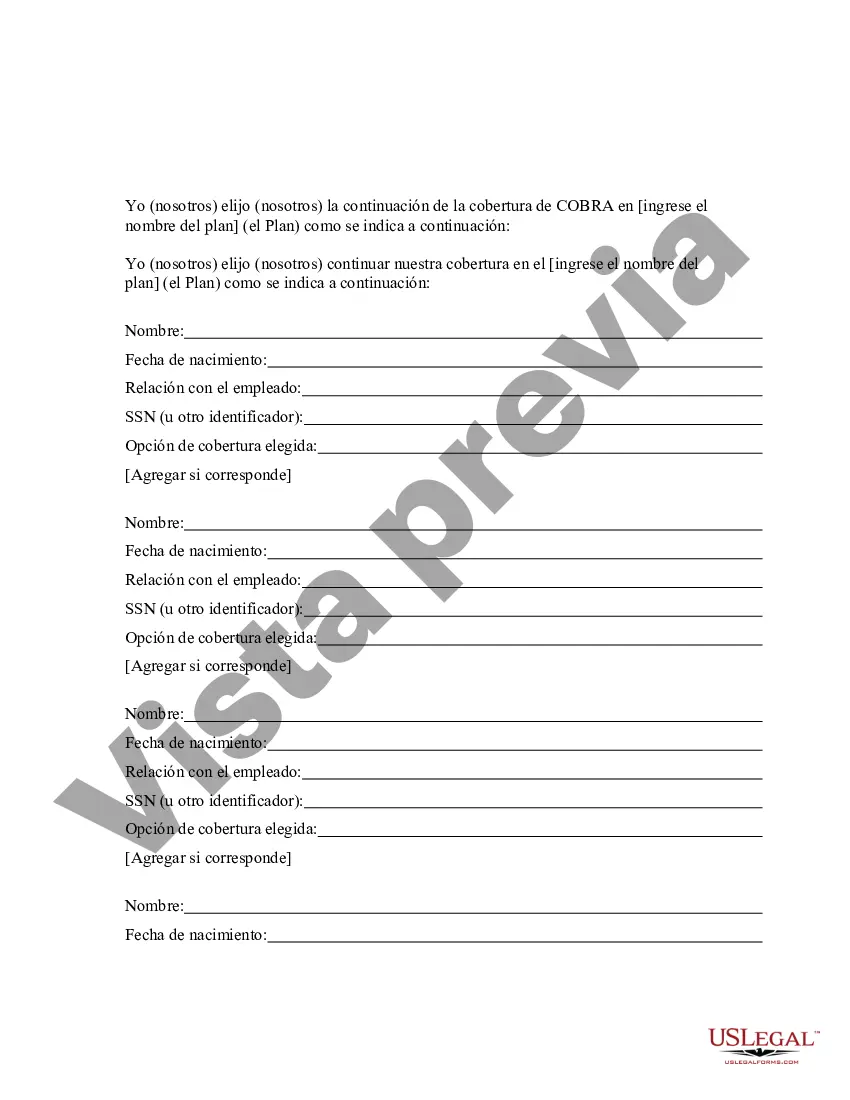
Este aviso contiene información importante sobre el derecho de una persona a continuar con la cobertura de atención médica bajo COBRA.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés.
For your convenience, the complete English version of this form is attached below the Spanish version.
Free preview