Anthem Claim Dispute Form With Provider In Washington
Description
Form popularity
FAQ
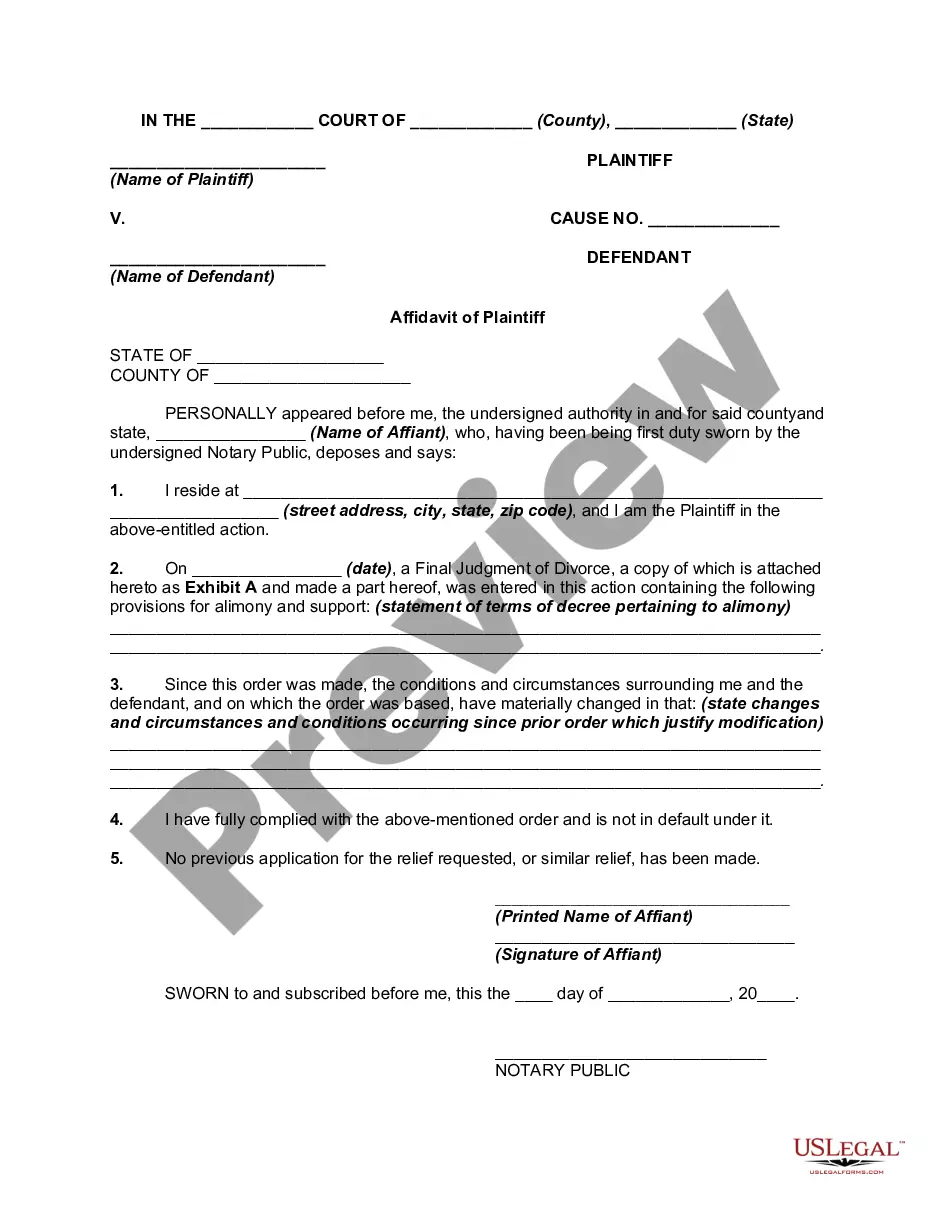
Members have up to 180 calendar days from the date of an incident or dispute, or from the date the member receives a denial letter, to submit a grievance or appeal to Anthem Blue Cross.
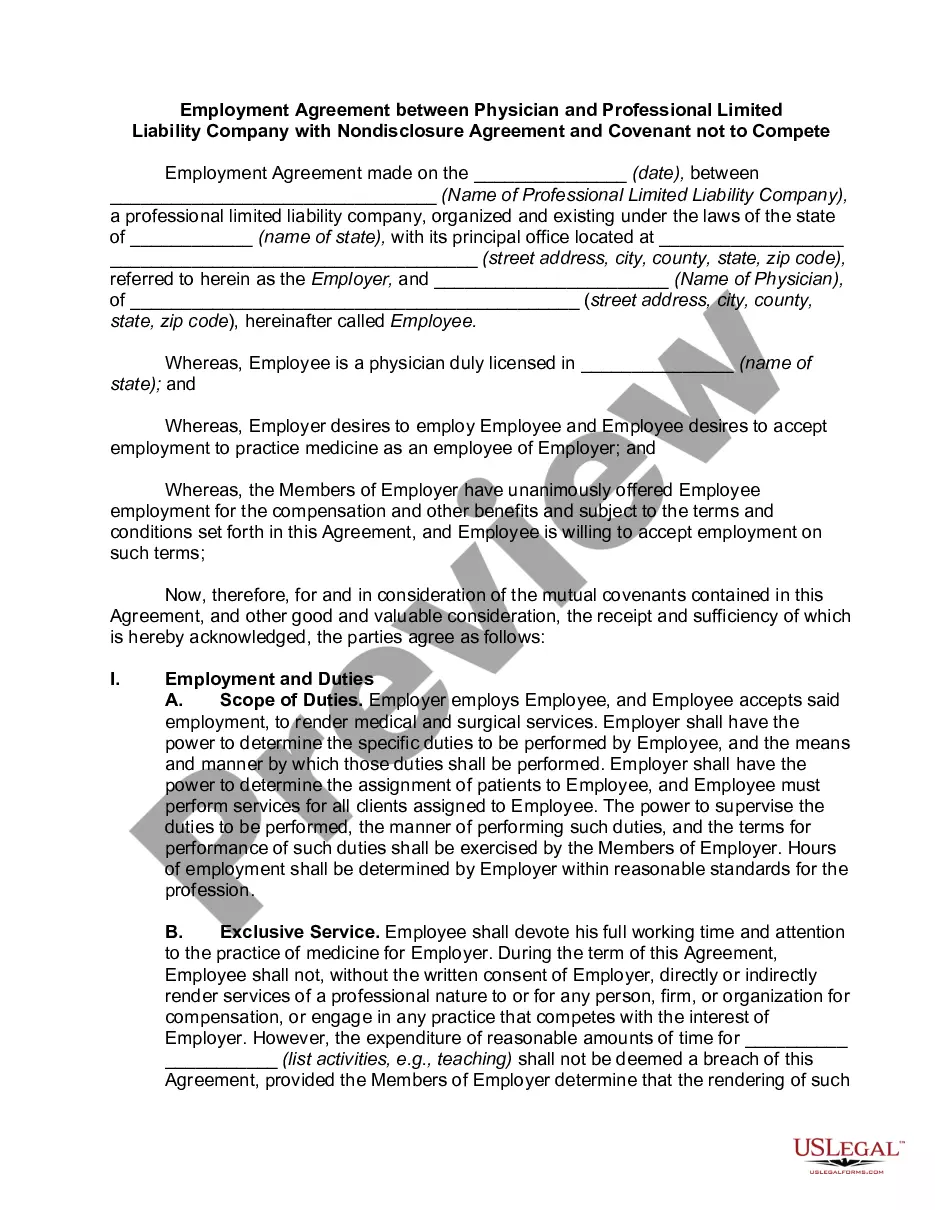
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.
Non-participating providers: Call the number on the back of the member's ID card or call 800-676-BLUE (2583) to reach Provider Services. You can also use chat or secure messaging directly in Availity.
Important Note: You must submit your appeal within 180 days of the date on the Adverse Benefit Determination or denial letter.
Form 1095-A It is typically sent by January 31st for the previous tax year. The form contains important details about the coverage, including the dates of coverage, the amount of the monthly premium, and the amount of any advance premium tax credit received.
Premera Blue Cross is a not-for-profit healthcare company that offers health plans in Washington state and Alaska. Driven by a mission to serve our customers and their communities, Premera has donated millions to local nonprofits since 2017.
Anthem will consider reimbursement for the initial claim, when received and accepted within timely filing requirements, in compliance with federal, and/or state mandates. Anthem follows the standard of: • 90 days for participating providers and facilities. 15 months for nonparticipating providers and facilities.
Premera Blue Cross | Washington State Health Care Authority.
Even though we will no longer offer Medicare Advantage plans in 2025, Premera isn't leaving the senior market entirely. We'll continue to offer Medicare Supplement plans, serving more than 58,000 members in Washington and Alaska.