Anthem Claim Dispute Form With 2 Points In Virginia
Description
Form popularity
FAQ
Please fax to 1-855-516-1083. You may ask us to rush your appeal if your health needs it. We'll let you know we got your appeal within 24 hours from the time we received it.
One redetermination form can be submitted for multiple claims only for denials by the Unified Program Integrity Contractor or Medical Review probe reviews. Fax request to 1-888-541-3829.
You can also fax to 855-516-1083. Please be sure to mark "EXPEDITED" on the form before faxing.
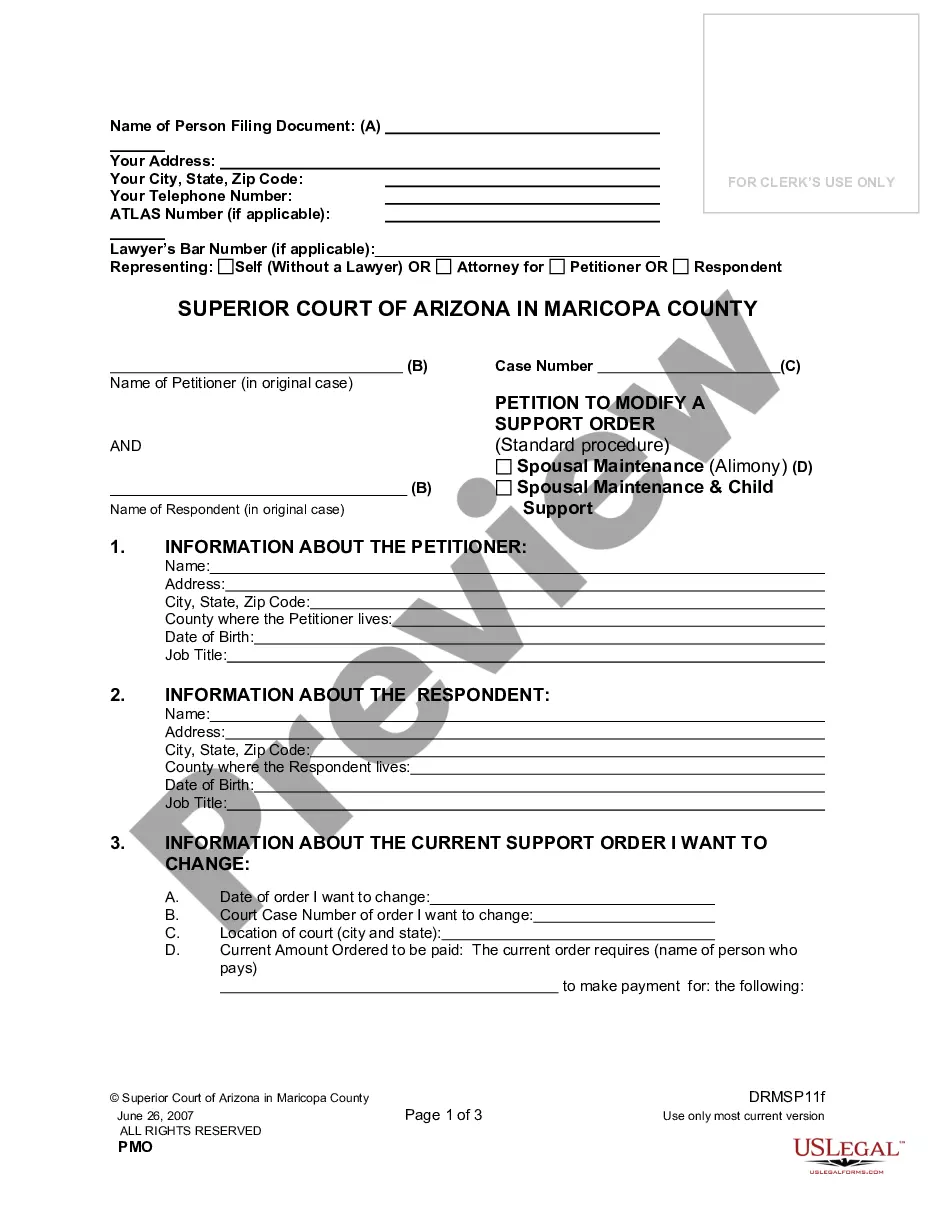
Anthem follows the standard of: • 90 days for participating providers and facilities. 180 days for nonparticipating providers and facilities (For dates of service prior to January 1, 2019, 12 months for nonparticipating providers).
File the appeal within ten (10) days from the date your "Determination of Eligibility" was sent by one of these methods: Mail the appeal to 10 North Senate Avenue, Indianapolis, IN 46204; Fax the appeal to (317) 233-6888; Deliver the appeal in person to the Department at 10 N.
After you fill out the form, Mail/Fax/deliver your request for a hearing within 33 days of the date of the notice you are appealing. Mail: FSSA Document Center PO Box 1810 Marion, Indiana 46952 Fax: 1-800-403-0864 Visit your local DFR/Medicaid Office.
TIMELY FILING The Medical Assistance Program regulations require the prompt submission of all claims. Virginia Medicaid is mandated by federal regulations 42 CFR § 447.45(d) to require the initial submission of all claims (including accident cases) within 12 months from the date of service.
Corrected claims must be received within 12 months of Explanation of Payment (EOP). Appeal deadlines: Claim payment reconsideration must be filed within 12 months of the EOP. Claim payment appeals must be filed within 15 months of service or 180 days from the reconsideration decision.
Corrected claims and appeals have shorter deadlines, typically within 60-180 days of denial or payment.